Sunday Poster Session
Category: Infections and Microbiome
P1361 - Double Trouble: Unmasking Parasitic Colitis Mimicking Inflammatory Bowel Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- KM
Kranthi Mandava, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Kranthi Mandava, MD1, Joshua E. Pagán-Busigó, MD2, Ethan Shamsian, DO1, Michael Bebawy, DO1, Mohamed Ismail, DO1, Menna-Allah Elaskandrany, DO3, Ahmed Al-Khazraji, MD1
1Rutgers New Jersey Medical School, Newark, NJ; 2Rutgers New Jersey Medical School, Kearny, NJ; 3Lenox Hill Hospital, Northwell Health, New York City, NY
Introduction: Cirrhotic patients often develop immune dysfunction, increasing their susceptibility to infections. Parasitic infections such as schistosomiasis and rarely strongyloidiasis can resemble inflammatory bowel disease (IBD), complicating diagnosis. Hepatic schistosomiasis, in particular, can cause periportal fibrosis and worsen cirrhosis through portal hypertension. In those with pre-existing cirrhosis, this can further impair liver function. We present a case of a double parasitic infection in a male with suspected AIH-related decompensated cirrhosis, whose presentation mimicked IBD.
Case Description/
Methods: A 27-year-old Egyptian male with a history of cirrhosis, initially attributed to autoimmune hepatitis (AIH), presented with persistent abdominal pain and several days of bloody diarrhea. He was diagnosed with AIH in 2016 (ANA/ASMA +, IgG level >3000) and cirrhosis in Egypt in 2022 after developing ascites, hemorrhoids, and GI bleeding. On admission, labs showed elevated liver enzymes (ALT 61 U/L, AST 80 U/L, ALP 376 U/L), hypoalbuminemia (2.4 g/dL), and iron deficiency anemia (Hgb 9.9 g/dL, MCV 68.5 fL, ferritin 12 ng/mL); eosinophil counts were normal. EGD revealed grade 1 esophageal varices. Colonoscopy showed strictures in the transverse colon, ulcers (including one within a stricture), and friable mucosa extending to the cecum. A history of oral ulcers raised concern for IBD. However, biopsies revealed chronic active eosinophilic colitis with crypt distortion and up to 80 eosinophils/HPF, and IBD testing was negative. Given a history of freshwater exposure in a schistosomiasis-endemic region, parasitic infection was suspected. Stool and serologic testing confirmed schistosomiasis and strongyloidiasis. He was treated with albendazole, praziquantel, and steroids, and showed marked improvement. Follow-up endoscopy and colonoscopy were later scheduled.
Discussion: This case of a young cirrhotic male with transverse colonic strictures and ulcerations due to coexisting schistosomiasis and strongyloidiasis highlights several challenges in the management of cirrhosis complicated by parasitic colitis. Initially, the unusual transverse colon involvement, history of the oral ulcer and lack of eosinophilia mimicked IBD. Despite absent eosinophilia, serology testing and biopsy-confirmed diagnosis prevented mismanagement and treatment with albendazole and praziquantel led to significant improvement, underscoring the need for early recognition and appropriate therapy.
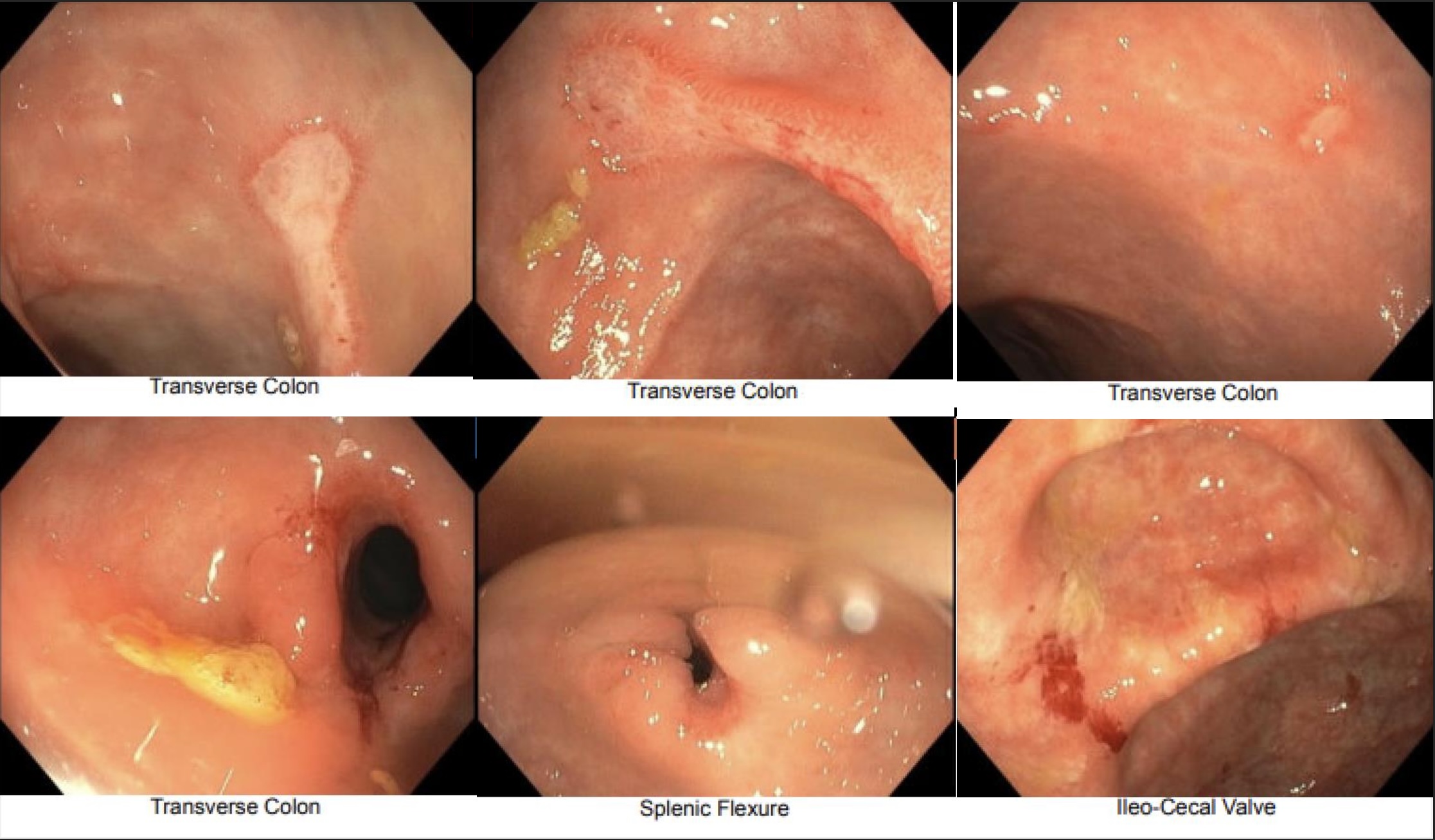
Figure: Images of the transverse colon reveal stricture and ulcerating disease. Stricture also present in splenic flexure, as well as a friable ileo-cecal valve.
Disclosures:
Kranthi Mandava indicated no relevant financial relationships.
Joshua Pagán-Busigó indicated no relevant financial relationships.
Ethan Shamsian indicated no relevant financial relationships.
Michael Bebawy indicated no relevant financial relationships.
Mohamed Ismail indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Kranthi Mandava, MD1, Joshua E. Pagán-Busigó, MD2, Ethan Shamsian, DO1, Michael Bebawy, DO1, Mohamed Ismail, DO1, Menna-Allah Elaskandrany, DO3, Ahmed Al-Khazraji, MD1. P1361 - Double Trouble: Unmasking Parasitic Colitis Mimicking Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Rutgers New Jersey Medical School, Kearny, NJ; 3Lenox Hill Hospital, Northwell Health, New York City, NY
Introduction: Cirrhotic patients often develop immune dysfunction, increasing their susceptibility to infections. Parasitic infections such as schistosomiasis and rarely strongyloidiasis can resemble inflammatory bowel disease (IBD), complicating diagnosis. Hepatic schistosomiasis, in particular, can cause periportal fibrosis and worsen cirrhosis through portal hypertension. In those with pre-existing cirrhosis, this can further impair liver function. We present a case of a double parasitic infection in a male with suspected AIH-related decompensated cirrhosis, whose presentation mimicked IBD.
Case Description/
Methods: A 27-year-old Egyptian male with a history of cirrhosis, initially attributed to autoimmune hepatitis (AIH), presented with persistent abdominal pain and several days of bloody diarrhea. He was diagnosed with AIH in 2016 (ANA/ASMA +, IgG level >3000) and cirrhosis in Egypt in 2022 after developing ascites, hemorrhoids, and GI bleeding. On admission, labs showed elevated liver enzymes (ALT 61 U/L, AST 80 U/L, ALP 376 U/L), hypoalbuminemia (2.4 g/dL), and iron deficiency anemia (Hgb 9.9 g/dL, MCV 68.5 fL, ferritin 12 ng/mL); eosinophil counts were normal. EGD revealed grade 1 esophageal varices. Colonoscopy showed strictures in the transverse colon, ulcers (including one within a stricture), and friable mucosa extending to the cecum. A history of oral ulcers raised concern for IBD. However, biopsies revealed chronic active eosinophilic colitis with crypt distortion and up to 80 eosinophils/HPF, and IBD testing was negative. Given a history of freshwater exposure in a schistosomiasis-endemic region, parasitic infection was suspected. Stool and serologic testing confirmed schistosomiasis and strongyloidiasis. He was treated with albendazole, praziquantel, and steroids, and showed marked improvement. Follow-up endoscopy and colonoscopy were later scheduled.
Discussion: This case of a young cirrhotic male with transverse colonic strictures and ulcerations due to coexisting schistosomiasis and strongyloidiasis highlights several challenges in the management of cirrhosis complicated by parasitic colitis. Initially, the unusual transverse colon involvement, history of the oral ulcer and lack of eosinophilia mimicked IBD. Despite absent eosinophilia, serology testing and biopsy-confirmed diagnosis prevented mismanagement and treatment with albendazole and praziquantel led to significant improvement, underscoring the need for early recognition and appropriate therapy.
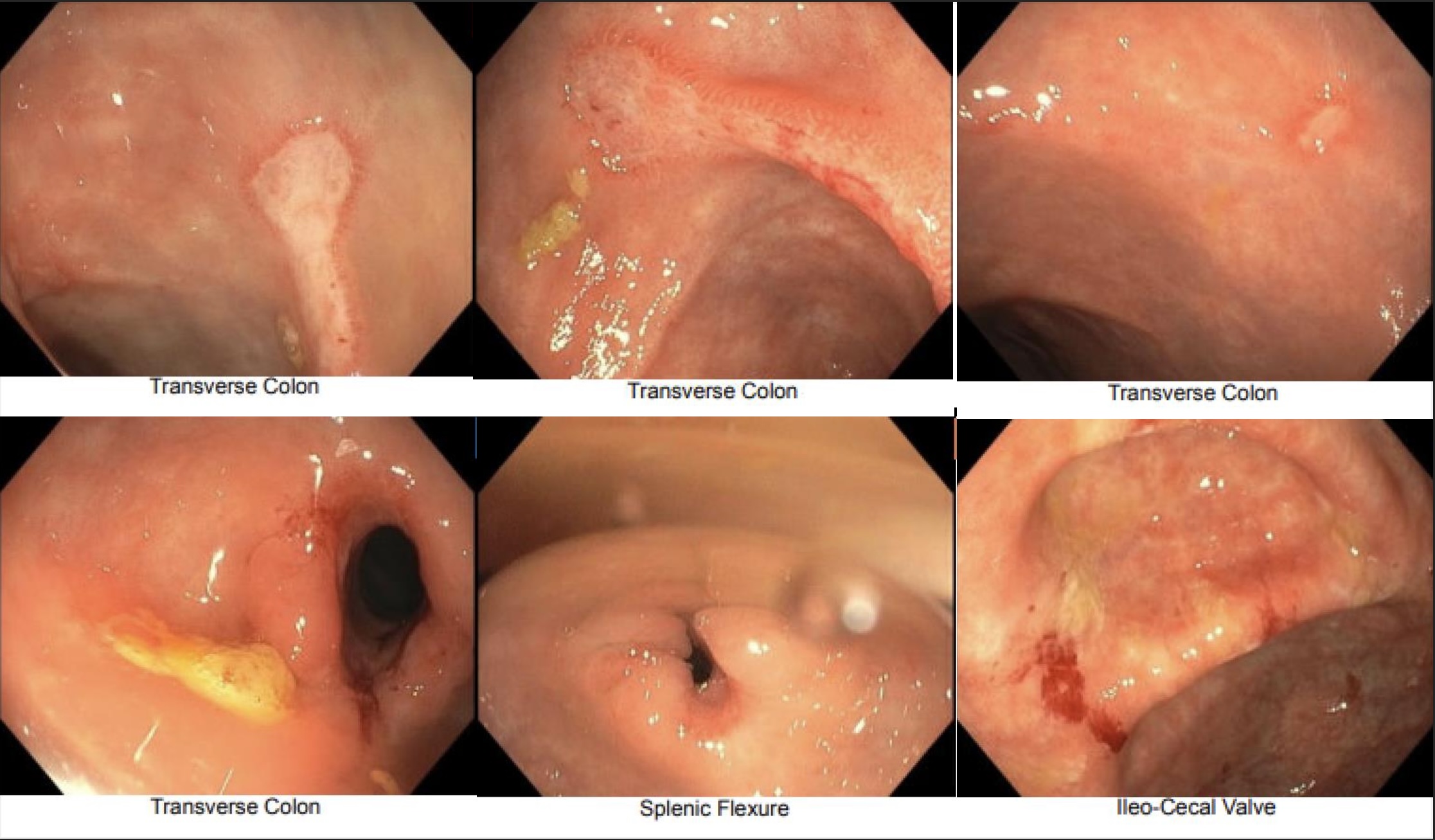
Figure: Images of the transverse colon reveal stricture and ulcerating disease. Stricture also present in splenic flexure, as well as a friable ileo-cecal valve.
Disclosures:
Kranthi Mandava indicated no relevant financial relationships.
Joshua Pagán-Busigó indicated no relevant financial relationships.
Ethan Shamsian indicated no relevant financial relationships.
Michael Bebawy indicated no relevant financial relationships.
Mohamed Ismail indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Kranthi Mandava, MD1, Joshua E. Pagán-Busigó, MD2, Ethan Shamsian, DO1, Michael Bebawy, DO1, Mohamed Ismail, DO1, Menna-Allah Elaskandrany, DO3, Ahmed Al-Khazraji, MD1. P1361 - Double Trouble: Unmasking Parasitic Colitis Mimicking Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
