Sunday Poster Session
Category: IBD
P1240 - Schistosomiasis: A Parasitic Imposter of Inflammatory Bowel Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Katie A. Dunleavy, MD (she/her/hers)
Mayo Clinic
Medfield, MA
Presenting Author(s)
Julia Liberto, MD, Katie A. Dunleavy, MD
Mayo Clinic, Rochester, MN
Introduction: Schistosomiasis, a parasitic disease endemic to tropical regions, can mimic inflammatory bowel disease (IBD), leading to misdiagnosis and inappropriate treatment.
Case Description/
Methods: A 61-year-old woman presented with nausea, vomiting, hematochezia, abdominal pain, and weight loss after a trip to the Philippines, where she swam in freshwater lakes and consumed local cuisine. GI pathogen panel was negative, and colonoscopy revealed cecal aphthous ulcers and diffuse rectosigmoid inflammation. Histopathology demonstrated chronic active crypt-destructive colitis without granulomas. She was diagnosed with ulcerative colitis (UC) and started oral mesalamine, discontinued due to renal dysfunction, and started prednisone with partial relief.
Six months later, severe symptoms recurred, requiring hospitalization. Imaging revealed left-sided colitis, and she was advised to begin Vedolizumab, which was prescribed but not initiated. Flexible sigmoidoscopy revealed persistent left-sided inflammation. Histopathology identified calcified schistosoma eggs within the lamina propria, diagnostic for schistosomiasis. Liver biopsy confirmed schistosoma eggs in the portal areas with minimal fibrosis. Praziquantel treatment led to partial improvement, but severe malnutrition persisted with a 25-lb weight loss.
A repeat colonoscopy two-months later showed severe colitis from the rectum to the ascending colon (Figure A) and histology confirmed calcified schistosoma eggs in the mucosa, without features of IBD (Figure B). Morphology demonstrated characteristics most consistent with Schistosoma japonicum. After praziquantel re-dosing, she improved significantly at four weeks, gaining 5 lbs with improved symptoms.
Discussion: This case illustrates schistosomiasis as an IBD mimic, particularly in endemic areas. Chronic colitis, mucosal calcification, and liver involvement are key features. Persistent symptoms post-treatment likely reflects mucosal damage rather than active infection. Misdiagnosis of IBD delayed antiparasitic treatment, though the patient did not start biologic therapy, which could have hindered recovery. Parasitic diseases should be considered in colitis cases with relevant travel history. Interestingly, studies suggest that S. japonicum infection protects against colitis in mouse models, possibly due to immune modulation and microbiota alteration. Multidisciplinary care is crucial for accurate diagnosis and management.
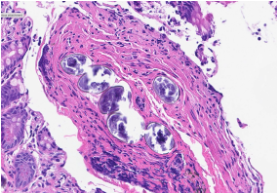
Figure: Endoscopic view of the descending colon showing congestion, erythema, friability, superficial linear erosions, and pseudopolyps arranged in a circumferential pattern extending from the rectum to the ascending colon.
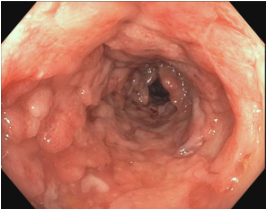
Figure: Histopathology of a colon biopsy demonstrating severely active chronic colitis with focal calcified Schistosoma eggs present within the lamina propria.
Disclosures:
Julia Liberto indicated no relevant financial relationships.
Katie Dunleavy indicated no relevant financial relationships.
Julia Liberto, MD, Katie A. Dunleavy, MD. P1240 - Schistosomiasis: A Parasitic Imposter of Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Schistosomiasis, a parasitic disease endemic to tropical regions, can mimic inflammatory bowel disease (IBD), leading to misdiagnosis and inappropriate treatment.
Case Description/
Methods: A 61-year-old woman presented with nausea, vomiting, hematochezia, abdominal pain, and weight loss after a trip to the Philippines, where she swam in freshwater lakes and consumed local cuisine. GI pathogen panel was negative, and colonoscopy revealed cecal aphthous ulcers and diffuse rectosigmoid inflammation. Histopathology demonstrated chronic active crypt-destructive colitis without granulomas. She was diagnosed with ulcerative colitis (UC) and started oral mesalamine, discontinued due to renal dysfunction, and started prednisone with partial relief.
Six months later, severe symptoms recurred, requiring hospitalization. Imaging revealed left-sided colitis, and she was advised to begin Vedolizumab, which was prescribed but not initiated. Flexible sigmoidoscopy revealed persistent left-sided inflammation. Histopathology identified calcified schistosoma eggs within the lamina propria, diagnostic for schistosomiasis. Liver biopsy confirmed schistosoma eggs in the portal areas with minimal fibrosis. Praziquantel treatment led to partial improvement, but severe malnutrition persisted with a 25-lb weight loss.
A repeat colonoscopy two-months later showed severe colitis from the rectum to the ascending colon (Figure A) and histology confirmed calcified schistosoma eggs in the mucosa, without features of IBD (Figure B). Morphology demonstrated characteristics most consistent with Schistosoma japonicum. After praziquantel re-dosing, she improved significantly at four weeks, gaining 5 lbs with improved symptoms.
Discussion: This case illustrates schistosomiasis as an IBD mimic, particularly in endemic areas. Chronic colitis, mucosal calcification, and liver involvement are key features. Persistent symptoms post-treatment likely reflects mucosal damage rather than active infection. Misdiagnosis of IBD delayed antiparasitic treatment, though the patient did not start biologic therapy, which could have hindered recovery. Parasitic diseases should be considered in colitis cases with relevant travel history. Interestingly, studies suggest that S. japonicum infection protects against colitis in mouse models, possibly due to immune modulation and microbiota alteration. Multidisciplinary care is crucial for accurate diagnosis and management.
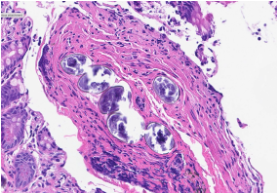
Figure: Endoscopic view of the descending colon showing congestion, erythema, friability, superficial linear erosions, and pseudopolyps arranged in a circumferential pattern extending from the rectum to the ascending colon.
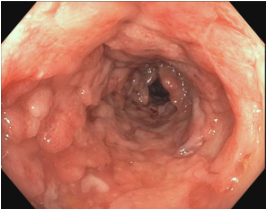
Figure: Histopathology of a colon biopsy demonstrating severely active chronic colitis with focal calcified Schistosoma eggs present within the lamina propria.
Disclosures:
Julia Liberto indicated no relevant financial relationships.
Katie Dunleavy indicated no relevant financial relationships.
Julia Liberto, MD, Katie A. Dunleavy, MD. P1240 - Schistosomiasis: A Parasitic Imposter of Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
