Sunday Poster Session
Category: IBD
P1217 - Miller Fisher Syndrome: A Rare Manifestation of Anti-TNF Therapy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Aastha Chokshi, MD (she/her/hers)
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Award: ACG Presidential Poster Award
Aastha Chokshi, MD1, Dania Hudhud, MD2, Ekta Gupta, MD3
1University of Maryland Medical Center, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD; 3University of Maryland, Balitmore, MD
Introduction: Infliximab, an anti-tumor necrosis factor (TNF) alpha inhibitor, is a commonly used biologic therapy for patients with inflammatory bowel disease (IBD). Neurologic complications, such as Guillain-Barré syndrome (GBS) and its variants, Miller Fisher syndrome (MFS), are rare side effects of anti-TNF inhibitors. We report a case of severe ulcerative colitis (UC) complicated by suspected infliximab-induced MFS, highlighting the importance of having a low threshold of suspicion in patients developing new neurological symptoms.
Case Description/
Methods: A 70-year-old male with a history of right hemicolectomy for cecal tubulovillous adenoma, COPD, OSA, and recently diagnosed ulcerative pancolitis presented with profuse watery diarrhea and abdominal pain. A year earlier, a colonoscopy showed chronic colitis, but treatment was deferred. Six months later, he was hospitalized for bloody diarrhea and started on steroids and mesalamine. He continued to have recurrent flares requiring steroids and therefore infliximab was initiated but discontinued after developing a drug-induced rash after the second dose.
During this admission, he tested positive for C. difficile PCR (toxin negative) and was treated with vancomycin and then fidaxomicin. Sigmoidoscopy showed severe UC (Mayo 2). IV steroids were started but discontinued after two days due to agitation. He received one induction dose of infliximab. Due to lack of clinical response with infliximab, he was switched to upadacitinib which he received for 2 days.
He then developed disorientation, slurred speech, and dysphagia requiring ICU admission and intubation. Imaging and CSF studies were unremarkable. On exam, he was disoriented, dysarthric, had upward gaze palsy, areflexic in lower extremities and hyporeflexic in upper extremities. He underwent urgent colectomy and was diagnosed with infliximab-induced MFS. He received IVIG with clinical improvement.
Discussion: This case highlights a rare but critical complication of biologic therapy in UC—suspected infliximab-induced MFS, characterized by ophthalmoplegia, ataxia, and areflexia. Few reports associate infliximab with MFS occurring days to weeks after biologic initiation, though the mechanism is unclear. While MFS due to anti-TNF therapy is uncommon, a high index of suspicion is needed when new neurologic symptoms develop during treatment, as neurologic decline can progress rapidly to respiratory compromise, emphasizing the need for early recognition and treatment.
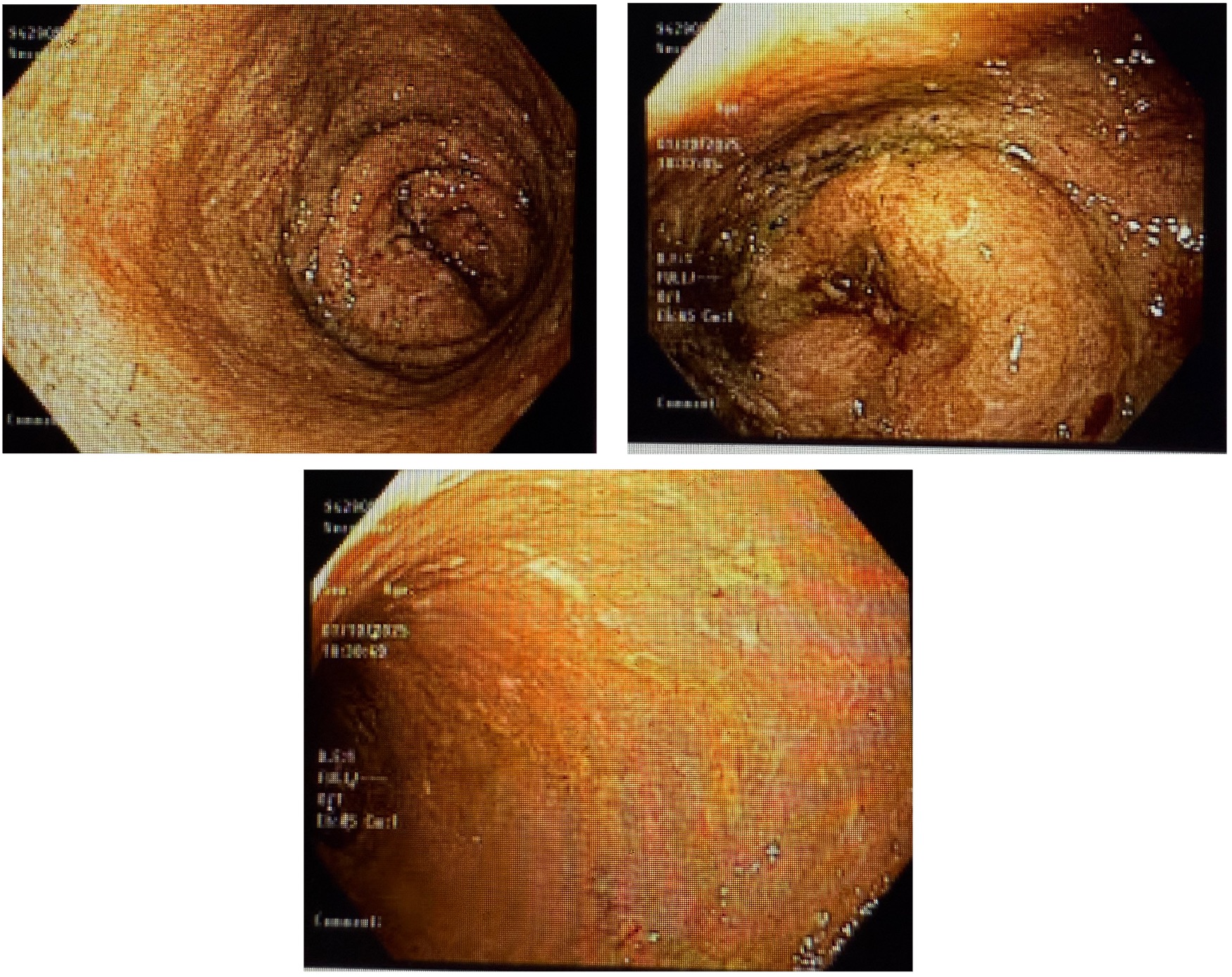
Figure: Representative images from flexible sigmoidoscopy showing severe ulcerative colitis (Mayo Score 2).
Disclosures:
Aastha Chokshi indicated no relevant financial relationships.
Dania Hudhud indicated no relevant financial relationships.
Ekta Gupta indicated no relevant financial relationships.
Aastha Chokshi, MD1, Dania Hudhud, MD2, Ekta Gupta, MD3. P1217 - Miller Fisher Syndrome: A Rare Manifestation of Anti-TNF Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Aastha Chokshi, MD1, Dania Hudhud, MD2, Ekta Gupta, MD3
1University of Maryland Medical Center, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD; 3University of Maryland, Balitmore, MD
Introduction: Infliximab, an anti-tumor necrosis factor (TNF) alpha inhibitor, is a commonly used biologic therapy for patients with inflammatory bowel disease (IBD). Neurologic complications, such as Guillain-Barré syndrome (GBS) and its variants, Miller Fisher syndrome (MFS), are rare side effects of anti-TNF inhibitors. We report a case of severe ulcerative colitis (UC) complicated by suspected infliximab-induced MFS, highlighting the importance of having a low threshold of suspicion in patients developing new neurological symptoms.
Case Description/
Methods: A 70-year-old male with a history of right hemicolectomy for cecal tubulovillous adenoma, COPD, OSA, and recently diagnosed ulcerative pancolitis presented with profuse watery diarrhea and abdominal pain. A year earlier, a colonoscopy showed chronic colitis, but treatment was deferred. Six months later, he was hospitalized for bloody diarrhea and started on steroids and mesalamine. He continued to have recurrent flares requiring steroids and therefore infliximab was initiated but discontinued after developing a drug-induced rash after the second dose.
During this admission, he tested positive for C. difficile PCR (toxin negative) and was treated with vancomycin and then fidaxomicin. Sigmoidoscopy showed severe UC (Mayo 2). IV steroids were started but discontinued after two days due to agitation. He received one induction dose of infliximab. Due to lack of clinical response with infliximab, he was switched to upadacitinib which he received for 2 days.
He then developed disorientation, slurred speech, and dysphagia requiring ICU admission and intubation. Imaging and CSF studies were unremarkable. On exam, he was disoriented, dysarthric, had upward gaze palsy, areflexic in lower extremities and hyporeflexic in upper extremities. He underwent urgent colectomy and was diagnosed with infliximab-induced MFS. He received IVIG with clinical improvement.
Discussion: This case highlights a rare but critical complication of biologic therapy in UC—suspected infliximab-induced MFS, characterized by ophthalmoplegia, ataxia, and areflexia. Few reports associate infliximab with MFS occurring days to weeks after biologic initiation, though the mechanism is unclear. While MFS due to anti-TNF therapy is uncommon, a high index of suspicion is needed when new neurologic symptoms develop during treatment, as neurologic decline can progress rapidly to respiratory compromise, emphasizing the need for early recognition and treatment.
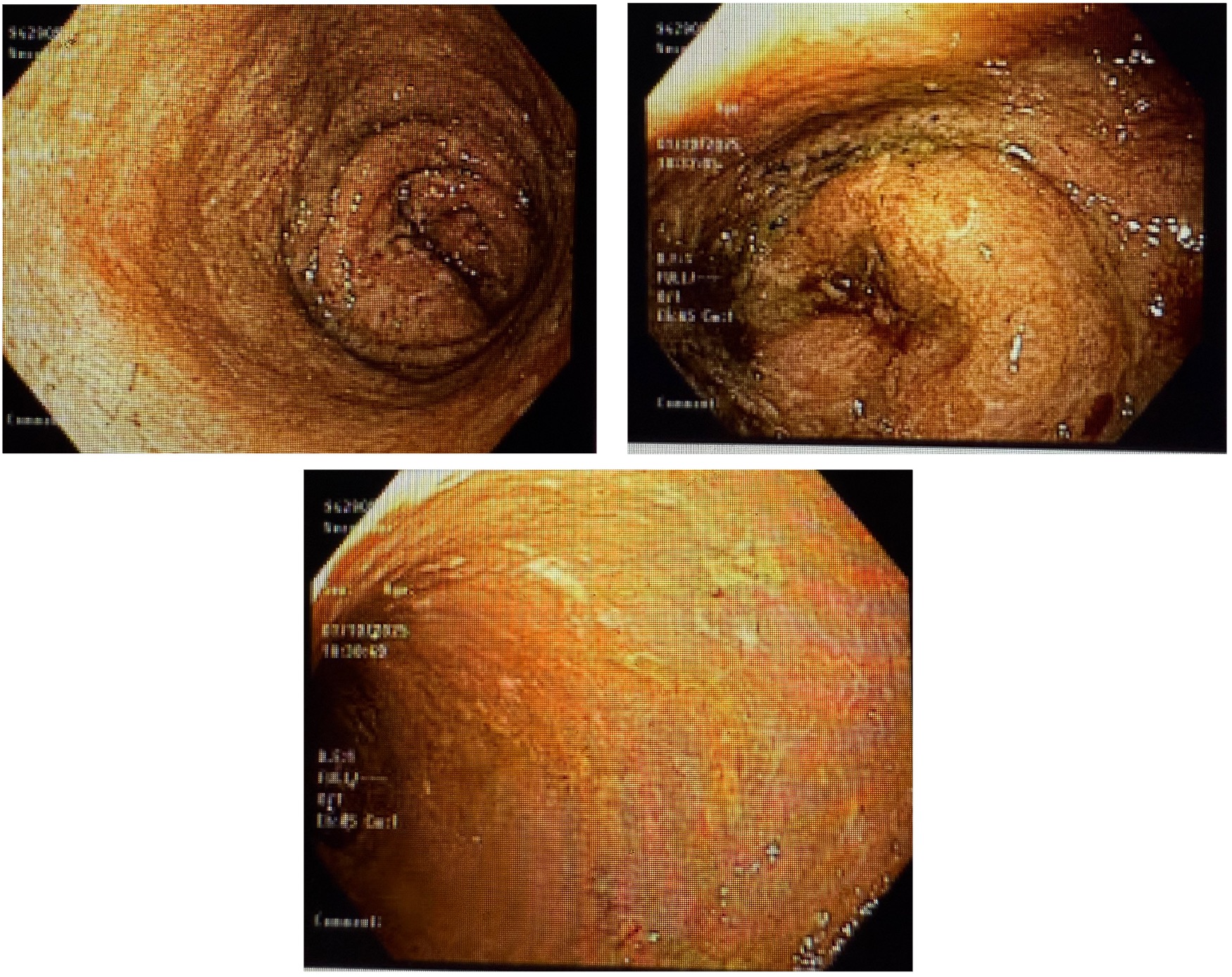
Figure: Representative images from flexible sigmoidoscopy showing severe ulcerative colitis (Mayo Score 2).
Disclosures:
Aastha Chokshi indicated no relevant financial relationships.
Dania Hudhud indicated no relevant financial relationships.
Ekta Gupta indicated no relevant financial relationships.
Aastha Chokshi, MD1, Dania Hudhud, MD2, Ekta Gupta, MD3. P1217 - Miller Fisher Syndrome: A Rare Manifestation of Anti-TNF Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

