Sunday Poster Session
Category: IBD
P1220 - Beyond the Gut: Pyoderma Gangrenosum in a Late-Onset Presentation with Enterobacter Cloacae Infection and Crohn's Colitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Salman Bari, MD
Memorial Hospital at Gulfport
Gulfport, MS
Presenting Author(s)
Salman Bari, MD1, Jordan Roussel, MD1, Anam Hamid, MD1, Josh Luke, MD1, Sarah Rashed, MBBS2, Benjamin Smith, MD1
1Memorial Hospital at Gulfport, Gulfport, MS; 2RAK Hospital, Gulfport, MS
Introduction: Pyoderma gangrenosum is an inflammatory and ulcerative skin condition characterized by painful pustules that progressively develop into ulcers. It is an extraintestinal manifestation of inflammatory bowel disease (IBD), affecting approximately 5% to 12% of patients with ulcerative colitis. This condition tends to affect women more than men, typically in the age range of 20 to 50 years.
In this case report, we present an interesting instance of late-onset pyoderma gangrenosum, complicated by a secondary bacterial infection, in a previously undiagnosed patient with IBD.
Case Description/
Methods: A 79-year-old w/oman with dementia and breast cancer presented with painful skin lesions on her lower extremities and under her left breast that developed over 2 weeks. The lesions worsened despite two courses of antibiotics, resulting in ulceration and erythema.
Labs showed Wbc-11.8 and ESR-38. Treatment with vancomycin and doxycycline was initiated. The wound care team treated the lesions, and a punch biopsy of five lesions revealed dense neutrophilic inflammation without signs of infection or viropathic changes, suggesting pyoderma gangrenosum. Tissue and wound cultures confirmed an Enterobacter cloacae complex infection, prompting a switch to IV Cefepime and IV Flagyl.
The patient had an acute onset of rectal bleeding with no previous history of IBD. A CT scan showed wall thickening in the mid-transverse colon, and flexible sigmoidoscopy findings of erythema and inflammation with scattered punched-out ulcers in the sigmoid and rectum, possibly Crohn's colitis.
The skin biopsy confirmed PG and wound cultures revealed infection. The patient was managed with a 2-week course of IV cefepime, IV Flagyl, and prednisone 40 mg daily, improving symptoms of both IBD and PG.
Discussion: Pyoderma gangrenosum (PG) is believed to result from immune dysregulation. Increased levels of inflammatory mediators are observed in PG. Diagnosing can be challenging; it is essential to rule out other ulcerative conditions. PG can occur alongside flare-ups of ulcerative colitis, suggesting a likely connection between them.
The diagnosis typically involves a skin biopsy that reveals neutrophil infiltrates and necrotic dermal vessels. A thorough evaluation, which includes wound biopsy and cultures, colonoscopy, is crucial for an accurate diagnosis.
Treatment plans include high-dose steroids and outpatient immunomodulators. Effective wound care and pain management are essential. Ustekinumab demonstrated effectiveness in managing PG.
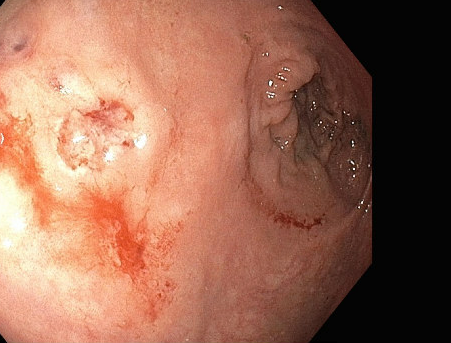
Figure: Pyoderma gangrenosum of the right leg- Deep ulcer with a raised, violaceous border. Erythema in the surrounding skin.

Figure: Colonoscopy- Erythema and inflammation with punched-out ulcers.
Disclosures:
Salman Bari indicated no relevant financial relationships.
Jordan Roussel indicated no relevant financial relationships.
Anam Hamid indicated no relevant financial relationships.
Josh Luke indicated no relevant financial relationships.
Sarah Rashed indicated no relevant financial relationships.
Benjamin Smith indicated no relevant financial relationships.
Salman Bari, MD1, Jordan Roussel, MD1, Anam Hamid, MD1, Josh Luke, MD1, Sarah Rashed, MBBS2, Benjamin Smith, MD1. P1220 - Beyond the Gut: Pyoderma Gangrenosum in a Late-Onset Presentation with Enterobacter Cloacae Infection and Crohn's Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Memorial Hospital at Gulfport, Gulfport, MS; 2RAK Hospital, Gulfport, MS
Introduction: Pyoderma gangrenosum is an inflammatory and ulcerative skin condition characterized by painful pustules that progressively develop into ulcers. It is an extraintestinal manifestation of inflammatory bowel disease (IBD), affecting approximately 5% to 12% of patients with ulcerative colitis. This condition tends to affect women more than men, typically in the age range of 20 to 50 years.
In this case report, we present an interesting instance of late-onset pyoderma gangrenosum, complicated by a secondary bacterial infection, in a previously undiagnosed patient with IBD.
Case Description/
Methods: A 79-year-old w/oman with dementia and breast cancer presented with painful skin lesions on her lower extremities and under her left breast that developed over 2 weeks. The lesions worsened despite two courses of antibiotics, resulting in ulceration and erythema.
Labs showed Wbc-11.8 and ESR-38. Treatment with vancomycin and doxycycline was initiated. The wound care team treated the lesions, and a punch biopsy of five lesions revealed dense neutrophilic inflammation without signs of infection or viropathic changes, suggesting pyoderma gangrenosum. Tissue and wound cultures confirmed an Enterobacter cloacae complex infection, prompting a switch to IV Cefepime and IV Flagyl.
The patient had an acute onset of rectal bleeding with no previous history of IBD. A CT scan showed wall thickening in the mid-transverse colon, and flexible sigmoidoscopy findings of erythema and inflammation with scattered punched-out ulcers in the sigmoid and rectum, possibly Crohn's colitis.
The skin biopsy confirmed PG and wound cultures revealed infection. The patient was managed with a 2-week course of IV cefepime, IV Flagyl, and prednisone 40 mg daily, improving symptoms of both IBD and PG.
Discussion: Pyoderma gangrenosum (PG) is believed to result from immune dysregulation. Increased levels of inflammatory mediators are observed in PG. Diagnosing can be challenging; it is essential to rule out other ulcerative conditions. PG can occur alongside flare-ups of ulcerative colitis, suggesting a likely connection between them.
The diagnosis typically involves a skin biopsy that reveals neutrophil infiltrates and necrotic dermal vessels. A thorough evaluation, which includes wound biopsy and cultures, colonoscopy, is crucial for an accurate diagnosis.
Treatment plans include high-dose steroids and outpatient immunomodulators. Effective wound care and pain management are essential. Ustekinumab demonstrated effectiveness in managing PG.
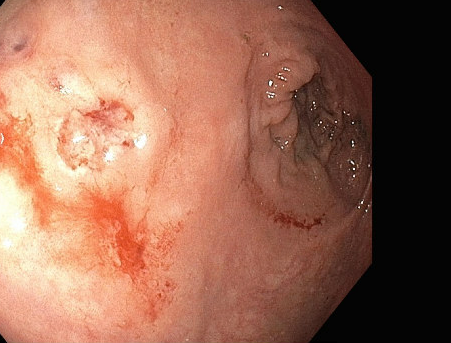
Figure: Pyoderma gangrenosum of the right leg- Deep ulcer with a raised, violaceous border. Erythema in the surrounding skin.

Figure: Colonoscopy- Erythema and inflammation with punched-out ulcers.
Disclosures:
Salman Bari indicated no relevant financial relationships.
Jordan Roussel indicated no relevant financial relationships.
Anam Hamid indicated no relevant financial relationships.
Josh Luke indicated no relevant financial relationships.
Sarah Rashed indicated no relevant financial relationships.
Benjamin Smith indicated no relevant financial relationships.
Salman Bari, MD1, Jordan Roussel, MD1, Anam Hamid, MD1, Josh Luke, MD1, Sarah Rashed, MBBS2, Benjamin Smith, MD1. P1220 - Beyond the Gut: Pyoderma Gangrenosum in a Late-Onset Presentation with Enterobacter Cloacae Infection and Crohn's Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

