Sunday Poster Session
Category: IBD
P1232 - Mucosa Building Bridges: An Uncommon Cause of Colonic Obstruction in Ulcerative Colitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Alexander F. Siegel, MD
Creighton University Medical Center
Omaha, NE
Presenting Author(s)
Alexander Siegel, MD1, Kyaw Min Tun, DO2, Aun R. Shah, MBBS, MRCP3
1CHI Health Creighton University Medical Center, Elkhorn, NE; 2Creighton University Medical Center, Omaha, NE; 3CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Mucosal bridging (MB) is a unique phenomenon associated with a variety of inflammatory conditions of the gastrointestinal (GI) tract. These mucosal projections within the GI lumen can lead to complications such as dysphagia, pain or obstruction. While MB is already considered an uncommon finding in inflammatory bowel disease (IBD) patients, colonic MB in patients with ulcerative colitis (UC) is considered particularly rare.
Case Description/
Methods: A 50-year-old male with a past medical history of untreated UC complicated by strictures requiring left hemicolectomy in 2018, recurrent Clostridioides difficile infections (CDI), untreated chronic hepatitis C and polysubstance use presented with a two-day history of progressive abdominal pain, nausea, vomiting, and constipation. Laboratory evaluation was unremarkable, with no leukocytosis, normal inflammatory markers and negative CDI testing. Imaging demonstrated distended loops of small and large bowel, and abdominal CT identified a distal colonic mass at the site the surgical anastomosis. Colonoscopy revealed a circumferential pseudopolyp at the anastomosis contributing to the obstruction. Further examination of the distal colon using pediatric colonoscope showed extensive pseudopolyps and multilobulated diverticula consistent with mucosal bridging. Histologic examination of cecal biopsy demonstrated inflammatory changes with focal cryptitis suggestive of UC. The patient’s symptoms resolved following endoscopic decompression, and no surgical intervention was required. The patient was discharged with follow-up arranged with gastroenterology for outpatient UC management.
Discussion: Colonic mucosal bridging is an uncommon and underrecognized manifestation of UC. Previous reported cases often occurred spontaneously and were discovered incidentally—such as during surveillance colonoscopy or during an acute flare in a patient considered to be in remission. One case did document MB formation a year after sigmoid resection with colo-colonic anastomosis in a patient with active UC. Although MB formation rarely progresses to the severity seen in our case, it is worth considering that patients with undiagnosed or untreated UC may develop subclinical MB. While initially asymptomatic, such anatomical changes to the gut lumen could predispose them to future complications and may necessitate more frequency follow up. Awareness of this potential complication is essential when guiding management and surveillance strategies in IBD patients.
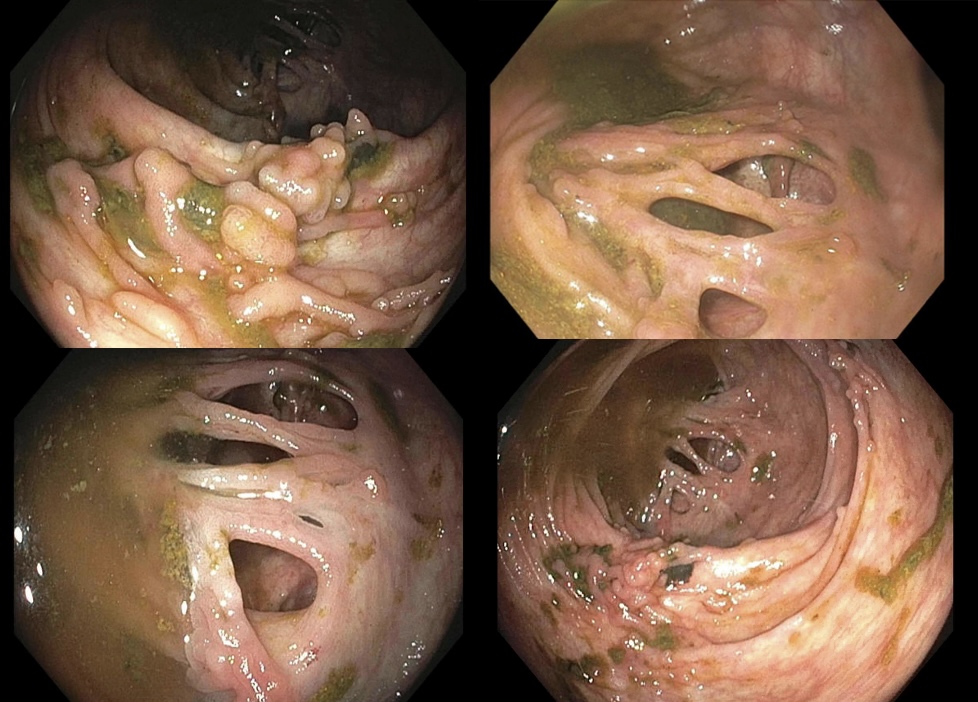
Figure: Endoscopic views of the ascending colon and cecum demonstrating mucosal projections characteristic of mucosal bridging

Figure: Endoscopic image of the ileocecal valve, identified by the yellow arrow, with adjacent pseudopolyps
Disclosures:
Alexander Siegel indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Aun Shah indicated no relevant financial relationships.
Alexander Siegel, MD1, Kyaw Min Tun, DO2, Aun R. Shah, MBBS, MRCP3. P1232 - Mucosa Building Bridges: An Uncommon Cause of Colonic Obstruction in Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1CHI Health Creighton University Medical Center, Elkhorn, NE; 2Creighton University Medical Center, Omaha, NE; 3CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Mucosal bridging (MB) is a unique phenomenon associated with a variety of inflammatory conditions of the gastrointestinal (GI) tract. These mucosal projections within the GI lumen can lead to complications such as dysphagia, pain or obstruction. While MB is already considered an uncommon finding in inflammatory bowel disease (IBD) patients, colonic MB in patients with ulcerative colitis (UC) is considered particularly rare.
Case Description/
Methods: A 50-year-old male with a past medical history of untreated UC complicated by strictures requiring left hemicolectomy in 2018, recurrent Clostridioides difficile infections (CDI), untreated chronic hepatitis C and polysubstance use presented with a two-day history of progressive abdominal pain, nausea, vomiting, and constipation. Laboratory evaluation was unremarkable, with no leukocytosis, normal inflammatory markers and negative CDI testing. Imaging demonstrated distended loops of small and large bowel, and abdominal CT identified a distal colonic mass at the site the surgical anastomosis. Colonoscopy revealed a circumferential pseudopolyp at the anastomosis contributing to the obstruction. Further examination of the distal colon using pediatric colonoscope showed extensive pseudopolyps and multilobulated diverticula consistent with mucosal bridging. Histologic examination of cecal biopsy demonstrated inflammatory changes with focal cryptitis suggestive of UC. The patient’s symptoms resolved following endoscopic decompression, and no surgical intervention was required. The patient was discharged with follow-up arranged with gastroenterology for outpatient UC management.
Discussion: Colonic mucosal bridging is an uncommon and underrecognized manifestation of UC. Previous reported cases often occurred spontaneously and were discovered incidentally—such as during surveillance colonoscopy or during an acute flare in a patient considered to be in remission. One case did document MB formation a year after sigmoid resection with colo-colonic anastomosis in a patient with active UC. Although MB formation rarely progresses to the severity seen in our case, it is worth considering that patients with undiagnosed or untreated UC may develop subclinical MB. While initially asymptomatic, such anatomical changes to the gut lumen could predispose them to future complications and may necessitate more frequency follow up. Awareness of this potential complication is essential when guiding management and surveillance strategies in IBD patients.
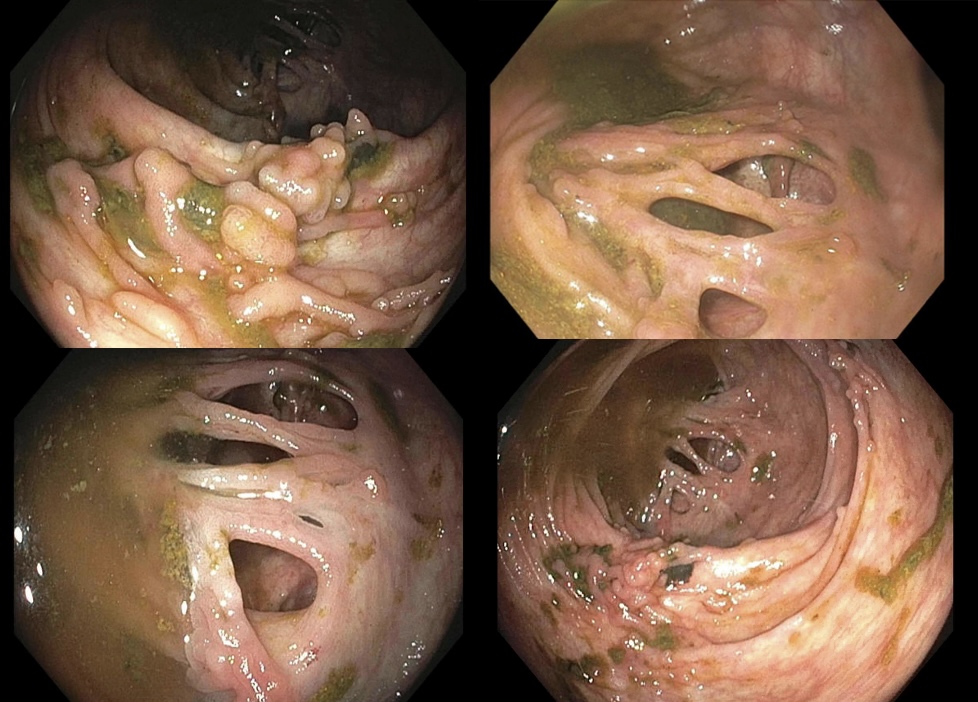
Figure: Endoscopic views of the ascending colon and cecum demonstrating mucosal projections characteristic of mucosal bridging

Figure: Endoscopic image of the ileocecal valve, identified by the yellow arrow, with adjacent pseudopolyps
Disclosures:
Alexander Siegel indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Aun Shah indicated no relevant financial relationships.
Alexander Siegel, MD1, Kyaw Min Tun, DO2, Aun R. Shah, MBBS, MRCP3. P1232 - Mucosa Building Bridges: An Uncommon Cause of Colonic Obstruction in Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
