Sunday Poster Session
Category: IBD
P1183 - Comparative Effectiveness of Statins in Inflammatory Bowel Disease: A Propensity Score-Matched Real-World Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- YA
Yazan Al Jabiri, MD
Washington University School of Medicine in St. Louis
St. Louis, MO
Presenting Author(s)
Yazan Al Jabiri, MD1, Mohammad Aldiabat, MD1, Andres Yarur, MD2, Parakkal Deepak, 3
1Washington University School of Medicine in St. Louis, St. Louis, MO; 2Cedars-Sinai Medical Center, Los Angeles, CA; 3Department of Medicine, Washington University School of Medicine, St. Louis, MO
Introduction: While statins are known for their cardioprotective benefits, limited data exist comparing individual agents within the same intensity class in patients with Inflammatory Bowel Disease (IBD). This study assessed the comparative effectiveness of rosuvastatin and atorvastatin (high-intensity statins), as well as simvastatin and pravastatin (low-/moderate-intensity statins), on mortality and acute arterial events, including Atherosclerotic Cardiovascular Disease (ASCVD)—which comprises Coronary Heart Disease (CHD) and Cerebrovascular Disease (CVD)—and Peripheral Arterial Disease (PAD), among patients with IBD, Crohn’s disease (CD), and ulcerative colitis (UC).
Methods: This retrospective, propensity score–matched cohort study utilized real-world data to compare rosuvastatin with atorvastatin and simvastatin with pravastatin across IBD, CD, and UC populations. Patients were matched on demographics, components of the Charlson Comorbidity Index, indicators of IBD severity, and ASCVD risk factors. Cox proportional hazards models were used to estimate hazard ratios (HRs) for all-cause mortality, CVD, CHD, and PAD
Results: Among high-intensity statins, rosuvastatin was associated with significantly lower all-cause mortality compared to atorvastatin in IBD (HR 0.73, p< 0.001), CD (HR 0.70, p< 0.001), and UC (HR 0.70, p< 0.001). Rosuvastatin also conferred greater reduction in CVD, CHD, and showed a non-significant trend toward lower PAD. Additionally, rosuvastatin was associated with a significantly lower risk of composite ASCVD outcomes in IBD (HR 0.65), CD (HR 0.61), and UC (HR 0.67), all p< 0.001. In the low-/moderate-intensity group, all-cause mortality was similar between simvastatin and pravastatin in IBD (HR 0.97, p=0.53), CD (HR 1.04, p=0.61), and UC (HR 0.97, p=0.54), though simvastatin was associated with modest improvements in CVD and CHD outcomes, as well as significantly lower composite ASCVD outcomes in IBD (HR 0.74), CD (HR 0.70), and UC (HR 0.79), all p< 0.001.
Discussion: In this real-world analysis, rosuvastatin was more effective than atorvastatin in reducing all-cause mortality and acute arterial events—including composite ASCVD outcomes—in IBD patients. Simvastatin and pravastatin demonstrated comparable all-cause mortality outcomes, with a possible vascular benefit favoring simvastatin, including significantly lower composite ASCVD risks. These within-class differences may guide statin selection in IBD patients with elevated cardiovascular risk.
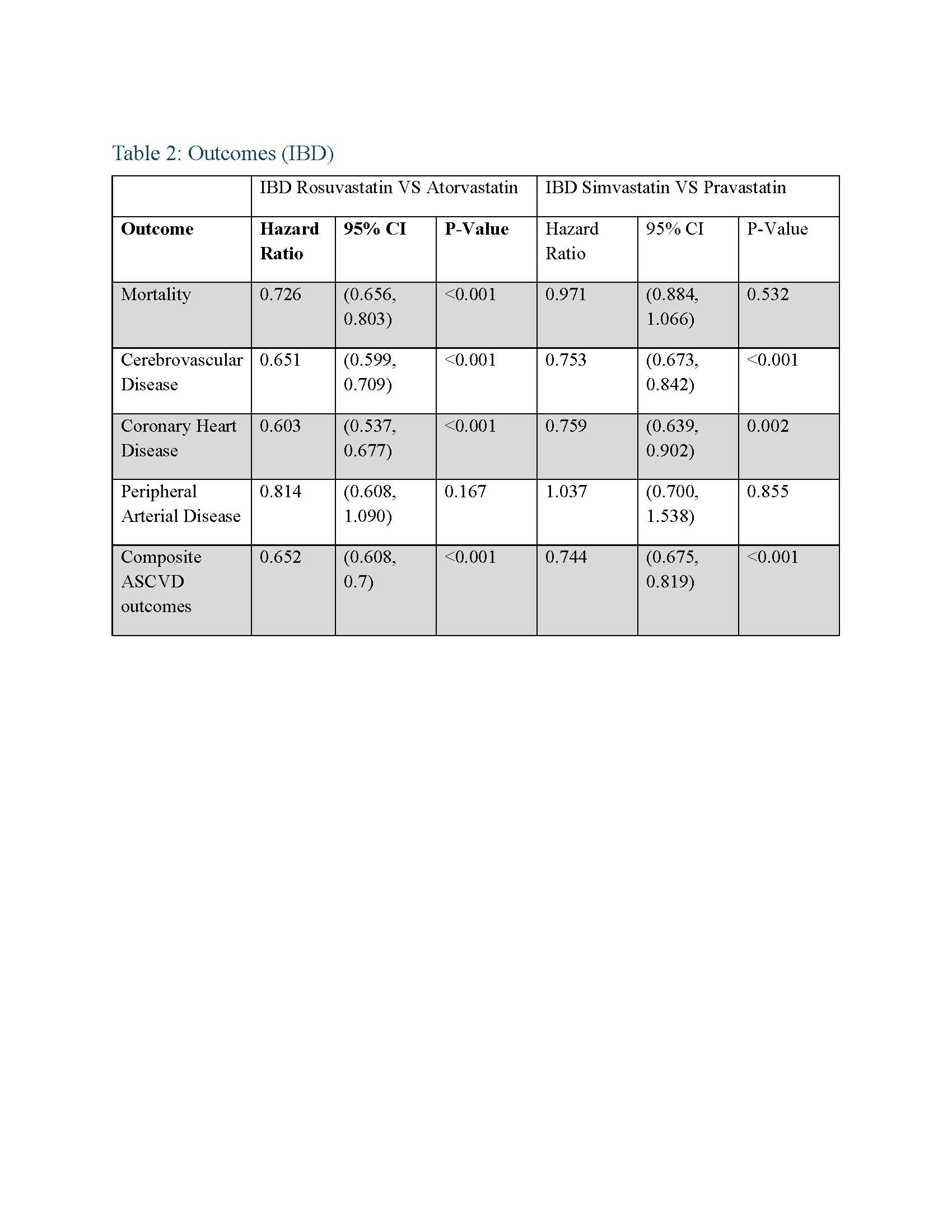
Figure: Tables 1: Baseline characteristics
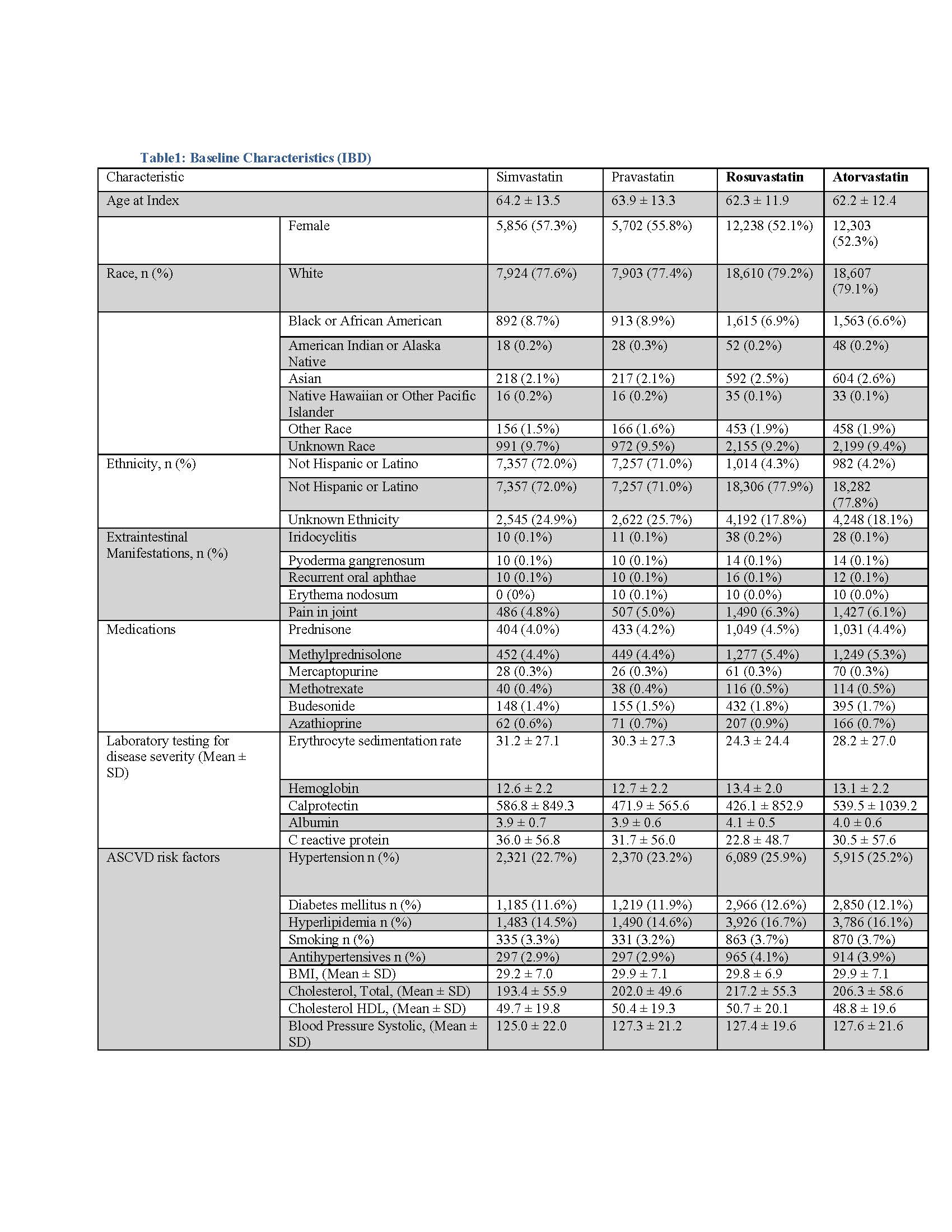
Figure: Tables 2: Outcomes
Disclosures:
Yazan Al Jabiri indicated no relevant financial relationships.
Mohammad Aldiabat indicated no relevant financial relationships.
Andres Yarur indicated no relevant financial relationships.
Parakkal Deepak: Arena Pharmaceuticals – Grant/Research Support, Personal or other fees. Boehringer Ingelheim – Grant/Research Support, Personal or other fees. Bristol Myers Squibb/Celgene – Grant/Research Support, Personal or other fees. Janssen – Grant/Research Support, Personal or other fees. Pfizer – Grant/Research Support, Personal or other fees. Prometheus Biosciences – Grant/Research Support, Personal or other fees. Takeda – Grant/Research Support, Personal or other fees.
Yazan Al Jabiri, MD1, Mohammad Aldiabat, MD1, Andres Yarur, MD2, Parakkal Deepak, 3. P1183 - Comparative Effectiveness of Statins in Inflammatory Bowel Disease: A Propensity Score-Matched Real-World Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Washington University School of Medicine in St. Louis, St. Louis, MO; 2Cedars-Sinai Medical Center, Los Angeles, CA; 3Department of Medicine, Washington University School of Medicine, St. Louis, MO
Introduction: While statins are known for their cardioprotective benefits, limited data exist comparing individual agents within the same intensity class in patients with Inflammatory Bowel Disease (IBD). This study assessed the comparative effectiveness of rosuvastatin and atorvastatin (high-intensity statins), as well as simvastatin and pravastatin (low-/moderate-intensity statins), on mortality and acute arterial events, including Atherosclerotic Cardiovascular Disease (ASCVD)—which comprises Coronary Heart Disease (CHD) and Cerebrovascular Disease (CVD)—and Peripheral Arterial Disease (PAD), among patients with IBD, Crohn’s disease (CD), and ulcerative colitis (UC).
Methods: This retrospective, propensity score–matched cohort study utilized real-world data to compare rosuvastatin with atorvastatin and simvastatin with pravastatin across IBD, CD, and UC populations. Patients were matched on demographics, components of the Charlson Comorbidity Index, indicators of IBD severity, and ASCVD risk factors. Cox proportional hazards models were used to estimate hazard ratios (HRs) for all-cause mortality, CVD, CHD, and PAD
Results: Among high-intensity statins, rosuvastatin was associated with significantly lower all-cause mortality compared to atorvastatin in IBD (HR 0.73, p< 0.001), CD (HR 0.70, p< 0.001), and UC (HR 0.70, p< 0.001). Rosuvastatin also conferred greater reduction in CVD, CHD, and showed a non-significant trend toward lower PAD. Additionally, rosuvastatin was associated with a significantly lower risk of composite ASCVD outcomes in IBD (HR 0.65), CD (HR 0.61), and UC (HR 0.67), all p< 0.001. In the low-/moderate-intensity group, all-cause mortality was similar between simvastatin and pravastatin in IBD (HR 0.97, p=0.53), CD (HR 1.04, p=0.61), and UC (HR 0.97, p=0.54), though simvastatin was associated with modest improvements in CVD and CHD outcomes, as well as significantly lower composite ASCVD outcomes in IBD (HR 0.74), CD (HR 0.70), and UC (HR 0.79), all p< 0.001.
Discussion: In this real-world analysis, rosuvastatin was more effective than atorvastatin in reducing all-cause mortality and acute arterial events—including composite ASCVD outcomes—in IBD patients. Simvastatin and pravastatin demonstrated comparable all-cause mortality outcomes, with a possible vascular benefit favoring simvastatin, including significantly lower composite ASCVD risks. These within-class differences may guide statin selection in IBD patients with elevated cardiovascular risk.
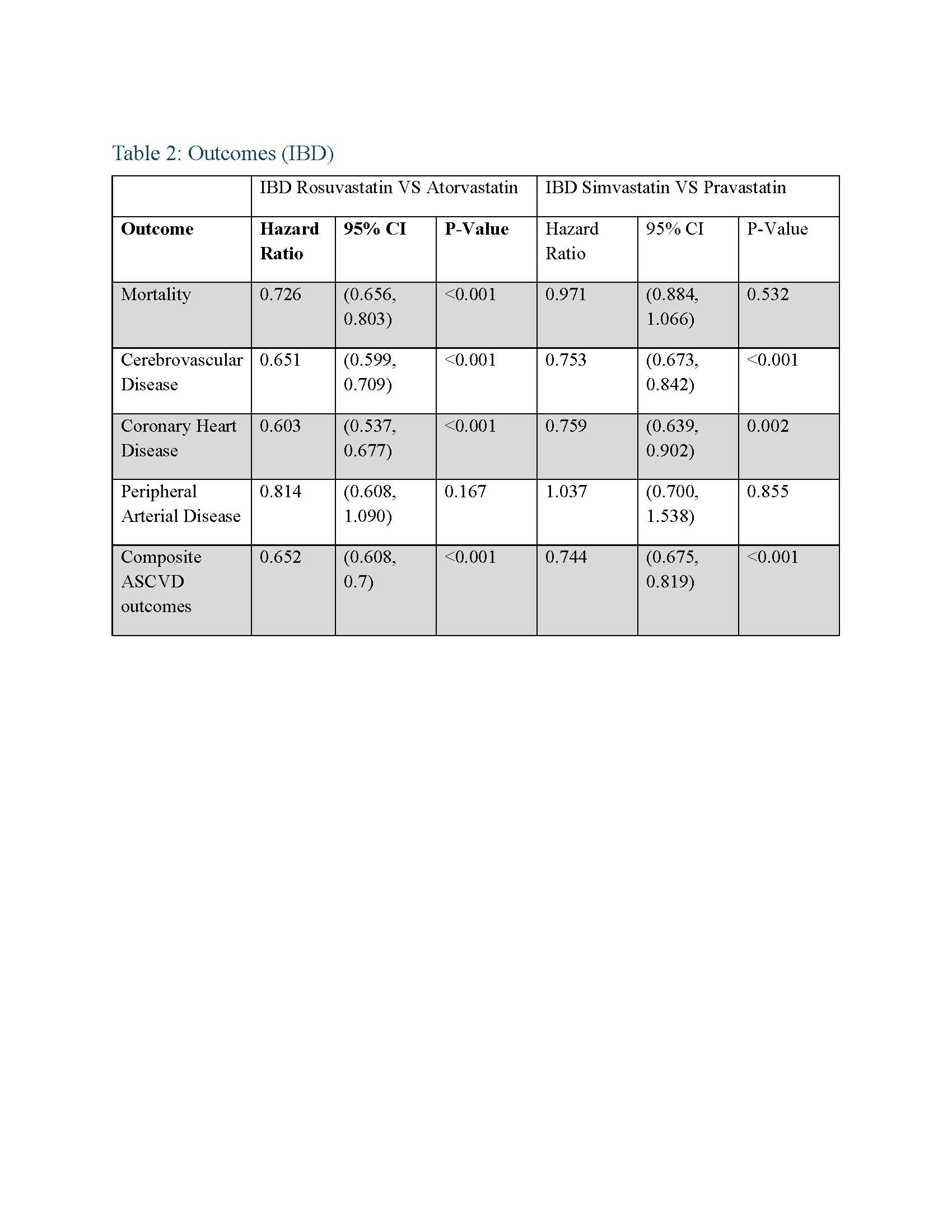
Figure: Tables 1: Baseline characteristics
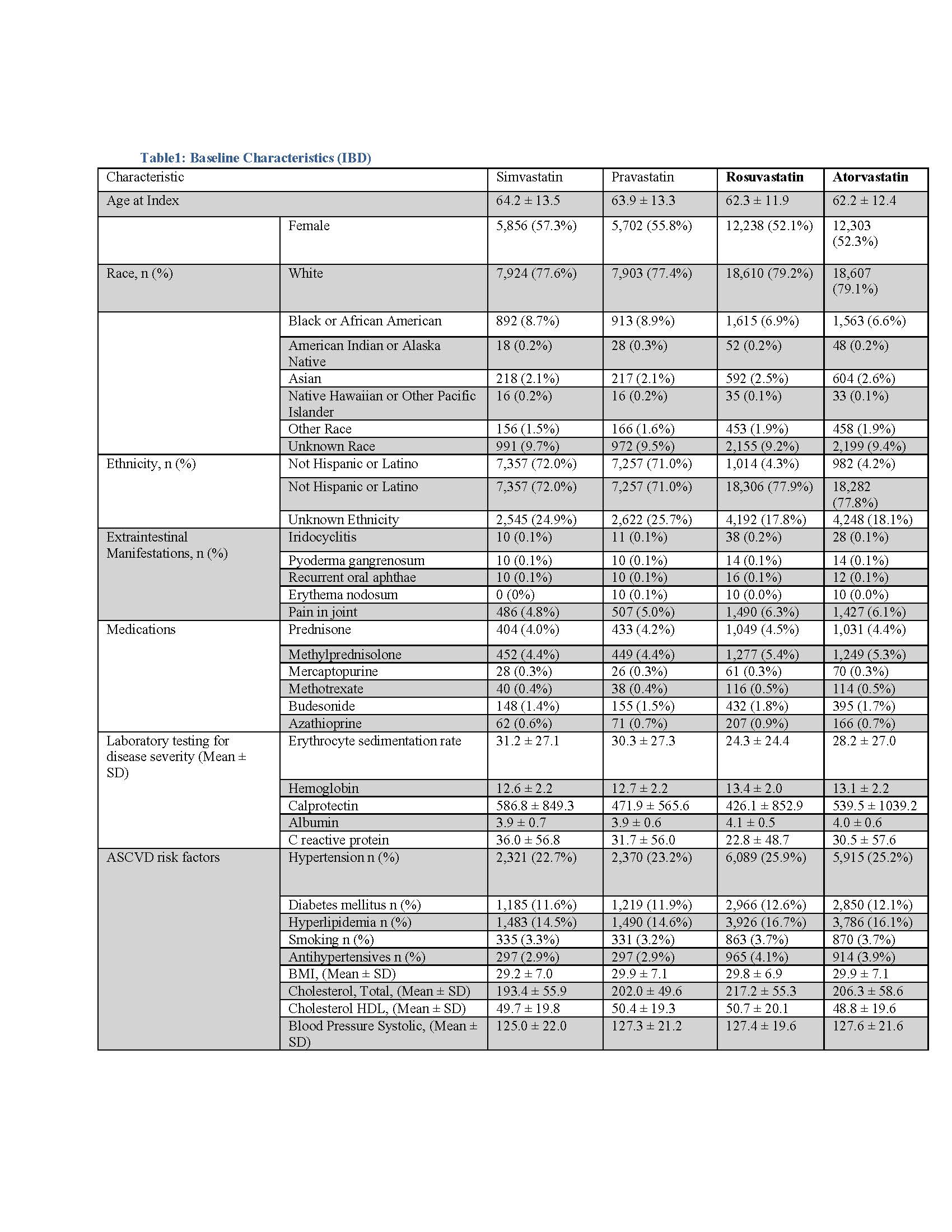
Figure: Tables 2: Outcomes
Disclosures:
Yazan Al Jabiri indicated no relevant financial relationships.
Mohammad Aldiabat indicated no relevant financial relationships.
Andres Yarur indicated no relevant financial relationships.
Parakkal Deepak: Arena Pharmaceuticals – Grant/Research Support, Personal or other fees. Boehringer Ingelheim – Grant/Research Support, Personal or other fees. Bristol Myers Squibb/Celgene – Grant/Research Support, Personal or other fees. Janssen – Grant/Research Support, Personal or other fees. Pfizer – Grant/Research Support, Personal or other fees. Prometheus Biosciences – Grant/Research Support, Personal or other fees. Takeda – Grant/Research Support, Personal or other fees.
Yazan Al Jabiri, MD1, Mohammad Aldiabat, MD1, Andres Yarur, MD2, Parakkal Deepak, 3. P1183 - Comparative Effectiveness of Statins in Inflammatory Bowel Disease: A Propensity Score-Matched Real-World Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
