Sunday Poster Session
Category: IBD
P1208 - Association Between Microscopic Colitis and Acute Pancreatitis: A Nationwide Inpatient Sample Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Gedion Yilma Amdetsion, MD (he/him/his)
Cook County Health
Chicago, IL
Presenting Author(s)
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Abhin Sapkota, MBBS3, Michael G. Tebeje, MD, MPH4, Shreyas Nandyal, MD1, Bhargav Koyani, MD5, Seema Gandhi, MD6
1Cook County Health, Chicago, IL; 2Washington University in St. Louis, Saint Louis, MO; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4Washington University in St. Louis, St. Louis, MO; 5Ascension Saint Francis Hospital, Evanston, IL; 6John H. Stroger Hospital of Cook Co, Chicago, IL
Introduction: Inflammatory bowel diseases (IBD) have long been associated with an increased risk of acute pancreatitis. However, the potential link between acute pancreatitis and microscopic colitis (MC), remains poorly understood. Given the shared immunopathogenic mechanisms with IBD and the increasing incidence of MC in older adults, this study aims to determine whether MC independently increases the odds of acute pancreatitis.
Methods: We conducted a retrospective analysis of adult (≥18 years) non-elective hospitalizations for acute pancreatitis using the 2017–2022 Nationwide Inpatient Sample (NIS). Acute pancreatitis and MC were identified using relevant ICD-10 codes. We also evaluated demographic covariates (age group, race/ethnicity, and median household income quartile) and clinical risk factors. The association between MC and acute pancreatitis was assessed using multivariable logistic regression.
Results: A total of 480,357 adult non-elective hospitalizations for acute pancreatitis were identified. The age distribution was 35.2% in the 18–44 years group, 38.8% in the 45–64 years group, and 26.0% in those aged ≥65 years. By race, 67.2% were White, 17.3% were Black, and 15.5% were Hispanic. Among the cohort, 47.0% were female. Common comorbidities included lipid disorders (33.5%), alcohol use (29.8%), gallstones (20.7%), and diabetes (14.6%). Microscopic colitis was rare, accounting for 0.04% of cases.
On multivariable logistic regression, adjusting for demographics, socioeconomic status, season of admission, and clinical risk factors, MC was independently associated with higher odds of acute pancreatitis (OR 2.96, p < 0.001).
By race, Black patients had a slight increase in odds versus White (OR 1.03, p = 0.002), and Hispanic patients had a more pronounced increase (OR 1.09, p < 0.001). Smoking was linked to higher odds (OR 1.76, p < 0.001), and diabetes conferred increased odds (OR 1.11, p < 0.001). Gallstone disease was the strongest predictor (OR 17.01, p < 0.001). Lipid disorders increased odds (OR 1.65, p < 0.001), and hypercalcemia nearly doubled odds (OR 2.02, p < 0.001).
Discussion: Microscopic colitis is rare among acute pancreatitis patients, yet its association is statistically significant. While budesonide use in MC treatment may contribute to pancreatitis, further research into the pathologic mechanisms underlying this association is warranted.
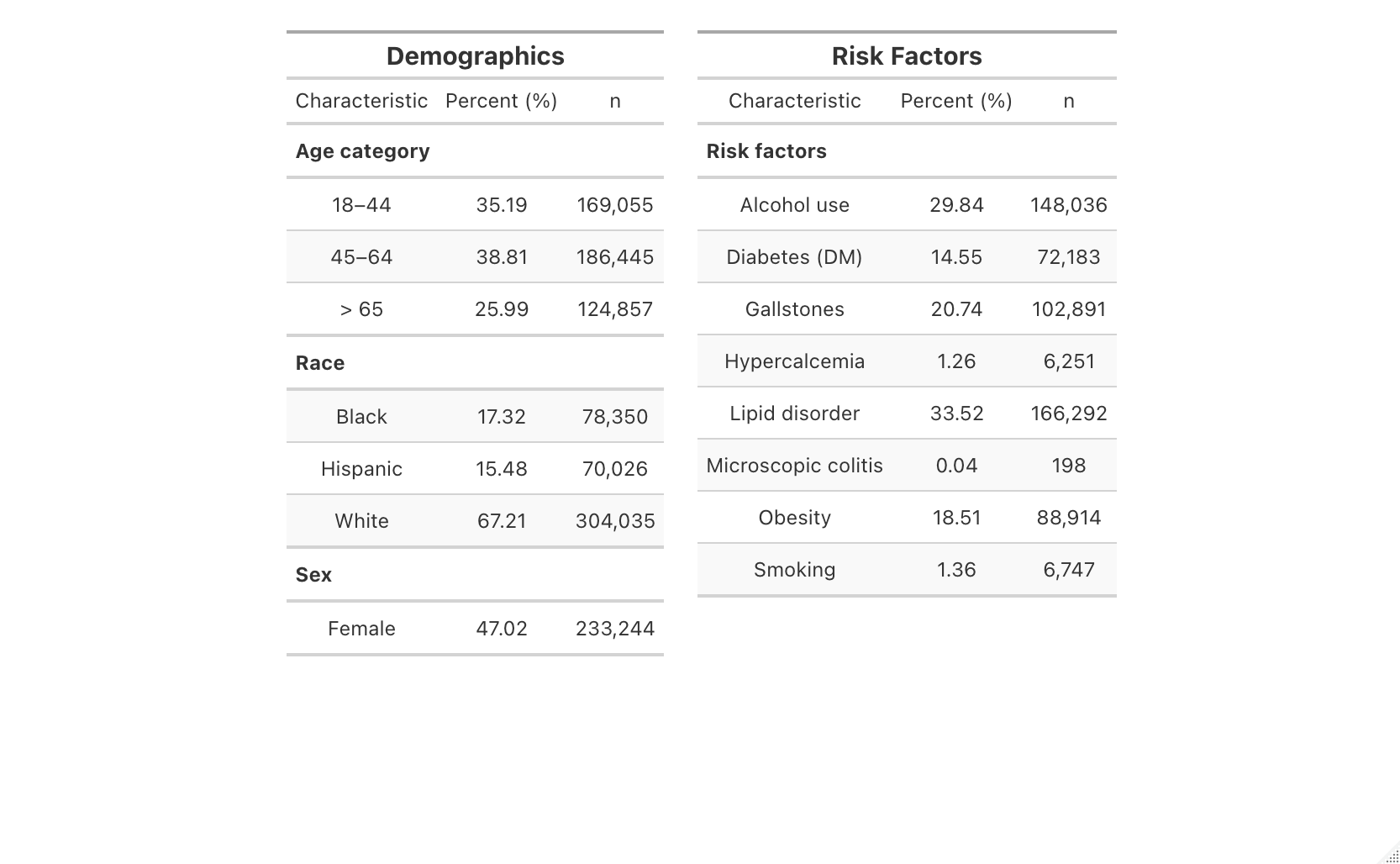
Figure: Fig. 1. Population characteristics of patients with Acute pancreatitis
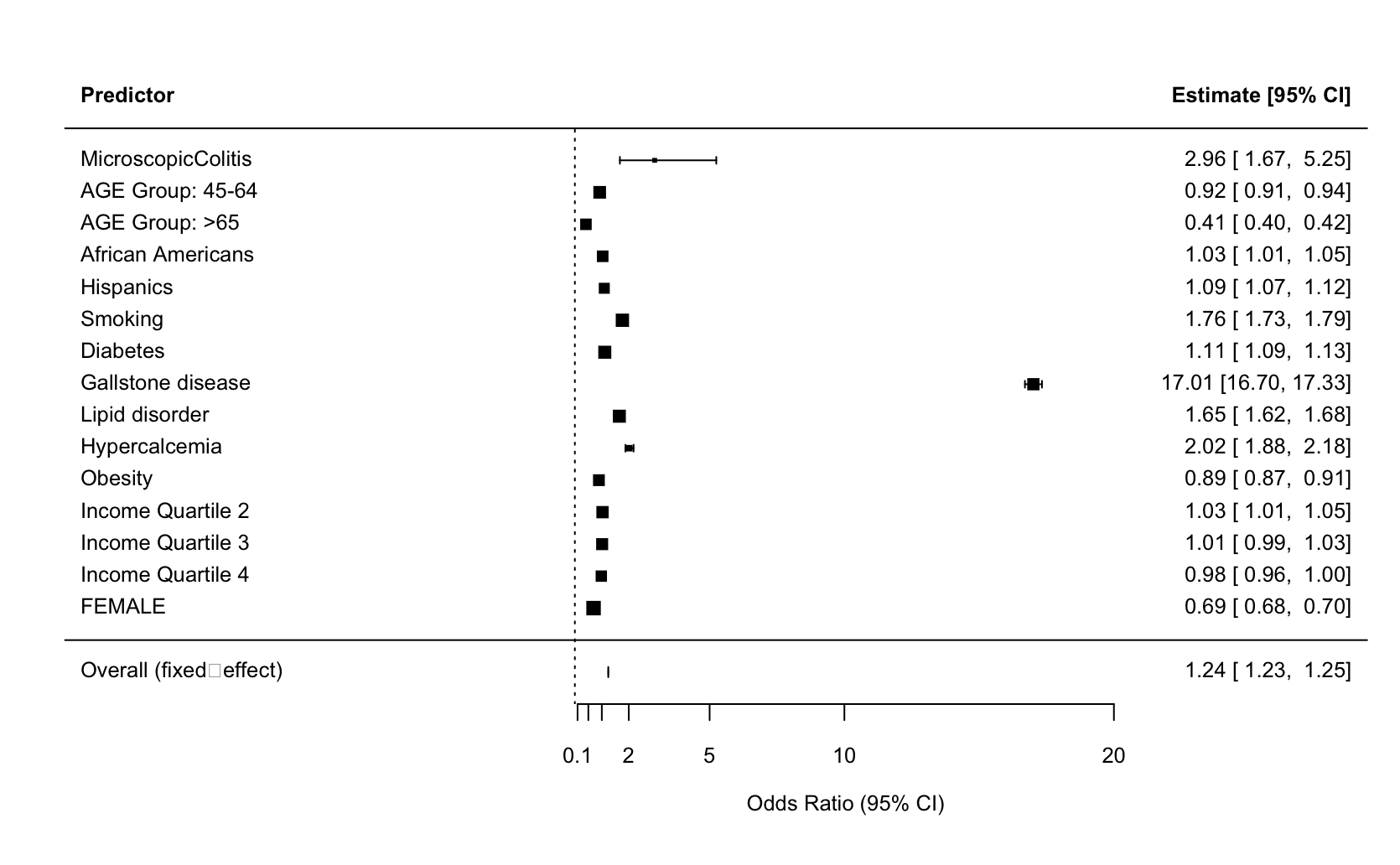
Figure: Fig. 2. Multivariate analysis of riskfactors for acute pancreatitis
Disclosures:
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Chun-wei Pan indicated no relevant financial relationships.
Hiwot Tebeje indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Michael Tebeje indicated no relevant financial relationships.
Shreyas Nandyal indicated no relevant financial relationships.
Bhargav Koyani indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Abhin Sapkota, MBBS3, Michael G. Tebeje, MD, MPH4, Shreyas Nandyal, MD1, Bhargav Koyani, MD5, Seema Gandhi, MD6. P1208 - Association Between Microscopic Colitis and Acute Pancreatitis: A Nationwide Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cook County Health, Chicago, IL; 2Washington University in St. Louis, Saint Louis, MO; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4Washington University in St. Louis, St. Louis, MO; 5Ascension Saint Francis Hospital, Evanston, IL; 6John H. Stroger Hospital of Cook Co, Chicago, IL
Introduction: Inflammatory bowel diseases (IBD) have long been associated with an increased risk of acute pancreatitis. However, the potential link between acute pancreatitis and microscopic colitis (MC), remains poorly understood. Given the shared immunopathogenic mechanisms with IBD and the increasing incidence of MC in older adults, this study aims to determine whether MC independently increases the odds of acute pancreatitis.
Methods: We conducted a retrospective analysis of adult (≥18 years) non-elective hospitalizations for acute pancreatitis using the 2017–2022 Nationwide Inpatient Sample (NIS). Acute pancreatitis and MC were identified using relevant ICD-10 codes. We also evaluated demographic covariates (age group, race/ethnicity, and median household income quartile) and clinical risk factors. The association between MC and acute pancreatitis was assessed using multivariable logistic regression.
Results: A total of 480,357 adult non-elective hospitalizations for acute pancreatitis were identified. The age distribution was 35.2% in the 18–44 years group, 38.8% in the 45–64 years group, and 26.0% in those aged ≥65 years. By race, 67.2% were White, 17.3% were Black, and 15.5% were Hispanic. Among the cohort, 47.0% were female. Common comorbidities included lipid disorders (33.5%), alcohol use (29.8%), gallstones (20.7%), and diabetes (14.6%). Microscopic colitis was rare, accounting for 0.04% of cases.
On multivariable logistic regression, adjusting for demographics, socioeconomic status, season of admission, and clinical risk factors, MC was independently associated with higher odds of acute pancreatitis (OR 2.96, p < 0.001).
By race, Black patients had a slight increase in odds versus White (OR 1.03, p = 0.002), and Hispanic patients had a more pronounced increase (OR 1.09, p < 0.001). Smoking was linked to higher odds (OR 1.76, p < 0.001), and diabetes conferred increased odds (OR 1.11, p < 0.001). Gallstone disease was the strongest predictor (OR 17.01, p < 0.001). Lipid disorders increased odds (OR 1.65, p < 0.001), and hypercalcemia nearly doubled odds (OR 2.02, p < 0.001).
Discussion: Microscopic colitis is rare among acute pancreatitis patients, yet its association is statistically significant. While budesonide use in MC treatment may contribute to pancreatitis, further research into the pathologic mechanisms underlying this association is warranted.
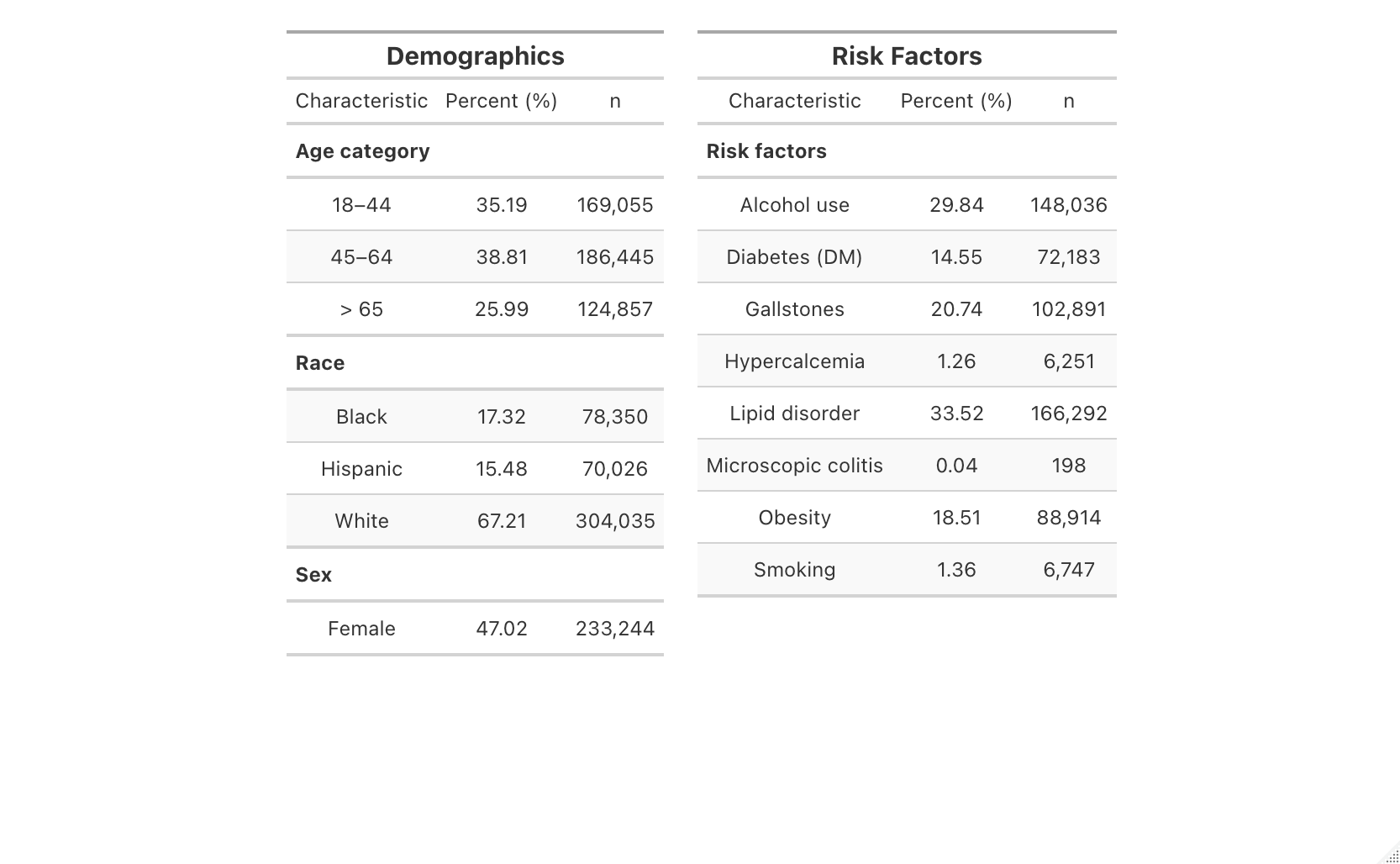
Figure: Fig. 1. Population characteristics of patients with Acute pancreatitis
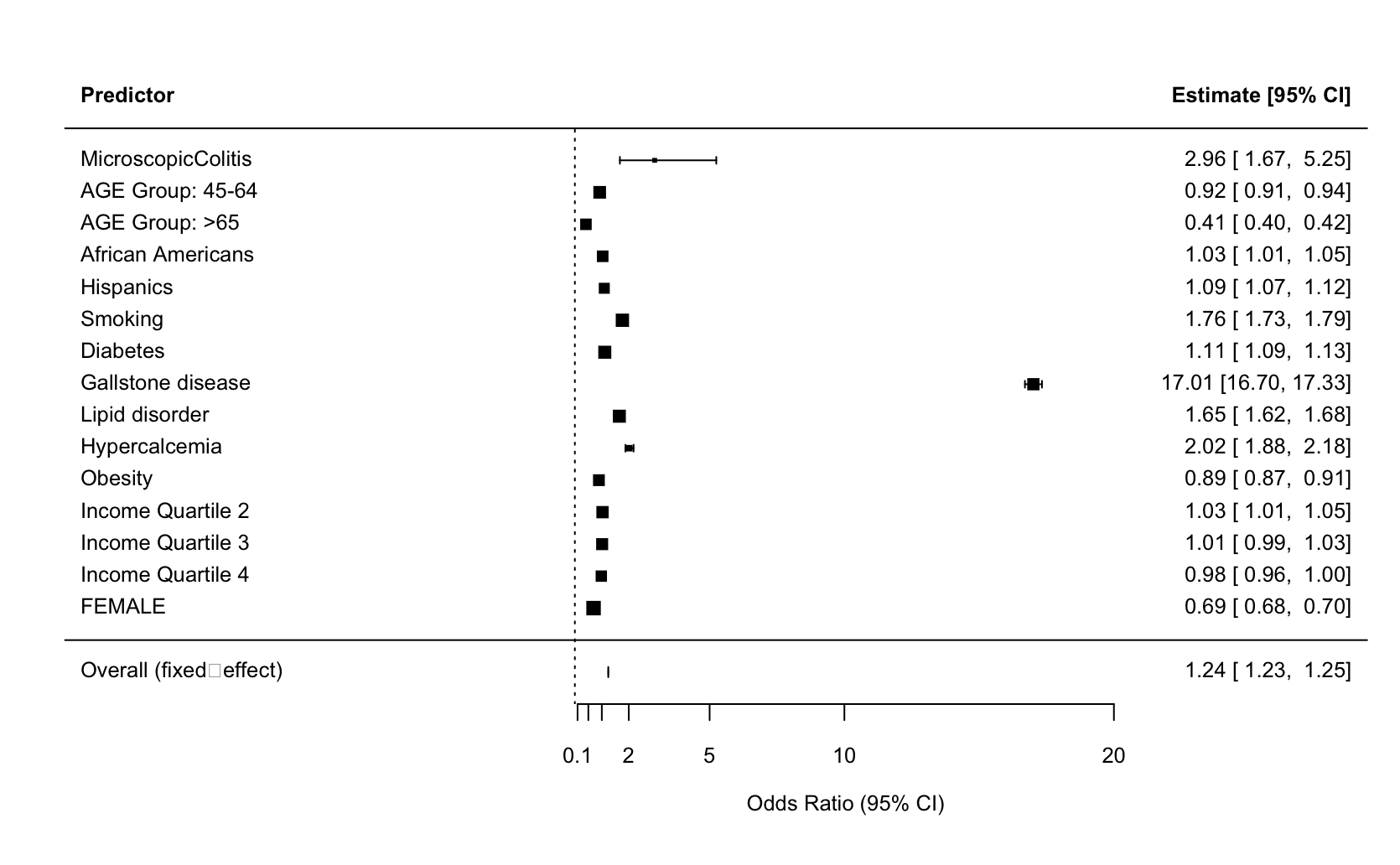
Figure: Fig. 2. Multivariate analysis of riskfactors for acute pancreatitis
Disclosures:
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Chun-wei Pan indicated no relevant financial relationships.
Hiwot Tebeje indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Michael Tebeje indicated no relevant financial relationships.
Shreyas Nandyal indicated no relevant financial relationships.
Bhargav Koyani indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Abhin Sapkota, MBBS3, Michael G. Tebeje, MD, MPH4, Shreyas Nandyal, MD1, Bhargav Koyani, MD5, Seema Gandhi, MD6. P1208 - Association Between Microscopic Colitis and Acute Pancreatitis: A Nationwide Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
