Sunday Poster Session
Category: IBD
P1234 - A Viral Twist to a Familiar Flare: HSV Colitis in Inflammatory Bowel Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Sam Papasotiriou, DO
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
Sam Papasotiriou, DO1, Mario Tavakoli, DO1, Kashif Osmani, MD1, Maria El Gemayel, MD2, Itishree Trivedi, MD2
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois, Chicago, IL
Introduction: Herpes simplex virus (HSV) colitis is a rare infection, mostly documented in immunocompromised individuals, including patients with inflammatory bowel disease (IBD). HSV colitis often has associated morbidity and mortality from complications such as bowel necrosis or perforation. The clinical presentation of HSV colitis can be identical to an exacerbation of colonic IBD, often delaying diagnosis and complicating management.
Case Description/
Methods: A 26-year-old female with history of ulcerative pancolitis, previously in clinical remission with vedolizumab, presented with bloody diarrhea, abdominal pain, and weight loss after being off of vedolizumab for 7 months. Laboratory and imaging findings revealed a CRP of 13.4 mg/L, fecal calprotectin >3000 mg/g, and pancolitis on abdominal CT. Infectious workup including CMV, Clostridium difficile and other stool pathogen testing, was negative.
Patient was initiated on intravenous corticosteroid therapy, however, had lack of clinical improvement. On day 3 of admission, a flexible sigmoidoscopy revealed continuous, severe mucosal inflammation in the descending colon(graded as Mayo 3) and multiple well-demarcated, punched-out ulcers in the sigmoid colon. Histopathology demonstrated moderate chronic active colitis with HSV viral cytopathic effect confirmed via immunohistochemical staining.
Given the HSV colitis diagnosis, IV acyclovir was initiated, and IV corticosteroids were transitioned to oral prednisone. Her symptoms improved rapidly within 3 days and she was discharged on a 2-week valacyclovir course. On follow-up, patient continued to do well and was ultimately restarted on vedolizumab and continued suppressive valacyclovir with colonoscopy after 6 months revealing Mayo 0 colon and resolution of HSV changes.
Discussion: HSV colitis can be indistinguishable in patients with UC, as it can mimic UC flare symptoms, often requiring endoscopic and histologic confirmation. Deep, well-circumscribed ulcers are a unique feature of HSV colitis. Early initiation of anti-viral therapy and a reduction or temporary cessation of immunosuppressive agents is needed for HSV colitis treatment. In our case, balancing management of a UC flare with the need to treat HSV infection was critical. Withholding immunosuppressives carries the risk of worsening UC, while continued steroids may promote viral dissemination and potential tissue necrosis. This case underscores the importance of considering rare infectious triggers of UC in patients with refractory colitis symptoms.

Figure: Ulceration of sigmoid colon
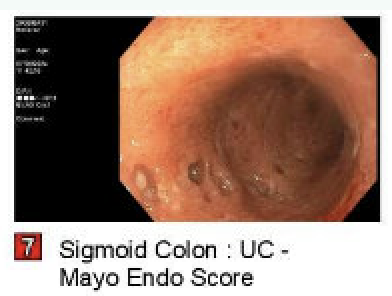
Figure: Punched out lesions
Disclosures:
Sam Papasotiriou indicated no relevant financial relationships.
Mario Tavakoli indicated no relevant financial relationships.
Kashif Osmani indicated no relevant financial relationships.
Maria El Gemayel indicated no relevant financial relationships.
Itishree Trivedi indicated no relevant financial relationships.
Sam Papasotiriou, DO1, Mario Tavakoli, DO1, Kashif Osmani, MD1, Maria El Gemayel, MD2, Itishree Trivedi, MD2. P1234 - A Viral Twist to a Familiar Flare: HSV Colitis in Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois, Chicago, IL
Introduction: Herpes simplex virus (HSV) colitis is a rare infection, mostly documented in immunocompromised individuals, including patients with inflammatory bowel disease (IBD). HSV colitis often has associated morbidity and mortality from complications such as bowel necrosis or perforation. The clinical presentation of HSV colitis can be identical to an exacerbation of colonic IBD, often delaying diagnosis and complicating management.
Case Description/
Methods: A 26-year-old female with history of ulcerative pancolitis, previously in clinical remission with vedolizumab, presented with bloody diarrhea, abdominal pain, and weight loss after being off of vedolizumab for 7 months. Laboratory and imaging findings revealed a CRP of 13.4 mg/L, fecal calprotectin >3000 mg/g, and pancolitis on abdominal CT. Infectious workup including CMV, Clostridium difficile and other stool pathogen testing, was negative.
Patient was initiated on intravenous corticosteroid therapy, however, had lack of clinical improvement. On day 3 of admission, a flexible sigmoidoscopy revealed continuous, severe mucosal inflammation in the descending colon(graded as Mayo 3) and multiple well-demarcated, punched-out ulcers in the sigmoid colon. Histopathology demonstrated moderate chronic active colitis with HSV viral cytopathic effect confirmed via immunohistochemical staining.
Given the HSV colitis diagnosis, IV acyclovir was initiated, and IV corticosteroids were transitioned to oral prednisone. Her symptoms improved rapidly within 3 days and she was discharged on a 2-week valacyclovir course. On follow-up, patient continued to do well and was ultimately restarted on vedolizumab and continued suppressive valacyclovir with colonoscopy after 6 months revealing Mayo 0 colon and resolution of HSV changes.
Discussion: HSV colitis can be indistinguishable in patients with UC, as it can mimic UC flare symptoms, often requiring endoscopic and histologic confirmation. Deep, well-circumscribed ulcers are a unique feature of HSV colitis. Early initiation of anti-viral therapy and a reduction or temporary cessation of immunosuppressive agents is needed for HSV colitis treatment. In our case, balancing management of a UC flare with the need to treat HSV infection was critical. Withholding immunosuppressives carries the risk of worsening UC, while continued steroids may promote viral dissemination and potential tissue necrosis. This case underscores the importance of considering rare infectious triggers of UC in patients with refractory colitis symptoms.

Figure: Ulceration of sigmoid colon
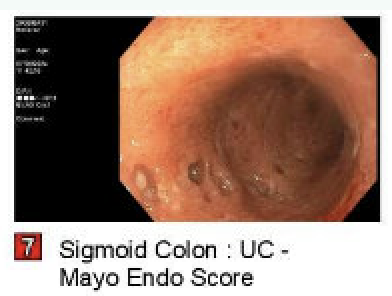
Figure: Punched out lesions
Disclosures:
Sam Papasotiriou indicated no relevant financial relationships.
Mario Tavakoli indicated no relevant financial relationships.
Kashif Osmani indicated no relevant financial relationships.
Maria El Gemayel indicated no relevant financial relationships.
Itishree Trivedi indicated no relevant financial relationships.
Sam Papasotiriou, DO1, Mario Tavakoli, DO1, Kashif Osmani, MD1, Maria El Gemayel, MD2, Itishree Trivedi, MD2. P1234 - A Viral Twist to a Familiar Flare: HSV Colitis in Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
