Sunday Poster Session
Category: IBD
P1152 - Virtual Multidisciplinary Clinic Improves IBD Patient Engagement, Satisfaction, and Symptoms at Reduced Costs and Healthcare Utilization: A Propensity-Matched Prospective Observational Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SB
Sameer Berry, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Award: ACG Presidential Poster Award
Sameer Berry, MD1, Sanskriti Varma, MD2, Chamara Basnayake, MBBS3, Jeffrey Berinstein, MD, MS4, David Cook, MD, MHA5, Walter Chan, MD, MPH, FACG6, John Allen, MD, MBA4, Gil Y. Melmed, MD, MS, FACG7
1NYU Langone Health, New York, NY; 2Massachusetts General Hospital, Somerville, MA; 3St Vincent’s Hospital Melbourne – Department of Gastroenterology, Melbourne, Victoria, Australia; 4University of Michigan Health, Ann Arbor, MI; 5Optum Labs, Eden Prairie, MN; 6Brigham and Women's Hospital, Boston, MA; 7F. Widjaja Inflammatory Bowel Disease Institute, Cedars Sinai Medical Center, Los Angeles, CA
Introduction: Inflammatory bowel disease (IBD) is rising worldwide, yet care remains fragmented, delaying effective therapy. Virtual and multidisciplinary care models can each individually improve IBD outcomes, but no study has tested a fully virtual multidisciplinary clinic designed for IBD. We evaluated whether a virtual multidisciplinary gastrointestinal (GI) clinic improves patient-reported outcomes and lowers healthcare use and costs in IBD patients.
Methods: This prospective observational study included adults with IBD and commercial insurance who enrolled in a virtual multidisciplinary GI clinic between 3/2021–5/2025. Patients receiving ≥1 year of care were analyzed for clinical engagement. Those completing ≥4 visits provided baseline and post-care (after the most recent visit) self-reports on symptom severity, global symptom control, and satisfaction. McNemar’s Chi-square tests assessed paired pre-post outcomes. Claims data from 9- and 12-month periods were compared to propensity-matched controls using difference-in-difference (DiD) analysis, adjusting for baseline clinical and cost factors.
Results: We included 120 patients (58% female, mean age 39.7±11.8) and 202 matched controls. New GI diagnoses were made in 30%. Enrolled patients had a mean of 11 visits (range 2–42) and exchanged 164 messages (range 0–755). Most received care from dietitians (86%) and GI psychologists (68%). Symptom severity (n=106; 20% moderate-to-severe post-care vs 59% baseline; p< 0.0001), global symptom control (n=117; 90% vs 44%; p< 0.0001) and satisfaction with care (n=61; 98% vs 36%; p< 0.0001) were significantly improved. Compared to controls, there were numerical reductions in GI surgery (76%; p=0.16), GI-ED visits (76%; p=0.56), GI-inpatient stays (48%; p=0.52), and GI-imaging (15%; p=0.74) at 9 months. 9-month all-cause costs ($40,261 vs $54,672; DiD $15,731; p=0.16) and prescription costs ($37,824 vs $50,902; DiD $9,774; p=0.37) were numerically lower. Twelve-month savings persisted (all-cause: $50,576 vs $67,147; DiD $16,751; p=0.21; prescription costs: $35,683 vs $48,002; DiD $12,426; p=0.35).
Discussion: A virtual multidisciplinary IBD clinic achieved high clinical engagement and improved symptoms and satisfaction. While differences in utilization and costs were not statistically significant, the observed trends were robust and showed consistently lower costs among cases compared to controls. Virtual multidisciplinary care is a scalable, effective strategy for modern IBD management.
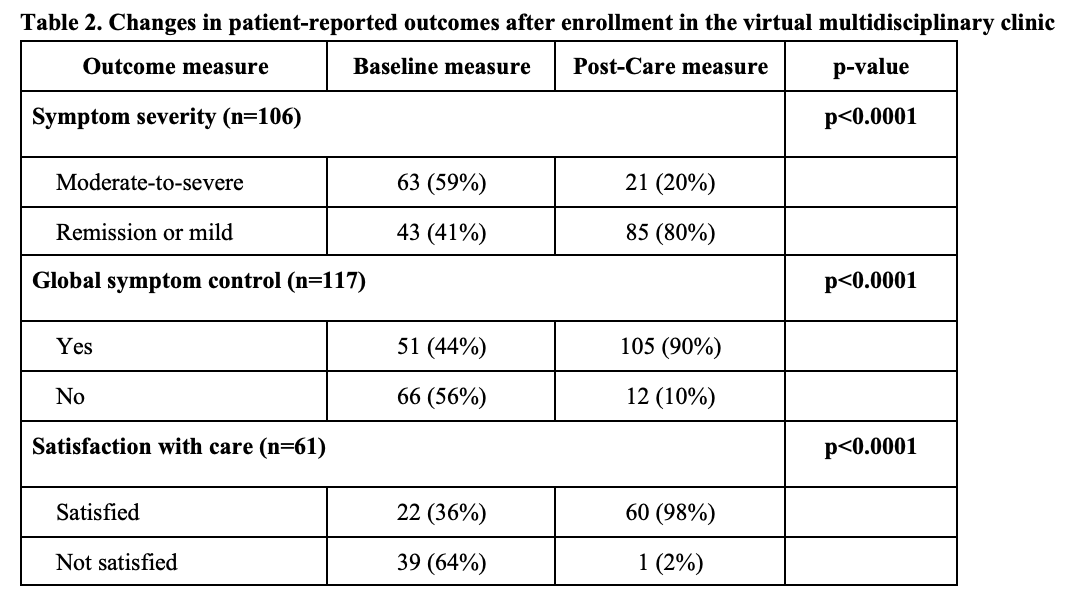
Figure: Values shown as N (%) or mean (standard deviation) for patients with documented diagnoses. Patients can have more than one condition and be classified multiple times. Diagnosis data is reflective of members who remained engaged in the clinic for at least 1 year.
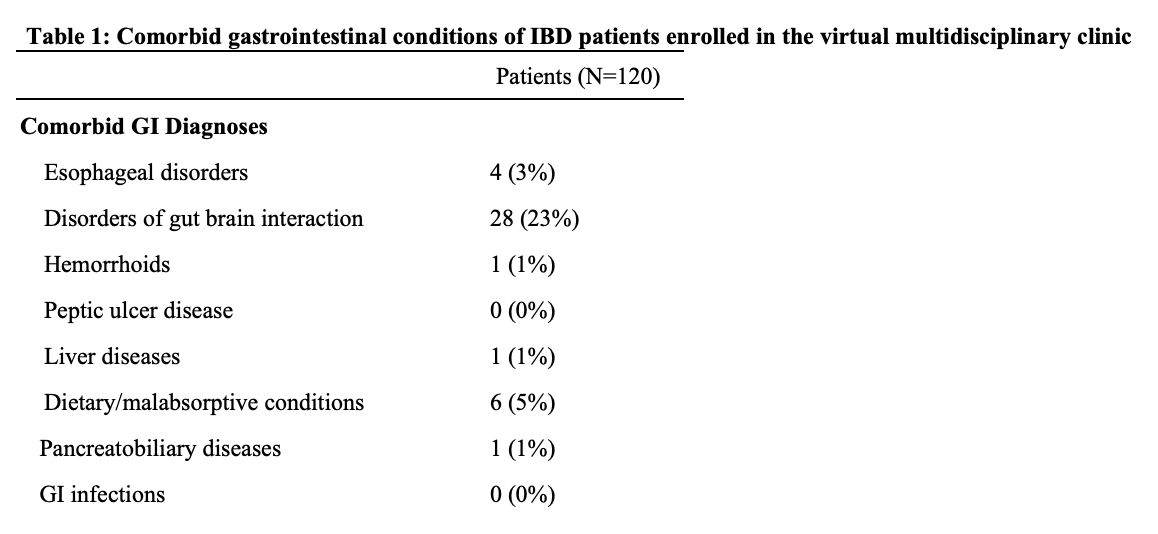
Figure: Symptom severity was assessed using the validated Patient-Modified Simple Clinical Colitis Activity Index (P-SCCAI) and Harvey Bradshaw Index (HBI). For the purposes of analyses, responses were grouped into “moderate-to-severe” for a score of 6+ on P-SCCAI and 8+ on HBI.
Global symptom control was assessed using a non-validated clinical questionnaire developed by Oshi Health for internal clinical use and measured in the following categories: yes, no.
Satisfaction with care was measured using the validated Customer Satisfaction Survey in the following categories: very dissatisfied, dissatisfied, neutral, satisfied, very satisfied. For the purposes of analyses, responses were grouped into “satisfied” if patients reported “satisfied” or “very satisfied” and “not satisfied” if patients reported “neutral”, “dissatisfied”, or “very dissatisfied”.
Disclosures:
Sameer Berry: Oshi Health – Employee.
Sanskriti Varma: Oshi Health – Consultant.
Chamara Basnayake indicated no relevant financial relationships.
Jeffrey Berinstein indicated no relevant financial relationships.
David Cook indicated no relevant financial relationships.
Walter Chan indicated no relevant financial relationships.
John Allen indicated no relevant financial relationships.
Gil Y. Melmed: AbbVie – Consultant. Arena – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Dieta – Consultant, Stock-privately held company. Ferring – Consultant. Fresenius Kalbi – Consultant. Genentech – Consultant. Gilead – Consultant. Iterative Scopes – Consultant. Janssen – Consultant. Lilly – Consultant. OptionCare – Personal Fees. Oshi Health – Consultant. Pfizer – Consultant, Grant/Research Support. Prometheus Labs – Consultant. Samsung Bioepis – Consultant. Takeda – Consultant. Techlab – Consultant. Treating inflammatory bowel disease using ultraviolet light – Intellectual Property/Patents. Treating inflammatory bowel disease with antifungal therapy – Intellectual Property/Patents. Verantos – Personal Fees. Viatris – Consultant.
Sameer Berry, MD1, Sanskriti Varma, MD2, Chamara Basnayake, MBBS3, Jeffrey Berinstein, MD, MS4, David Cook, MD, MHA5, Walter Chan, MD, MPH, FACG6, John Allen, MD, MBA4, Gil Y. Melmed, MD, MS, FACG7. P1152 - Virtual Multidisciplinary Clinic Improves IBD Patient Engagement, Satisfaction, and Symptoms at Reduced Costs and Healthcare Utilization: A Propensity-Matched Prospective Observational Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Sameer Berry, MD1, Sanskriti Varma, MD2, Chamara Basnayake, MBBS3, Jeffrey Berinstein, MD, MS4, David Cook, MD, MHA5, Walter Chan, MD, MPH, FACG6, John Allen, MD, MBA4, Gil Y. Melmed, MD, MS, FACG7
1NYU Langone Health, New York, NY; 2Massachusetts General Hospital, Somerville, MA; 3St Vincent’s Hospital Melbourne – Department of Gastroenterology, Melbourne, Victoria, Australia; 4University of Michigan Health, Ann Arbor, MI; 5Optum Labs, Eden Prairie, MN; 6Brigham and Women's Hospital, Boston, MA; 7F. Widjaja Inflammatory Bowel Disease Institute, Cedars Sinai Medical Center, Los Angeles, CA
Introduction: Inflammatory bowel disease (IBD) is rising worldwide, yet care remains fragmented, delaying effective therapy. Virtual and multidisciplinary care models can each individually improve IBD outcomes, but no study has tested a fully virtual multidisciplinary clinic designed for IBD. We evaluated whether a virtual multidisciplinary gastrointestinal (GI) clinic improves patient-reported outcomes and lowers healthcare use and costs in IBD patients.
Methods: This prospective observational study included adults with IBD and commercial insurance who enrolled in a virtual multidisciplinary GI clinic between 3/2021–5/2025. Patients receiving ≥1 year of care were analyzed for clinical engagement. Those completing ≥4 visits provided baseline and post-care (after the most recent visit) self-reports on symptom severity, global symptom control, and satisfaction. McNemar’s Chi-square tests assessed paired pre-post outcomes. Claims data from 9- and 12-month periods were compared to propensity-matched controls using difference-in-difference (DiD) analysis, adjusting for baseline clinical and cost factors.
Results: We included 120 patients (58% female, mean age 39.7±11.8) and 202 matched controls. New GI diagnoses were made in 30%. Enrolled patients had a mean of 11 visits (range 2–42) and exchanged 164 messages (range 0–755). Most received care from dietitians (86%) and GI psychologists (68%). Symptom severity (n=106; 20% moderate-to-severe post-care vs 59% baseline; p< 0.0001), global symptom control (n=117; 90% vs 44%; p< 0.0001) and satisfaction with care (n=61; 98% vs 36%; p< 0.0001) were significantly improved. Compared to controls, there were numerical reductions in GI surgery (76%; p=0.16), GI-ED visits (76%; p=0.56), GI-inpatient stays (48%; p=0.52), and GI-imaging (15%; p=0.74) at 9 months. 9-month all-cause costs ($40,261 vs $54,672; DiD $15,731; p=0.16) and prescription costs ($37,824 vs $50,902; DiD $9,774; p=0.37) were numerically lower. Twelve-month savings persisted (all-cause: $50,576 vs $67,147; DiD $16,751; p=0.21; prescription costs: $35,683 vs $48,002; DiD $12,426; p=0.35).
Discussion: A virtual multidisciplinary IBD clinic achieved high clinical engagement and improved symptoms and satisfaction. While differences in utilization and costs were not statistically significant, the observed trends were robust and showed consistently lower costs among cases compared to controls. Virtual multidisciplinary care is a scalable, effective strategy for modern IBD management.
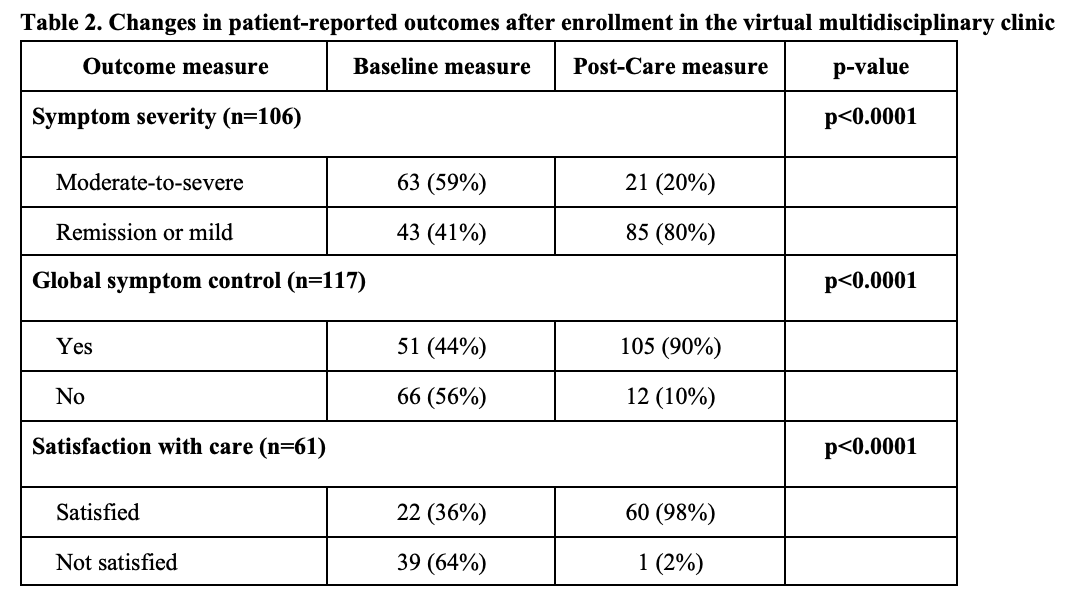
Figure: Values shown as N (%) or mean (standard deviation) for patients with documented diagnoses. Patients can have more than one condition and be classified multiple times. Diagnosis data is reflective of members who remained engaged in the clinic for at least 1 year.
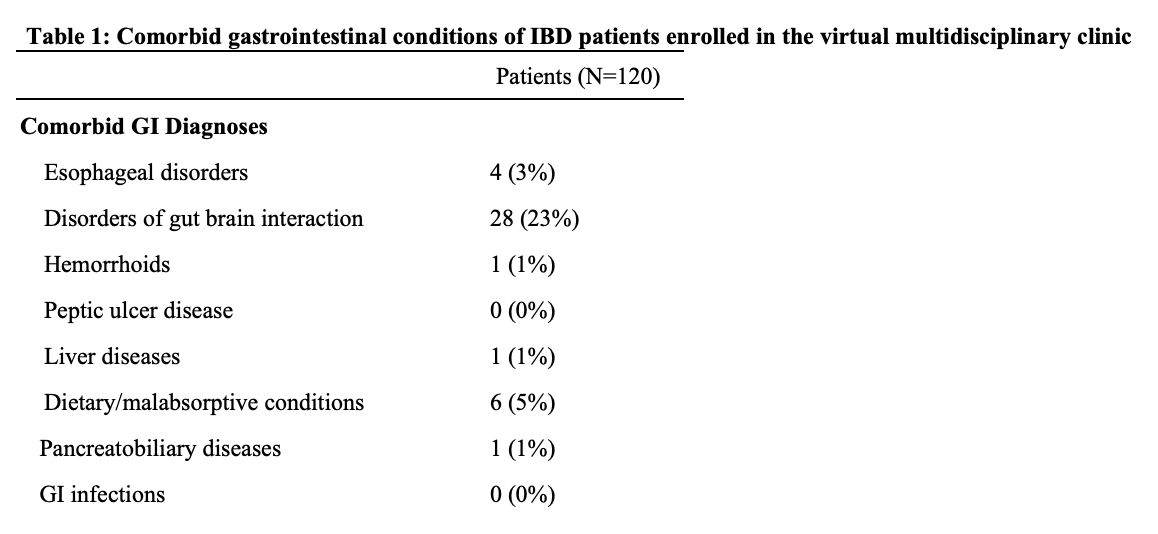
Figure: Symptom severity was assessed using the validated Patient-Modified Simple Clinical Colitis Activity Index (P-SCCAI) and Harvey Bradshaw Index (HBI). For the purposes of analyses, responses were grouped into “moderate-to-severe” for a score of 6+ on P-SCCAI and 8+ on HBI.
Global symptom control was assessed using a non-validated clinical questionnaire developed by Oshi Health for internal clinical use and measured in the following categories: yes, no.
Satisfaction with care was measured using the validated Customer Satisfaction Survey in the following categories: very dissatisfied, dissatisfied, neutral, satisfied, very satisfied. For the purposes of analyses, responses were grouped into “satisfied” if patients reported “satisfied” or “very satisfied” and “not satisfied” if patients reported “neutral”, “dissatisfied”, or “very dissatisfied”.
Disclosures:
Sameer Berry: Oshi Health – Employee.
Sanskriti Varma: Oshi Health – Consultant.
Chamara Basnayake indicated no relevant financial relationships.
Jeffrey Berinstein indicated no relevant financial relationships.
David Cook indicated no relevant financial relationships.
Walter Chan indicated no relevant financial relationships.
John Allen indicated no relevant financial relationships.
Gil Y. Melmed: AbbVie – Consultant. Arena – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Dieta – Consultant, Stock-privately held company. Ferring – Consultant. Fresenius Kalbi – Consultant. Genentech – Consultant. Gilead – Consultant. Iterative Scopes – Consultant. Janssen – Consultant. Lilly – Consultant. OptionCare – Personal Fees. Oshi Health – Consultant. Pfizer – Consultant, Grant/Research Support. Prometheus Labs – Consultant. Samsung Bioepis – Consultant. Takeda – Consultant. Techlab – Consultant. Treating inflammatory bowel disease using ultraviolet light – Intellectual Property/Patents. Treating inflammatory bowel disease with antifungal therapy – Intellectual Property/Patents. Verantos – Personal Fees. Viatris – Consultant.
Sameer Berry, MD1, Sanskriti Varma, MD2, Chamara Basnayake, MBBS3, Jeffrey Berinstein, MD, MS4, David Cook, MD, MHA5, Walter Chan, MD, MPH, FACG6, John Allen, MD, MBA4, Gil Y. Melmed, MD, MS, FACG7. P1152 - Virtual Multidisciplinary Clinic Improves IBD Patient Engagement, Satisfaction, and Symptoms at Reduced Costs and Healthcare Utilization: A Propensity-Matched Prospective Observational Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

