Sunday Poster Session
Category: IBD
P1207 - Seasonality and Risk of Hospitalization for Ulcerative Colitis: Insights From a National Inpatient Study (2017-2022)
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Gedion Yilma Amdetsion, MD (he/him/his)
Cook County Health
Chicago, IL
Presenting Author(s)
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Abhin Sapkota, MBBS3, Michael G. Tebeje, MD, MPH4, Shreyas Nandyal, MD1, Michael Shimelash, MD, MSc(Epi)5, Dusay Salih, MD6, Kajali Mishra, MD1
1Cook County Health, Chicago, IL; 2Washington University in St. Louis, Saint Louis, MO; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4Washington University in St. Louis, St. Louis, MO; 5University Medical Center Groningen, Groningen, Groningen, Netherlands; 6SBH Health System, Bronx, NY
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease, accounting for approximately 8 to 12 hospitalizations per 100,000 individuals annually. Known triggers for disease flares and admissions include medication nonadherence, smoking, dietary factors, infections, and NSAID use. However, the influence of seasonal variation on UC admissions remains uncertain, with prior studies showing conflicting results.
Methods: We analyzed adult non-elective hospitalizations for UC flares/complications using the Nationwide Inpatient Sample (NIS) from 2017 to 2022. Covariates assessed included demographic characteristics (age group, race, income quartile) and clinical risk factors (smoking, alcohol use, malnutrition, anemia, obesity, diabetes, and medication noncompliance). Multivariable logistic regression was performed to identify independent predictors of UC admission. A generalized additive model (GAM) was used to visualize seasonal trends in UC admissions.
Results: A total of 35,260 UC related admissions were identified. Admissions demonstrated a clear seasonal pattern, with peaks in July and August and the lowest rates in December. Compared to winter, flare admissions were significantly more likely in the Spring (OR 1.06, p=0.001), Summer (OR 1.12, p< 0.001), and Fall (OR 1.07, p< 0.001). This trend was supported by GAM visualization, showing a steady increase in admissions from January through August. Insurance status also showed strong associations: compared to Medicare, patients with private insurance had significantly higher odds of UC related admission (OR 1.74, p < 0.001), as did self-pay patients (OR 1.54, p < 0.001); Medicaid was not significantly different (OR 0.97, p = 0.123). Among clinical predictors, Malnutrition showed the strongest association, with a more than threefold increase in odds of UC flare (OR 3.41, p < 0.001), followed closely by anemia (OR 3.06, p < 0.001). Ethnicity was also associated with flare risk, with reduced odds observed in non-caucasians (OR 0.67, p < 0.001) relative to Caucasians.
Discussion: UC flare-related hospitalizations exhibit significant seasonal variation, with the lowest risk in winter and a pronounced increase during the summer months. These findings highlight the need for further investigation into environmental triggers and strategies to mitigate flare risk through targeted public health and clinical interventions.
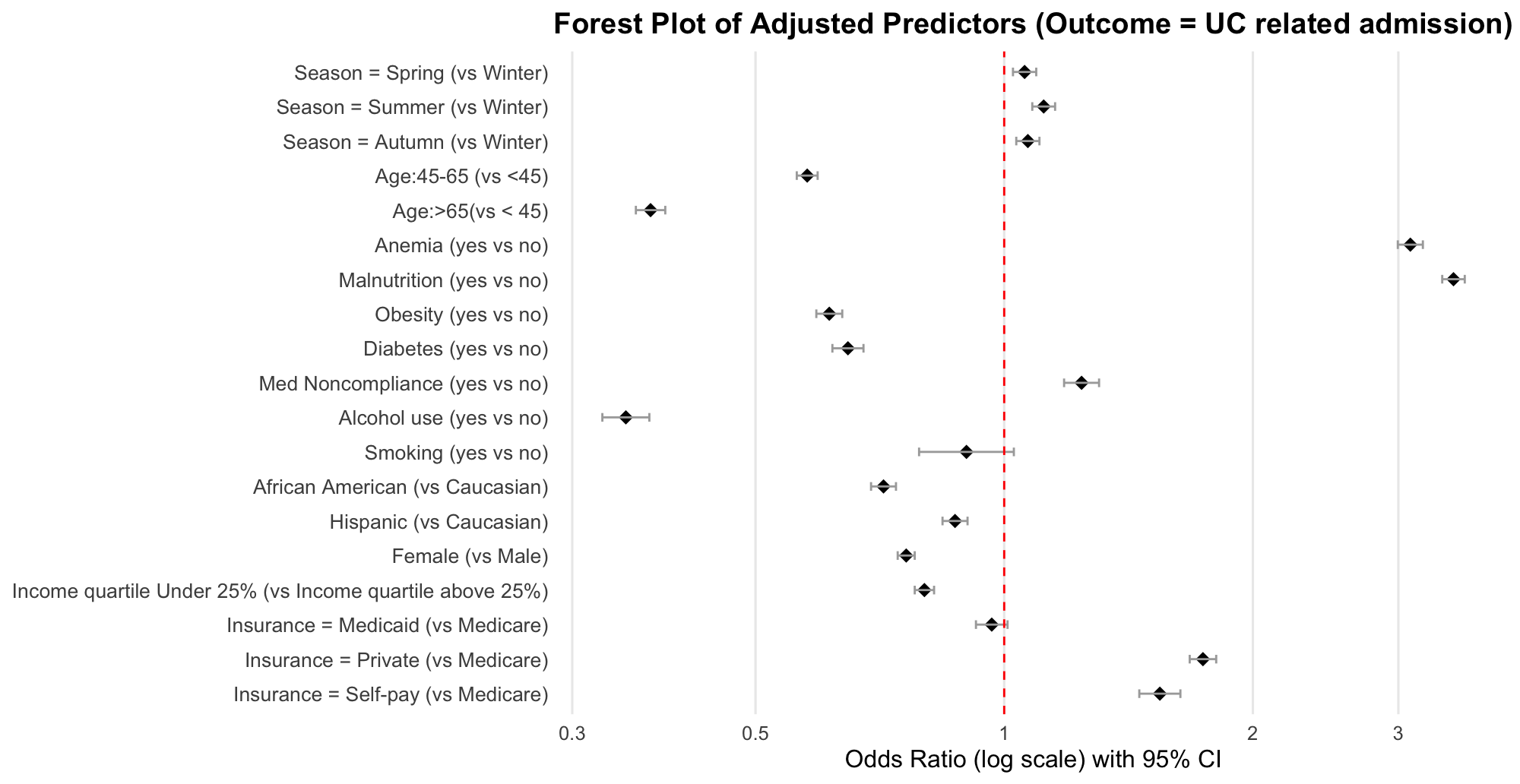
Figure: Fig. 1. Forest Plot of Adjusted Predictors for UC related admission

Figure: Fig. 2 GAM showing trend in UC flare admission
Disclosures:
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Chun-wei Pan indicated no relevant financial relationships.
Hiwot Tebeje indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Michael Tebeje indicated no relevant financial relationships.
Shreyas Nandyal indicated no relevant financial relationships.
Michael Shimelash indicated no relevant financial relationships.
Dusay Salih indicated no relevant financial relationships.
Kajali Mishra indicated no relevant financial relationships.
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Abhin Sapkota, MBBS3, Michael G. Tebeje, MD, MPH4, Shreyas Nandyal, MD1, Michael Shimelash, MD, MSc(Epi)5, Dusay Salih, MD6, Kajali Mishra, MD1. P1207 - Seasonality and Risk of Hospitalization for Ulcerative Colitis: Insights From a National Inpatient Study (2017-2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cook County Health, Chicago, IL; 2Washington University in St. Louis, Saint Louis, MO; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4Washington University in St. Louis, St. Louis, MO; 5University Medical Center Groningen, Groningen, Groningen, Netherlands; 6SBH Health System, Bronx, NY
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease, accounting for approximately 8 to 12 hospitalizations per 100,000 individuals annually. Known triggers for disease flares and admissions include medication nonadherence, smoking, dietary factors, infections, and NSAID use. However, the influence of seasonal variation on UC admissions remains uncertain, with prior studies showing conflicting results.
Methods: We analyzed adult non-elective hospitalizations for UC flares/complications using the Nationwide Inpatient Sample (NIS) from 2017 to 2022. Covariates assessed included demographic characteristics (age group, race, income quartile) and clinical risk factors (smoking, alcohol use, malnutrition, anemia, obesity, diabetes, and medication noncompliance). Multivariable logistic regression was performed to identify independent predictors of UC admission. A generalized additive model (GAM) was used to visualize seasonal trends in UC admissions.
Results: A total of 35,260 UC related admissions were identified. Admissions demonstrated a clear seasonal pattern, with peaks in July and August and the lowest rates in December. Compared to winter, flare admissions were significantly more likely in the Spring (OR 1.06, p=0.001), Summer (OR 1.12, p< 0.001), and Fall (OR 1.07, p< 0.001). This trend was supported by GAM visualization, showing a steady increase in admissions from January through August. Insurance status also showed strong associations: compared to Medicare, patients with private insurance had significantly higher odds of UC related admission (OR 1.74, p < 0.001), as did self-pay patients (OR 1.54, p < 0.001); Medicaid was not significantly different (OR 0.97, p = 0.123). Among clinical predictors, Malnutrition showed the strongest association, with a more than threefold increase in odds of UC flare (OR 3.41, p < 0.001), followed closely by anemia (OR 3.06, p < 0.001). Ethnicity was also associated with flare risk, with reduced odds observed in non-caucasians (OR 0.67, p < 0.001) relative to Caucasians.
Discussion: UC flare-related hospitalizations exhibit significant seasonal variation, with the lowest risk in winter and a pronounced increase during the summer months. These findings highlight the need for further investigation into environmental triggers and strategies to mitigate flare risk through targeted public health and clinical interventions.
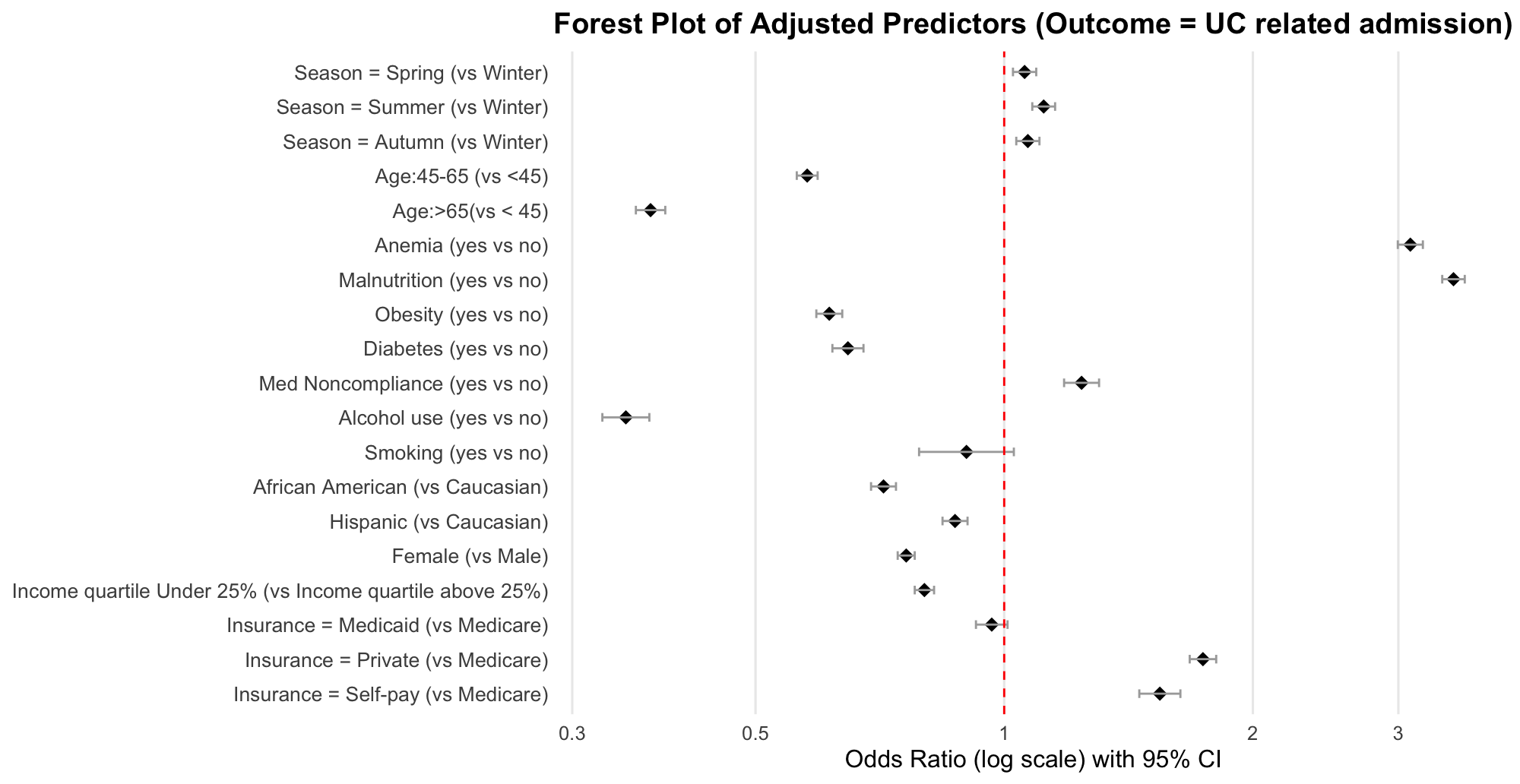
Figure: Fig. 1. Forest Plot of Adjusted Predictors for UC related admission

Figure: Fig. 2 GAM showing trend in UC flare admission
Disclosures:
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Chun-wei Pan indicated no relevant financial relationships.
Hiwot Tebeje indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Michael Tebeje indicated no relevant financial relationships.
Shreyas Nandyal indicated no relevant financial relationships.
Michael Shimelash indicated no relevant financial relationships.
Dusay Salih indicated no relevant financial relationships.
Kajali Mishra indicated no relevant financial relationships.
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Abhin Sapkota, MBBS3, Michael G. Tebeje, MD, MPH4, Shreyas Nandyal, MD1, Michael Shimelash, MD, MSc(Epi)5, Dusay Salih, MD6, Kajali Mishra, MD1. P1207 - Seasonality and Risk of Hospitalization for Ulcerative Colitis: Insights From a National Inpatient Study (2017-2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

