Sunday Poster Session
Category: Infections and Microbiome
P1357 - Beyond the Surface: Refractory Small Intestinal Bacterial Overgrowth as the Hidden Driver of Recurrent Pneumatosis Intestinalis in Atypical Small Bowel Crohn’s
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Omair Khokhar, MD, MPH (he/him/his)
Sovah Health
Arlington, VA
Presenting Author(s)
Omair Khokhar, MD, MPH1, Cassandra Minor, MD2
1Sovah Health, Arlington, VA; 2W. G. (Bill) Heffner Veterans Affairs Medical Center, Salisbury, NC
Introduction: Small intestinal bacterial overgrowth (SIBO) is defined by an abnormal increase in bacterial populations in the small intestine, leading to symptoms such as bloating, diarrhea, and nutrient malabsorption. When standard therapies fail, alternative treatment options must be considered.
Case Description/
Methods: We present a 77-year-old male with end-stage renal disease on hemodialysis and a complex GI history, including perforated appendicitis, sigmoid diverticulitis post-resection, and recurrent SIBO. He reports persistent explosive flatulence and intermittent secretory diarrhea, refractory to multiple antibiotics (rifaximin, neomycin, vancomycin) since his SIBO diagnosis via breath testing in 2017.
CT imaging from 2016 and 2020 showed small bowel pneumatosis and free peritoneal air without peritonitis. CT enterography revealed jejunal pneumatosis, extensive small bowel diverticulosis, and bowel dilation consistent with ileus. Pneumatosis was attributed to transmural gas due to SIBO rather than true perforation.
Capsule endoscopy in 2020 showed jejunal ulcerations and pneumatosis, with capsule retention in a large diverticulum. A repeat in 2024 revealed additional erosions and fissures. Due to concern for Crohn’s disease, double-balloon enteroscopy was considered but deferred due to high perforation risk.
Colonoscopy in 2019 showed only benign polyps. IBD serologies were equivocal, celiac testing was negative, and duodenal biopsies were normal. Fecal calprotectin was persistently elevated (~240) but recently improved to 90.
He has had four C. difficile infections, most recently in 2020. Despite some biochemical improvement with budesonide, vedolizumab, and infliximab, his GI symptoms persist.
Discussion: Although inflammatory markers such as fecal calprotectin have shown improvement, the persistence of clinical symptoms points toward underlying refractory SIBO as a likely driver rather than atypical small bowel Crohn’s disease.
Given that standard therapeutic approaches have been exhausted, the next step will be to pursue fecal microbiota transplantation (FMT). Emerging evidence supports the use of FMT as a potential therapeutic option for SIBO, with studies indicating its ability to alleviate gastrointestinal symptoms and restore microbial balance.
Gastrointestinal symptoms caused by SIBO can be both debilitating and discouraging. FMT represents a promising therapeutic option for refractory cases. However, further research is needed to establish its role in the management of SIBO.
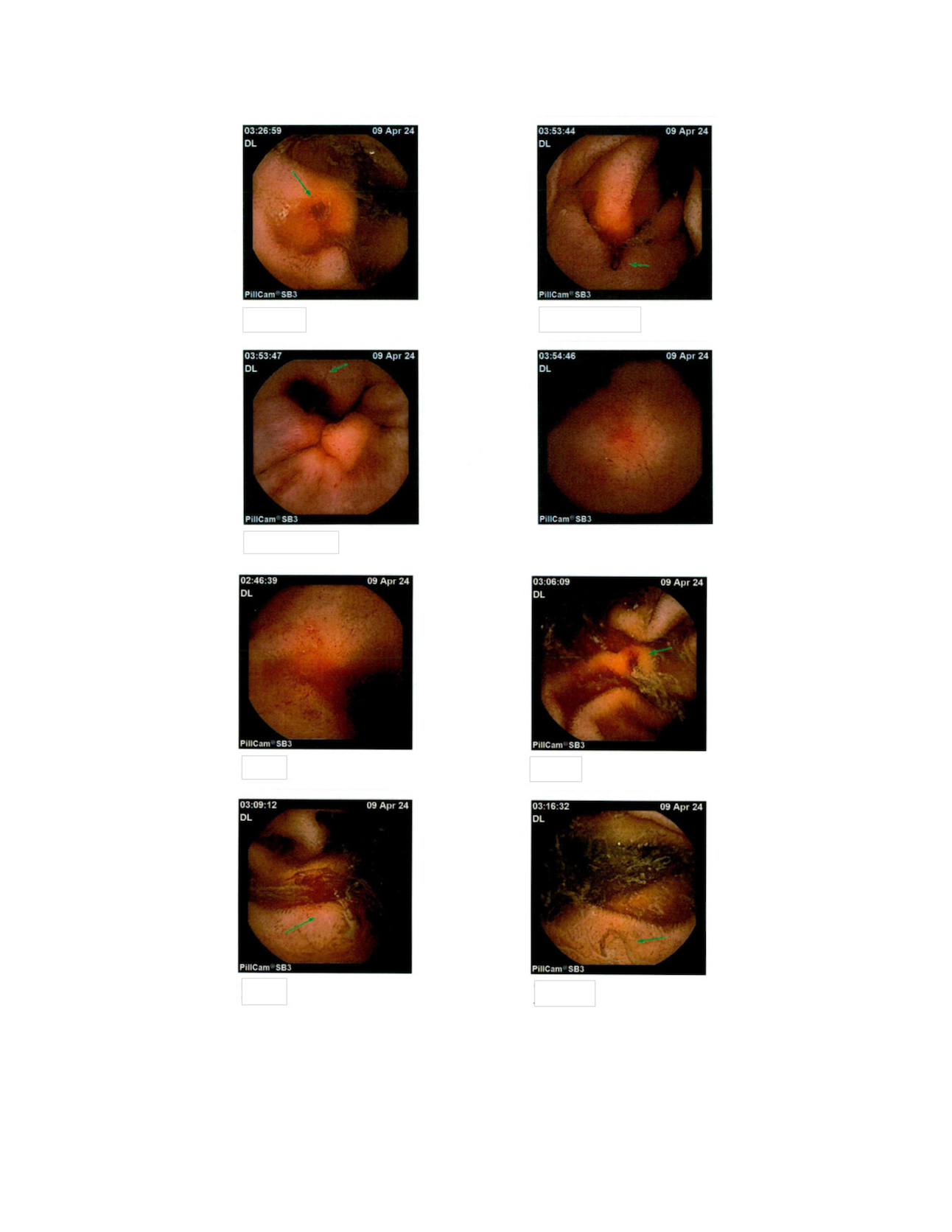
Figure: Hydrogen Breath Test: Early rise in combined hydrogen and methane production diagnostic for severe bacterial overgrowth
CT Abdomen/Pelvis: Revealing small bowel pneumatosis intestinalis
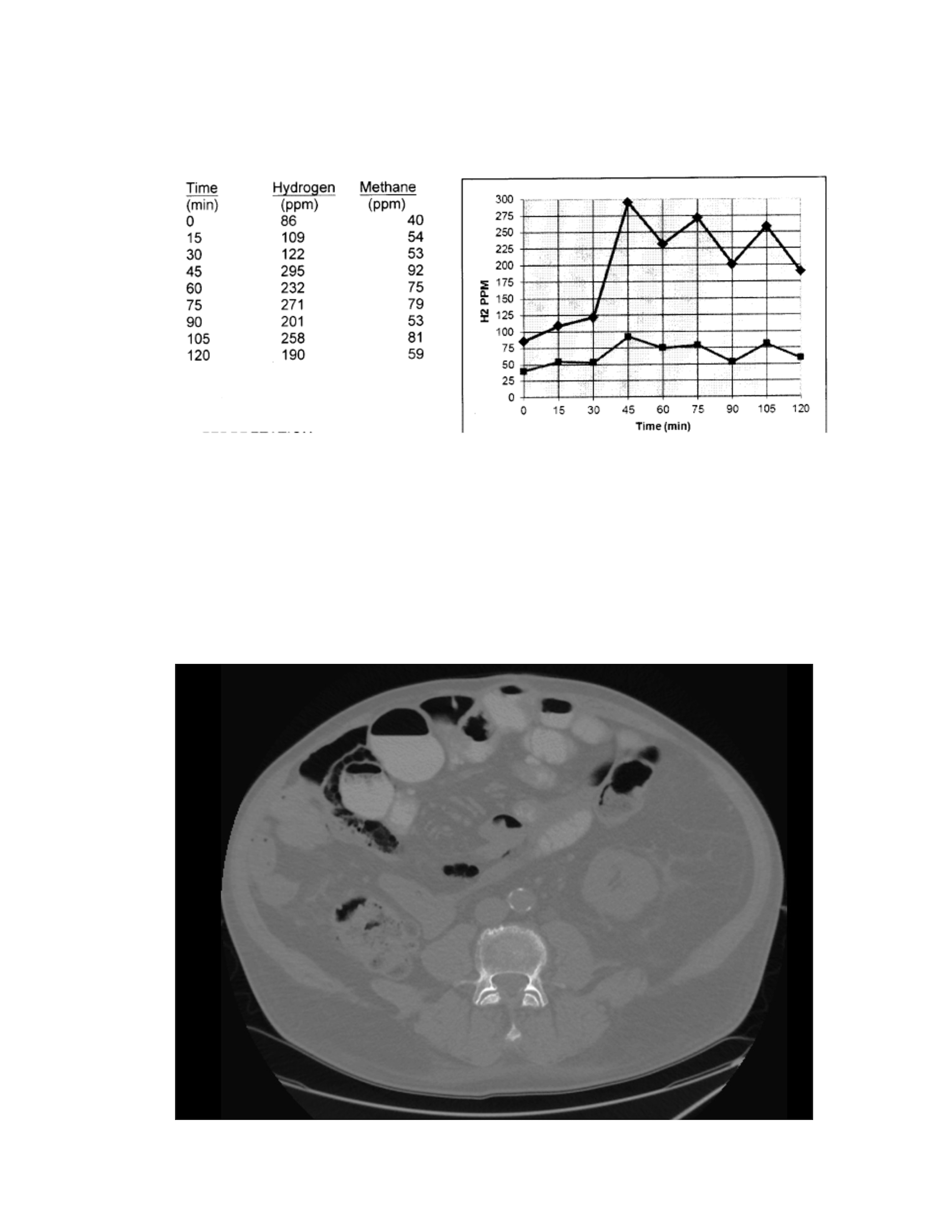
Figure: Capsule endoscopy: revealing ulcerations, erosions and fissures
Disclosures:
Omair Khokhar indicated no relevant financial relationships.
Cassandra Minor indicated no relevant financial relationships.
Omair Khokhar, MD, MPH1, Cassandra Minor, MD2. P1357 - Beyond the Surface: Refractory Small Intestinal Bacterial Overgrowth as the Hidden Driver of Recurrent Pneumatosis Intestinalis in Atypical Small Bowel Crohn’s, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Sovah Health, Arlington, VA; 2W. G. (Bill) Heffner Veterans Affairs Medical Center, Salisbury, NC
Introduction: Small intestinal bacterial overgrowth (SIBO) is defined by an abnormal increase in bacterial populations in the small intestine, leading to symptoms such as bloating, diarrhea, and nutrient malabsorption. When standard therapies fail, alternative treatment options must be considered.
Case Description/
Methods: We present a 77-year-old male with end-stage renal disease on hemodialysis and a complex GI history, including perforated appendicitis, sigmoid diverticulitis post-resection, and recurrent SIBO. He reports persistent explosive flatulence and intermittent secretory diarrhea, refractory to multiple antibiotics (rifaximin, neomycin, vancomycin) since his SIBO diagnosis via breath testing in 2017.
CT imaging from 2016 and 2020 showed small bowel pneumatosis and free peritoneal air without peritonitis. CT enterography revealed jejunal pneumatosis, extensive small bowel diverticulosis, and bowel dilation consistent with ileus. Pneumatosis was attributed to transmural gas due to SIBO rather than true perforation.
Capsule endoscopy in 2020 showed jejunal ulcerations and pneumatosis, with capsule retention in a large diverticulum. A repeat in 2024 revealed additional erosions and fissures. Due to concern for Crohn’s disease, double-balloon enteroscopy was considered but deferred due to high perforation risk.
Colonoscopy in 2019 showed only benign polyps. IBD serologies were equivocal, celiac testing was negative, and duodenal biopsies were normal. Fecal calprotectin was persistently elevated (~240) but recently improved to 90.
He has had four C. difficile infections, most recently in 2020. Despite some biochemical improvement with budesonide, vedolizumab, and infliximab, his GI symptoms persist.
Discussion: Although inflammatory markers such as fecal calprotectin have shown improvement, the persistence of clinical symptoms points toward underlying refractory SIBO as a likely driver rather than atypical small bowel Crohn’s disease.
Given that standard therapeutic approaches have been exhausted, the next step will be to pursue fecal microbiota transplantation (FMT). Emerging evidence supports the use of FMT as a potential therapeutic option for SIBO, with studies indicating its ability to alleviate gastrointestinal symptoms and restore microbial balance.
Gastrointestinal symptoms caused by SIBO can be both debilitating and discouraging. FMT represents a promising therapeutic option for refractory cases. However, further research is needed to establish its role in the management of SIBO.
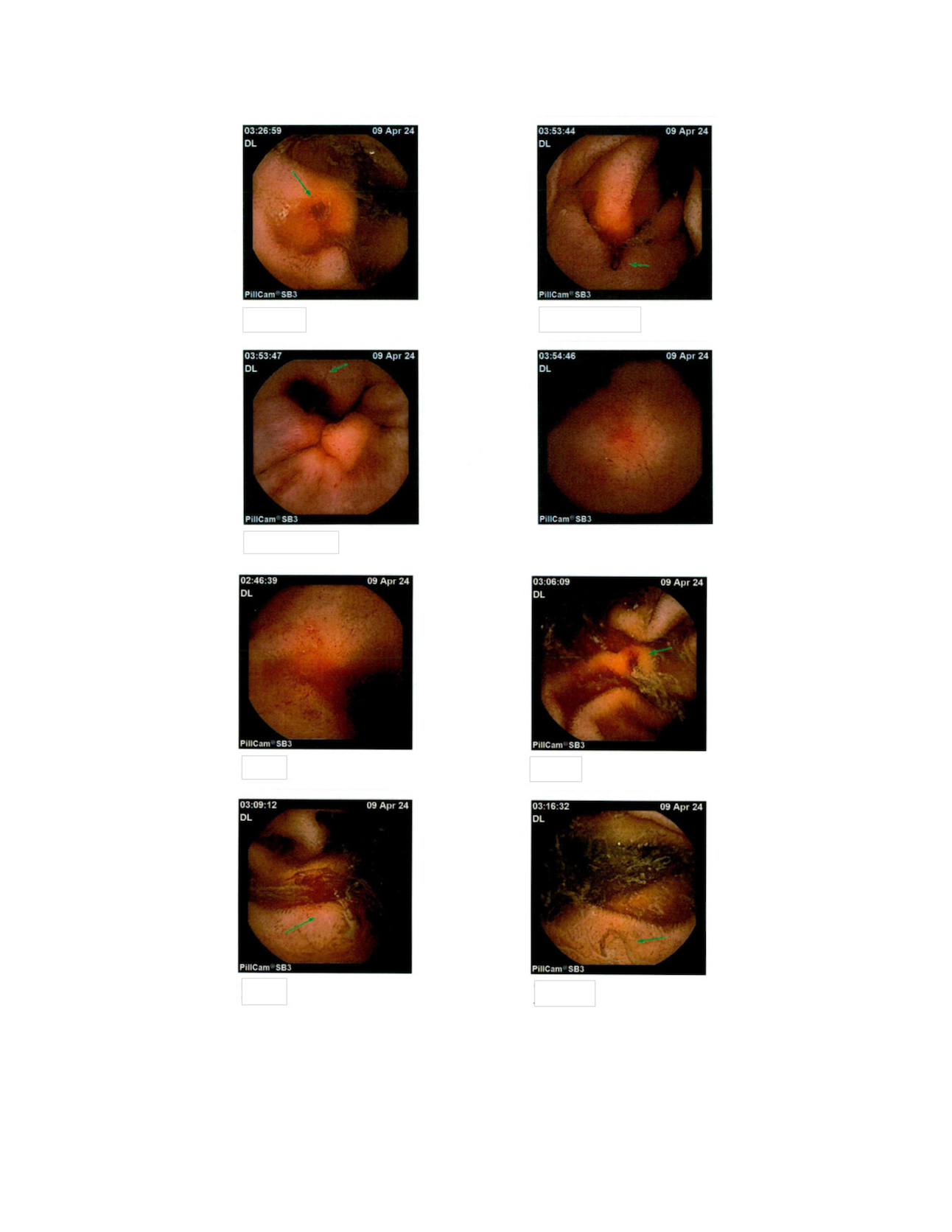
Figure: Hydrogen Breath Test: Early rise in combined hydrogen and methane production diagnostic for severe bacterial overgrowth
CT Abdomen/Pelvis: Revealing small bowel pneumatosis intestinalis
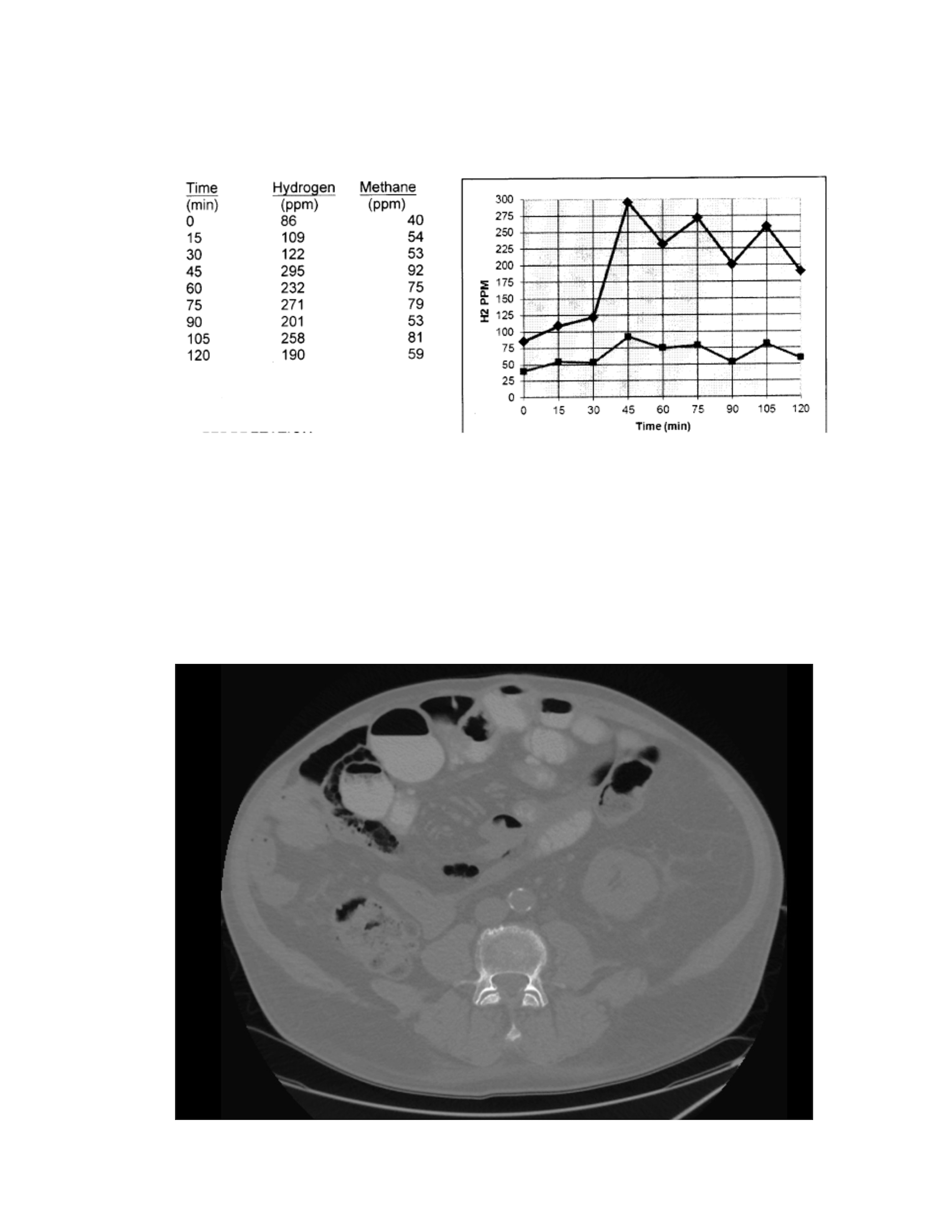
Figure: Capsule endoscopy: revealing ulcerations, erosions and fissures
Disclosures:
Omair Khokhar indicated no relevant financial relationships.
Cassandra Minor indicated no relevant financial relationships.
Omair Khokhar, MD, MPH1, Cassandra Minor, MD2. P1357 - Beyond the Surface: Refractory Small Intestinal Bacterial Overgrowth as the Hidden Driver of Recurrent Pneumatosis Intestinalis in Atypical Small Bowel Crohn’s, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
