Sunday Poster Session
Category: Infections and Microbiome
P1281 - Effects of Opioids on Gastrointestinal Microbiome Diversity and Composition: A Systematic Review
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Farheen F. Vhora, MBBS (she/her/hers)
B.J. Medical College, Ahmedabad
Ahmedabad, Gujarat, India
Presenting Author(s)
Abhay A.. Kapoor, MBBS1, Ratnadeep Biswas, MBBS2, Pratima Jasti, MBBS3, Farheen F.. Vhora, MBBS4, Gurleen Kaur, MBBS5, Vraj J.. Rangrej, MBBS6, Digvijay S.. Rajawat, 5, Ibrahim Reyaz, MBBS7
1St. Mary Medical Center, Langhorne, Langhorne, PA; 2ESIC Medical College & Hospital, Bihta, Patna, Patna, Bihar, India; 3All India Institute of Medical Sciences, Bhubaneswar, Bhubaneswar, Orissa, India; 4B.J. Medical College, Ahmedabad, Ahmedabad, Gujarat, India; 5All India Institute of Medical Sciences, Patna, Patna, Bihar, India; 6GMERS Medical College Gotri, Vadodara, Vadodara, Gujarat, India; 7Nassau University Medical Center, East Meadow, NY
Introduction: Opioids, while critical for analgesia, also alter host physiology. Their use has been linked to changes in the GI microbiome, which may influence host immunity, metabolism, and clinical outcomes. Understanding these changes may enable microbiome-focused interventions to reduce opioid-related harms. This review synthesizes human studies examining how opioid exposure alters the GI microbiome.
Methods: We comprehensively searched PubMed, Embase, Scopus, Cochrane, OVID, and ClinicalTrials.gov from inception to May 2025 using a uniform search strategy according to the PRISMA guidelines. After deduplication (n = 565), 721 records were screened by title and abstract (643 excluded). Seventy-eight full texts were reviewed, out of which, 73 were excluded and a total of five observational studies were included in the review.
Results: All studies reported reduced α-diversity in opioid-exposed versus control groups. Neonates with neonatal abstinence syndrome had lower Faith’s phylogenetic diversity (≈0.56; p = 0.035). Oxycodone-treated cancer patients trended toward decreased Chao1 and Shannon indices versus opioid-naïve peers. Cirrhotic patients on chronic opioids exhibited significantly lower genus-level richness (p < 0.01) compared to non-users. β-diversity analyses uniformly showed distinct clustering between opioid‐exposed and control groups.
Taxonomic shifts consistently included Proteobacteria expansion (e.g., Escherichia-Shigella) and depletion of Firmicutes (e.g., Ruminococcaceae, Lachnospiraceae). In NAS, Escherichia-Shigella and Bacteroides increased with symptom severity, while Bifidobacterium decreased. Cancer patients on oxycodone showed elevated Lactobacillus (p = 0.025), Anaerostipes (p = 0.034), and Megamonas (p = 0.008). Cirrhotic opioid users had reduced Ruminococcaceae and Lachnospiraceae, coupled with lower Bacteroidaceae.
Discussion: Opioid exposure was consistently linked to gut dysbiosis characterized by reduced α‐diversity, altered β‐diversity, and expansion of potentially pathogenic taxa (e.g., Proteobacteria) alongside loss of beneficial anaerobes (e.g., Ruminococcaceae). Clinically, these changes may promote systemic inflammation via increased endotoxin production, worsen GI symptoms (constipation, bloating), and alter drug metabolism. Monitoring microbial shifts could guide probiotic or prebiotic therapy to restore balance and improve patient outcomes. Future longitudinal, larger‐scale studies are needed to elucidate mechanistic links between opioid use and dysbiosis.
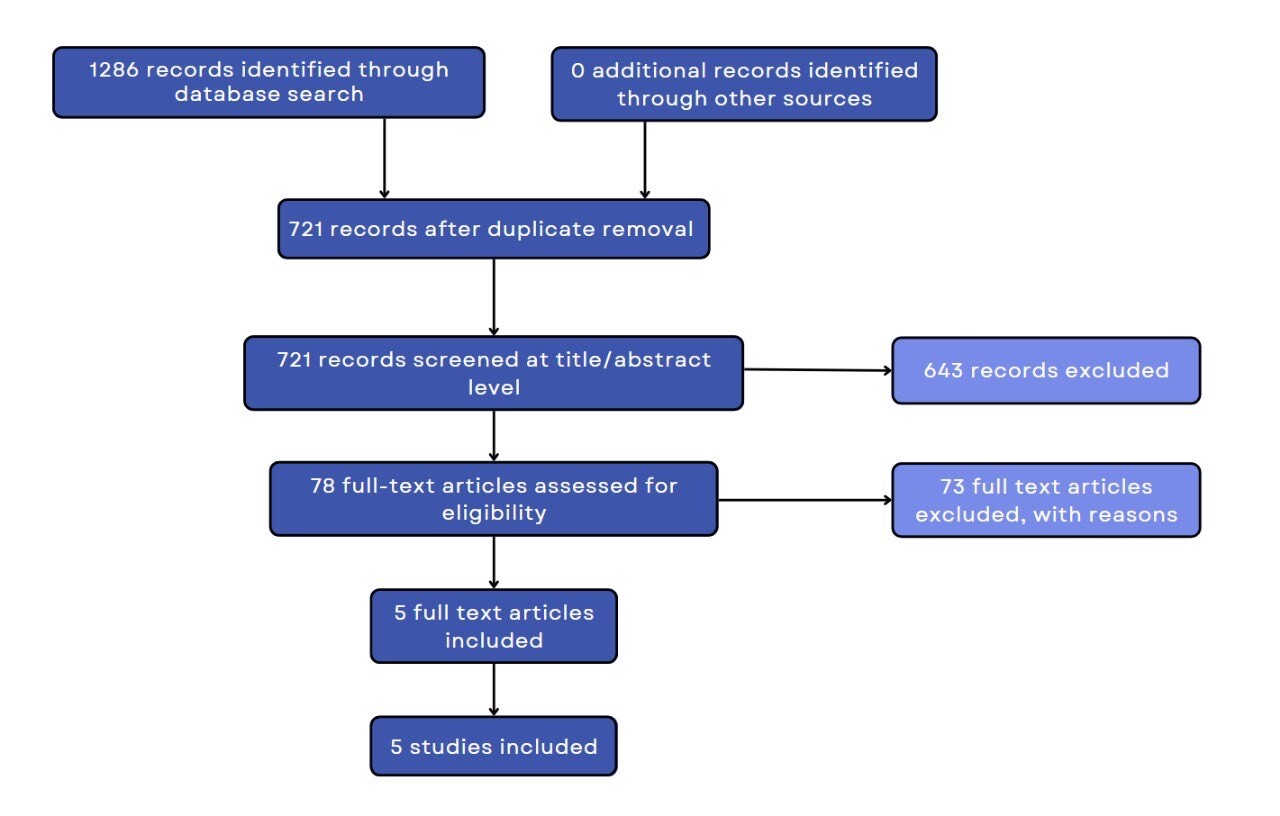
Figure: PRISMA flowchart of the study
Disclosures:
Abhay Kapoor indicated no relevant financial relationships.
Ratnadeep Biswas indicated no relevant financial relationships.
Pratima Jasti indicated no relevant financial relationships.
Farheen Vhora indicated no relevant financial relationships.
Gurleen Kaur indicated no relevant financial relationships.
Vraj Rangrej indicated no relevant financial relationships.
Digvijay Rajawat indicated no relevant financial relationships.
Ibrahim Reyaz indicated no relevant financial relationships.
Abhay A.. Kapoor, MBBS1, Ratnadeep Biswas, MBBS2, Pratima Jasti, MBBS3, Farheen F.. Vhora, MBBS4, Gurleen Kaur, MBBS5, Vraj J.. Rangrej, MBBS6, Digvijay S.. Rajawat, 5, Ibrahim Reyaz, MBBS7. P1281 - Effects of Opioids on Gastrointestinal Microbiome Diversity and Composition: A Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Mary Medical Center, Langhorne, Langhorne, PA; 2ESIC Medical College & Hospital, Bihta, Patna, Patna, Bihar, India; 3All India Institute of Medical Sciences, Bhubaneswar, Bhubaneswar, Orissa, India; 4B.J. Medical College, Ahmedabad, Ahmedabad, Gujarat, India; 5All India Institute of Medical Sciences, Patna, Patna, Bihar, India; 6GMERS Medical College Gotri, Vadodara, Vadodara, Gujarat, India; 7Nassau University Medical Center, East Meadow, NY
Introduction: Opioids, while critical for analgesia, also alter host physiology. Their use has been linked to changes in the GI microbiome, which may influence host immunity, metabolism, and clinical outcomes. Understanding these changes may enable microbiome-focused interventions to reduce opioid-related harms. This review synthesizes human studies examining how opioid exposure alters the GI microbiome.
Methods: We comprehensively searched PubMed, Embase, Scopus, Cochrane, OVID, and ClinicalTrials.gov from inception to May 2025 using a uniform search strategy according to the PRISMA guidelines. After deduplication (n = 565), 721 records were screened by title and abstract (643 excluded). Seventy-eight full texts were reviewed, out of which, 73 were excluded and a total of five observational studies were included in the review.
Results: All studies reported reduced α-diversity in opioid-exposed versus control groups. Neonates with neonatal abstinence syndrome had lower Faith’s phylogenetic diversity (≈0.56; p = 0.035). Oxycodone-treated cancer patients trended toward decreased Chao1 and Shannon indices versus opioid-naïve peers. Cirrhotic patients on chronic opioids exhibited significantly lower genus-level richness (p < 0.01) compared to non-users. β-diversity analyses uniformly showed distinct clustering between opioid‐exposed and control groups.
Taxonomic shifts consistently included Proteobacteria expansion (e.g., Escherichia-Shigella) and depletion of Firmicutes (e.g., Ruminococcaceae, Lachnospiraceae). In NAS, Escherichia-Shigella and Bacteroides increased with symptom severity, while Bifidobacterium decreased. Cancer patients on oxycodone showed elevated Lactobacillus (p = 0.025), Anaerostipes (p = 0.034), and Megamonas (p = 0.008). Cirrhotic opioid users had reduced Ruminococcaceae and Lachnospiraceae, coupled with lower Bacteroidaceae.
Discussion: Opioid exposure was consistently linked to gut dysbiosis characterized by reduced α‐diversity, altered β‐diversity, and expansion of potentially pathogenic taxa (e.g., Proteobacteria) alongside loss of beneficial anaerobes (e.g., Ruminococcaceae). Clinically, these changes may promote systemic inflammation via increased endotoxin production, worsen GI symptoms (constipation, bloating), and alter drug metabolism. Monitoring microbial shifts could guide probiotic or prebiotic therapy to restore balance and improve patient outcomes. Future longitudinal, larger‐scale studies are needed to elucidate mechanistic links between opioid use and dysbiosis.
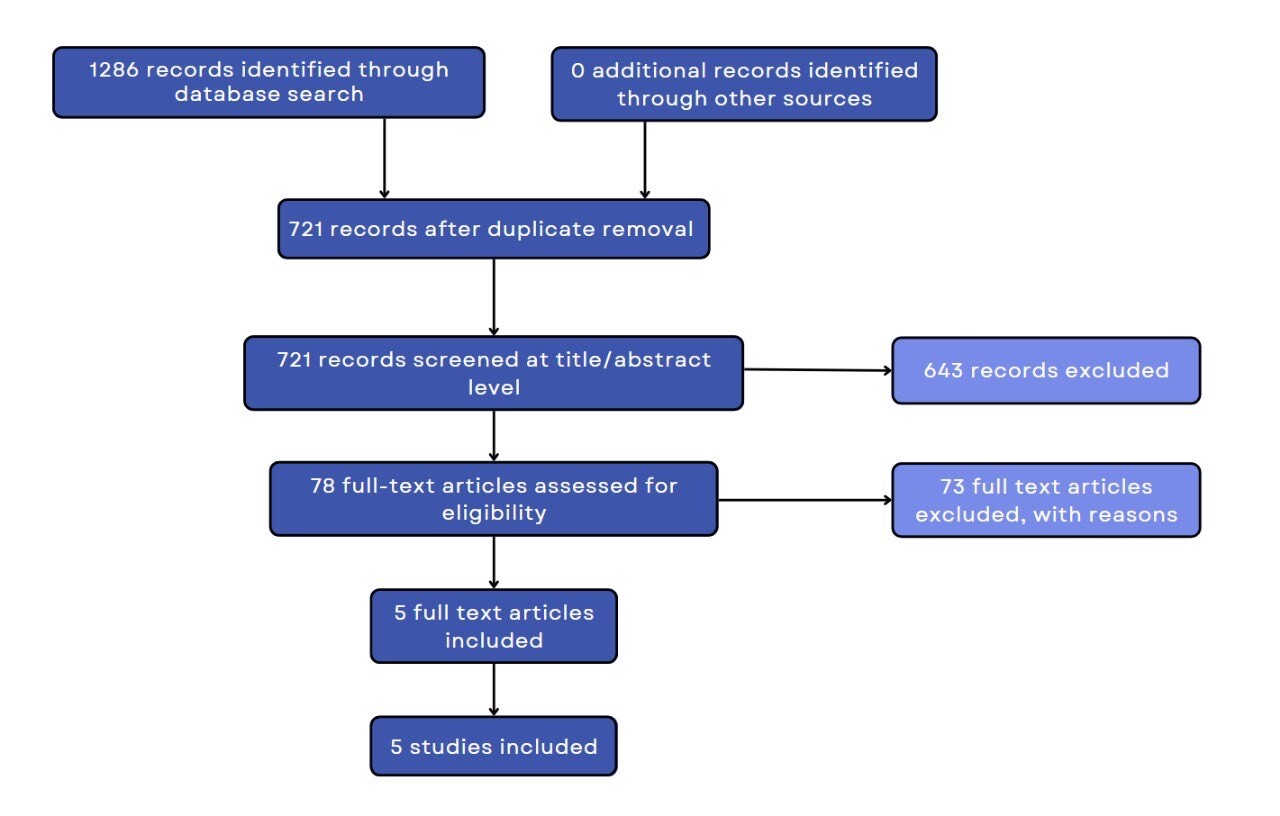
Figure: PRISMA flowchart of the study
Disclosures:
Abhay Kapoor indicated no relevant financial relationships.
Ratnadeep Biswas indicated no relevant financial relationships.
Pratima Jasti indicated no relevant financial relationships.
Farheen Vhora indicated no relevant financial relationships.
Gurleen Kaur indicated no relevant financial relationships.
Vraj Rangrej indicated no relevant financial relationships.
Digvijay Rajawat indicated no relevant financial relationships.
Ibrahim Reyaz indicated no relevant financial relationships.
Abhay A.. Kapoor, MBBS1, Ratnadeep Biswas, MBBS2, Pratima Jasti, MBBS3, Farheen F.. Vhora, MBBS4, Gurleen Kaur, MBBS5, Vraj J.. Rangrej, MBBS6, Digvijay S.. Rajawat, 5, Ibrahim Reyaz, MBBS7. P1281 - Effects of Opioids on Gastrointestinal Microbiome Diversity and Composition: A Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
