Sunday Poster Session
Category: IBD
P1159 - Predictors of Risk of Lymphoma in IBD Patients With Thiopurine Use: A Retrospective TrinetX Based Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Shivam Kalra, MBBS, MHA (he/him/his)
Trident Medical Center
North Charleston, SC
Presenting Author(s)
Shivam Kalra, MBBS, MHA1, Rishi Chowdhary, MD2, Manjeet Kumar Goyal, MBBS, MD, DM, DNB3, Maitri Shah, MD4, Ashujot K. Dang, MD5, Anmol Singh, MD6, Kirti Arora, MD3, Amaninder Dhaliwal, MD7
1Trident Medical Center, North Charleston, SC; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3Cleveland Clinic Akron General, Akron, OH; 4University of Michigan Health - Sparrow, Lansing, MI; 5University of California Riverside School of Medicine, Riverside, CA; 6Cook County Health, Chicago, IL; 7University of South Carolina School of Medicine, Florence, SC
Introduction: Thiopurines (Azathioprine and Mercaptopurine) are effective for maintenance of remission in ulcerative colitis, particularly in patients who are steroid-dependent or intolerant to mesalamine. The risk of developing lymphoma in patients with ulcerative colitis treated with thiopurines is increased.
Methods: We performed a retrospective cohort study via TriNetX, with two cohorts using the platform: patients with ulcerative colitis who received thiopurines, and those with UC who had no record of thiopurine use. We excluded patients with a prior history of lymphoma, crohn’s disease, HIV infection, organ transplantation, and other biologic use. Only adults aged ≥18 years were included. Propensity score matching (1:1) balanced baseline covariates (age, sex, disease duration, co-medications) between exposed and unexposed groups. The primary outcome was incident lymphoma (any subtype) after UC diagnosis. Time-to-event analyses were used to compare lymphoma risk, yielding hazard ratios (HR) with 95% confidence intervals (CI).
Results: In a matched cohort of 13,562 ulcerative colitis patients with thiopurine exposure and 13,567 unexposed patients, lymphoma occurred in 23 and 11 cases, respectively. Kaplan-Meier analysis showed high 5-year lymphoma-free survival probabilities (98.49% vs. 99.84%), with median survival not reached in either group. The log-rank test (χ²=2.053, p=0.152) and hazard ratio (HR=1.68, 95% CI:0.82–3.46; p=0.066) indicated no statistically significant increased lymphoma risk with thiopurines, though a numerical trend toward higher risk was observed. Lymphoma risk was doubled in thiopurine group (0.4% vs 0.2%, HR 1.6, p=0.047).
Discussion: Thiopurines (azathioprine and mercaptopurine) are effective for maintenance of remission in ulcerative colitis, particularly in patients who are steroid-dependent or intolerant to mesalamine. This risk is highest during active therapy and decreases after discontinuation. Hence, Careful patient selection and monitoring are essential: pre-treatment screening for TPMT and NUDT15 deficiency is recommended to reduce the risk of myelosuppression, and ongoing monitoring for cytopenias, hepatotoxicity, and malignancy is required.
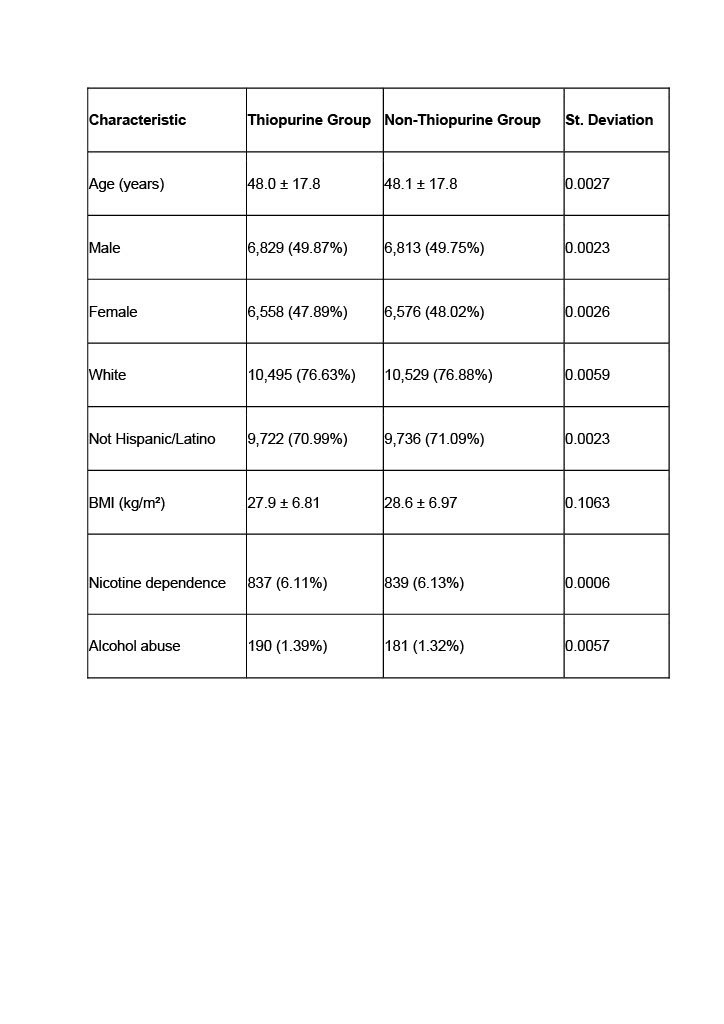
Figure: Patient Demographics and Characteristics stratified by thiopurine use
Disclosures:
Shivam Kalra indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Manjeet Kumar Goyal indicated no relevant financial relationships.
Maitri Shah indicated no relevant financial relationships.
Ashujot Dang indicated no relevant financial relationships.
Anmol Singh indicated no relevant financial relationships.
Kirti Arora indicated no relevant financial relationships.
Amaninder Dhaliwal indicated no relevant financial relationships.
Shivam Kalra, MBBS, MHA1, Rishi Chowdhary, MD2, Manjeet Kumar Goyal, MBBS, MD, DM, DNB3, Maitri Shah, MD4, Ashujot K. Dang, MD5, Anmol Singh, MD6, Kirti Arora, MD3, Amaninder Dhaliwal, MD7. P1159 - Predictors of Risk of Lymphoma in IBD Patients With Thiopurine Use: A Retrospective TrinetX Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Trident Medical Center, North Charleston, SC; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3Cleveland Clinic Akron General, Akron, OH; 4University of Michigan Health - Sparrow, Lansing, MI; 5University of California Riverside School of Medicine, Riverside, CA; 6Cook County Health, Chicago, IL; 7University of South Carolina School of Medicine, Florence, SC
Introduction: Thiopurines (Azathioprine and Mercaptopurine) are effective for maintenance of remission in ulcerative colitis, particularly in patients who are steroid-dependent or intolerant to mesalamine. The risk of developing lymphoma in patients with ulcerative colitis treated with thiopurines is increased.
Methods: We performed a retrospective cohort study via TriNetX, with two cohorts using the platform: patients with ulcerative colitis who received thiopurines, and those with UC who had no record of thiopurine use. We excluded patients with a prior history of lymphoma, crohn’s disease, HIV infection, organ transplantation, and other biologic use. Only adults aged ≥18 years were included. Propensity score matching (1:1) balanced baseline covariates (age, sex, disease duration, co-medications) between exposed and unexposed groups. The primary outcome was incident lymphoma (any subtype) after UC diagnosis. Time-to-event analyses were used to compare lymphoma risk, yielding hazard ratios (HR) with 95% confidence intervals (CI).
Results: In a matched cohort of 13,562 ulcerative colitis patients with thiopurine exposure and 13,567 unexposed patients, lymphoma occurred in 23 and 11 cases, respectively. Kaplan-Meier analysis showed high 5-year lymphoma-free survival probabilities (98.49% vs. 99.84%), with median survival not reached in either group. The log-rank test (χ²=2.053, p=0.152) and hazard ratio (HR=1.68, 95% CI:0.82–3.46; p=0.066) indicated no statistically significant increased lymphoma risk with thiopurines, though a numerical trend toward higher risk was observed. Lymphoma risk was doubled in thiopurine group (0.4% vs 0.2%, HR 1.6, p=0.047).
Discussion: Thiopurines (azathioprine and mercaptopurine) are effective for maintenance of remission in ulcerative colitis, particularly in patients who are steroid-dependent or intolerant to mesalamine. This risk is highest during active therapy and decreases after discontinuation. Hence, Careful patient selection and monitoring are essential: pre-treatment screening for TPMT and NUDT15 deficiency is recommended to reduce the risk of myelosuppression, and ongoing monitoring for cytopenias, hepatotoxicity, and malignancy is required.
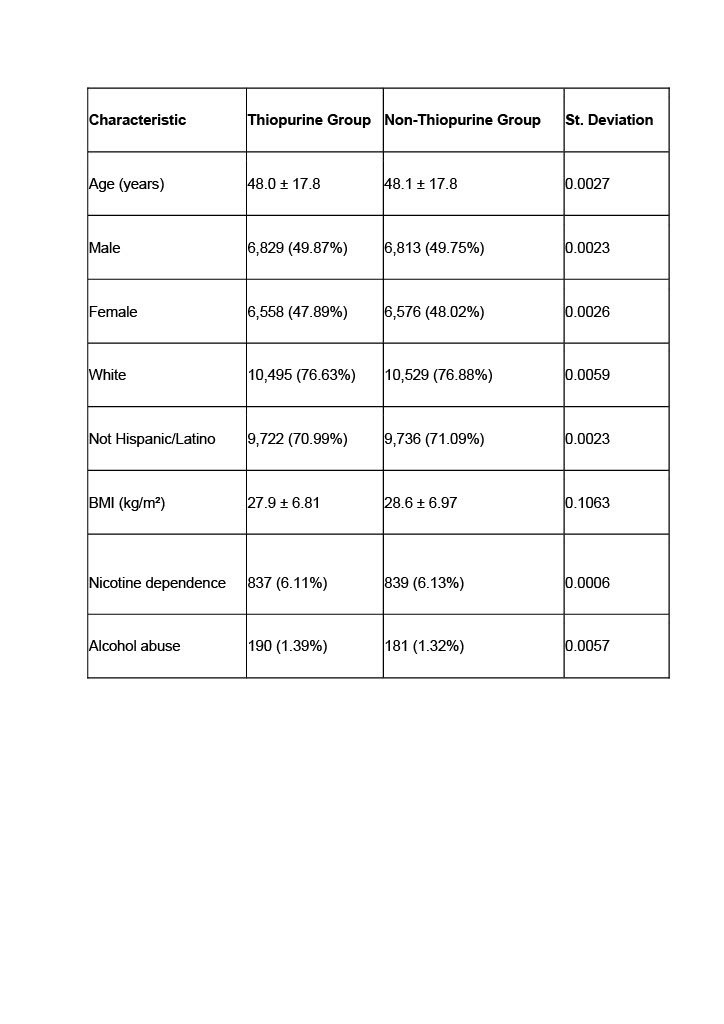
Figure: Patient Demographics and Characteristics stratified by thiopurine use
Disclosures:
Shivam Kalra indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Manjeet Kumar Goyal indicated no relevant financial relationships.
Maitri Shah indicated no relevant financial relationships.
Ashujot Dang indicated no relevant financial relationships.
Anmol Singh indicated no relevant financial relationships.
Kirti Arora indicated no relevant financial relationships.
Amaninder Dhaliwal indicated no relevant financial relationships.
Shivam Kalra, MBBS, MHA1, Rishi Chowdhary, MD2, Manjeet Kumar Goyal, MBBS, MD, DM, DNB3, Maitri Shah, MD4, Ashujot K. Dang, MD5, Anmol Singh, MD6, Kirti Arora, MD3, Amaninder Dhaliwal, MD7. P1159 - Predictors of Risk of Lymphoma in IBD Patients With Thiopurine Use: A Retrospective TrinetX Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
