Sunday Poster Session
Category: IBD
P1146 - Evaluation of the Relationship Between Endoscopic Disease Severity and Treatment Choice for Patients With Ulcerative Colitis Using a Real-World Data Set Linked to Endoscopic Videos Evaluated With Computer Vision
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- PD
Parambir Dulai, MD
Division of Gastroenterology and Hepatology, Feinberg School of Medicine, Northwestern University
Chicago, IL
Presenting Author(s)
Parambir S. Dulai, MD1, Ronen Arai, MD2, Shrujal Baxi, MD, MPH3, Darren Thomason, MBA4, Yeli Wang, PhD3, Maggie McCue, MS, RD5, Chris Blair, MS5, Lisa Young, PhD5, Megan Gower, PharmD5, Vijay Vajnik, MD, PhD5
1Division of Gastroenterology and Hepatology, Feinberg School of Medicine, Northwestern University, Chicago, IL; 2Gastro Health, Coral Springs, FL; 3Iterative Health, Cambridge, MA; 4Iterative Health Inc, Cambridge, MA; 5Takeda Pharmaceuticals U.S.A. Inc., Cambridge, MA
Introduction: Standardized diagnostic tools to assess endoscopic disease severity in patients with ulcerative colitis (UC) are needed but clinical practices may lack appropriate resources for routine deployment. Artificial intelligence (AI) models can enable rapid, standardized assessments of endoscopy videos. This retrospective, observational study assessed whether AI-driven endoscopy findings were associated with treatment plan in patients with UC in community gastroenterology clinics in the USA.
Methods: Adults with UC who underwent endoscopy using Iterative Health video recording technology between January 1, 2023 and June 30, 2024 in the Gastro Health network were included. Baseline characteristics and treatment data were collected from electronic health records for 6 months before and 6 months after the date of endoscopy (index date), respectively. Endoscopy videos were analyzed with computer vision AI to generate an AI Endoscopic Score (AI-ES; Mayo endoscopic score model of disease severity [0 = inactive, 1 = mild, 2 = moderate, and 3 = severe]) and AI Endoscopic Score for disease extent (AI-ESe; high is defined as ≥ 20% of clips showing moderate or severe inflammation). The relationships between AI-ES or AI-ESe and treatment selection were analyzed by logistic regression to calculate odds ratios (ORs) with 95% confidence intervals (CIs), using patients with an AI-ES of 0–1 or a low AI-ESe as a reference.
Results: Of 799 patients, 141 (17.6%) had an AI-ES of 2–3 (moderate to severe endoscopic activity) and 158 (19.8%) had extensive disease (high AI-ESe; Figure 1). After endoscopy, 28.4% of patients with an AI-ES of 2–3 received advanced therapy. On univariable analysis, patients with an AI-ES of 2–3 had higher odds of receiving advanced therapy vs no advanced therapy (OR, 1.78; 95% CI, 1.16–2.68) and higher odds of receiving any therapy vs no therapy (OR, 1.70; 95% CI, 1.17–2.46; Figure 2). Patients with a high AI-ESe had higher odds of receiving advanced therapy vs no advanced therapy (OR, 1.82; 95% CI, 1.21–2.71) and higher odds of receiving any therapy vs no therapy (OR, 1.99; 95% CI, 1.39–2.83; Figure 2). Multivariable analysis results were similar.
Discussion: AI-based endoscopic scores correlated with treatment plan for patients with UC. However, disease severity alone may not drive treatment selection and patients with moderate to severe disease may be undertreated in routine care. AI may support standardized treatment decisions and care continuity across providers and experience levels.
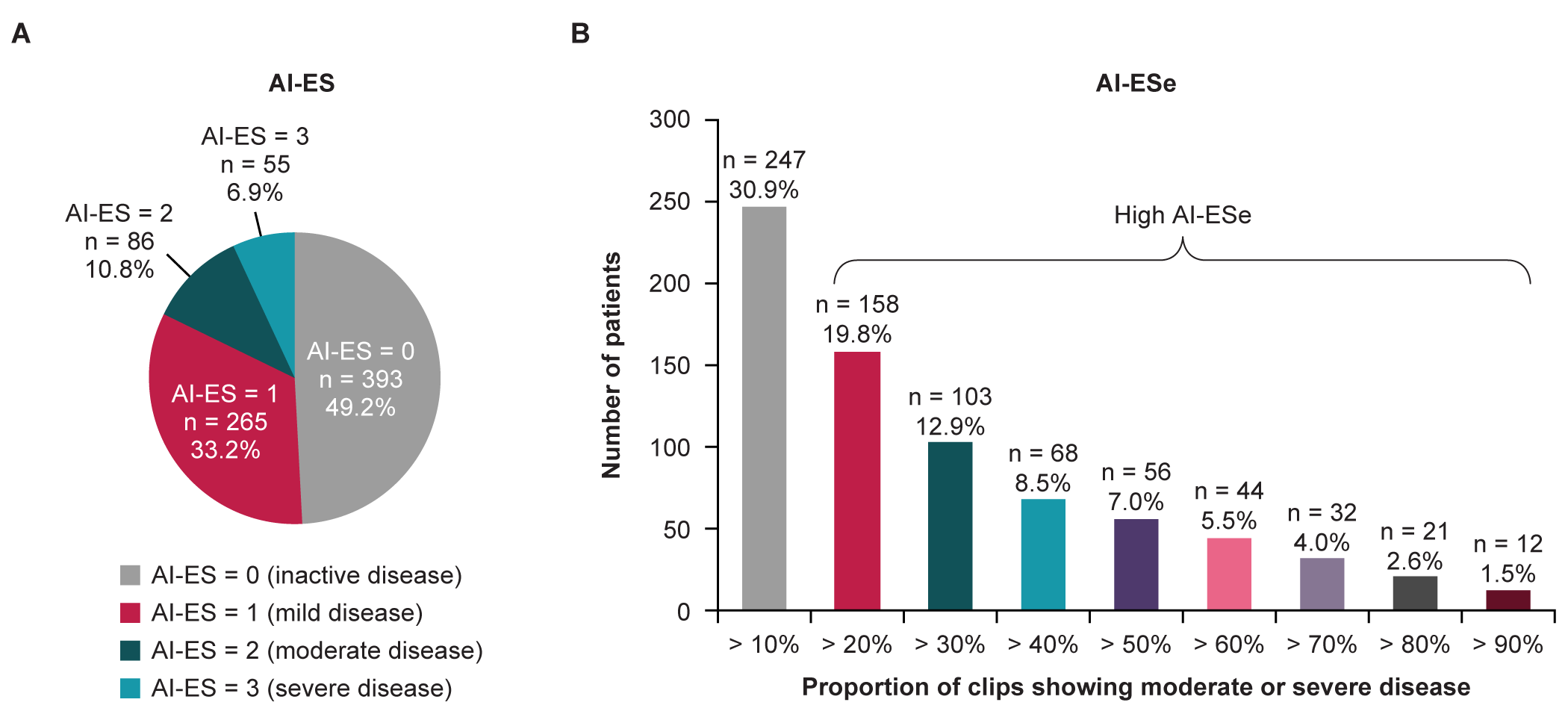
Figure: Figure 1. AI-ES and AI-ESe assessed using the Iterative Health endoscopic video recording technology and computer vision.
For AI-ESe, patients could be in more than one threshold category. AI-ES, Artificial Intelligence Endoscopic Score; AI-ESe, Artificial Intelligence Endoscopic Score for disease extent.
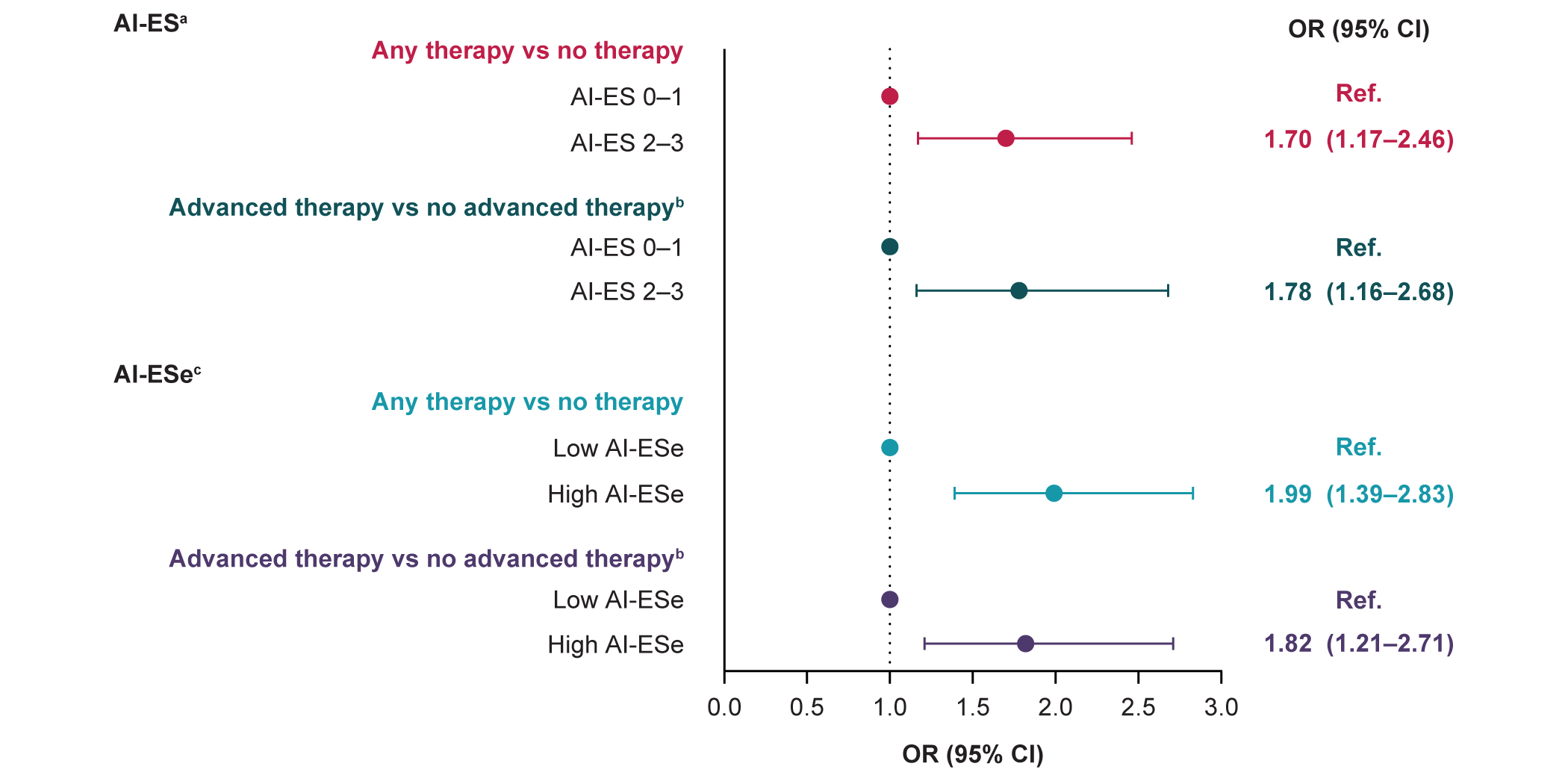
Figure: Figure 2. Univariable logistic regression to assess the relationship between AI-ES or AI-ESe and treatment selection after endoscopy.
aMayo endoscopic score model of disease severity where 0 = inactive, 1 = mild, 2 = moderate, and 3 = severe. bConventional therapy or no therapy. cDisease severity index where high is defined as ≥ 20% of clips showing mucosal surface with moderate or severe inflammation. AI-ES, Artificial Intelligence Endoscopic Score; AI-ESe, Artificial Intelligence Endoscopic Score for disease extent; CI, confidence interval; OR, odds ratio; Ref., reference.
Disclosures:
Parambir S. Dulai: AbbVie – Consultant. Abivax – Consultant. Adiso – Consultant. Alimentiv – Consultant. Bristol Myers Squibb – Consultant. Celltrion – Consultant. Digbi Health – Stock Options. Genentech – Consultant. Geneoscopy – Consultant. GSK – Consultant. Janssen – Consultant. Lilly – Consultant. Pfizer – Consultant, Grant/Research Support. Precidiag – Royalties. Takeda – Consultant, Grant/Research Support.
Ronen Arai: AbbVie – Speakers Bureau. Bristol Myers Squibb – Speakers Bureau. Castle Biosciences – Speakers Bureau. Celltrion – Speakers Bureau. Janssen – Speakers Bureau. Lilly – Speakers Bureau. Pfizer – Speakers Bureau. Phathom Pharmaceuticals – Speakers Bureau. Prometheus Pharmaceuticals – Consultant. Takeda – Speakers Bureau.
Shrujal Baxi: Iterative Health – Employee.
Darren Thomason: Iterative Health – Employee.
Yeli Wang: Iterative Health – Employee.
Maggie McCue: Takeda – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Chris Blair: Takeda – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Lisa Young: Takeda – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Megan Gower: Takeda – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Vijay Vajnik: Takeda – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Parambir S. Dulai, MD1, Ronen Arai, MD2, Shrujal Baxi, MD, MPH3, Darren Thomason, MBA4, Yeli Wang, PhD3, Maggie McCue, MS, RD5, Chris Blair, MS5, Lisa Young, PhD5, Megan Gower, PharmD5, Vijay Vajnik, MD, PhD5. P1146 - Evaluation of the Relationship Between Endoscopic Disease Severity and Treatment Choice for Patients With Ulcerative Colitis Using a Real-World Data Set Linked to Endoscopic Videos Evaluated With Computer Vision, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Division of Gastroenterology and Hepatology, Feinberg School of Medicine, Northwestern University, Chicago, IL; 2Gastro Health, Coral Springs, FL; 3Iterative Health, Cambridge, MA; 4Iterative Health Inc, Cambridge, MA; 5Takeda Pharmaceuticals U.S.A. Inc., Cambridge, MA
Introduction: Standardized diagnostic tools to assess endoscopic disease severity in patients with ulcerative colitis (UC) are needed but clinical practices may lack appropriate resources for routine deployment. Artificial intelligence (AI) models can enable rapid, standardized assessments of endoscopy videos. This retrospective, observational study assessed whether AI-driven endoscopy findings were associated with treatment plan in patients with UC in community gastroenterology clinics in the USA.
Methods: Adults with UC who underwent endoscopy using Iterative Health video recording technology between January 1, 2023 and June 30, 2024 in the Gastro Health network were included. Baseline characteristics and treatment data were collected from electronic health records for 6 months before and 6 months after the date of endoscopy (index date), respectively. Endoscopy videos were analyzed with computer vision AI to generate an AI Endoscopic Score (AI-ES; Mayo endoscopic score model of disease severity [0 = inactive, 1 = mild, 2 = moderate, and 3 = severe]) and AI Endoscopic Score for disease extent (AI-ESe; high is defined as ≥ 20% of clips showing moderate or severe inflammation). The relationships between AI-ES or AI-ESe and treatment selection were analyzed by logistic regression to calculate odds ratios (ORs) with 95% confidence intervals (CIs), using patients with an AI-ES of 0–1 or a low AI-ESe as a reference.
Results: Of 799 patients, 141 (17.6%) had an AI-ES of 2–3 (moderate to severe endoscopic activity) and 158 (19.8%) had extensive disease (high AI-ESe; Figure 1). After endoscopy, 28.4% of patients with an AI-ES of 2–3 received advanced therapy. On univariable analysis, patients with an AI-ES of 2–3 had higher odds of receiving advanced therapy vs no advanced therapy (OR, 1.78; 95% CI, 1.16–2.68) and higher odds of receiving any therapy vs no therapy (OR, 1.70; 95% CI, 1.17–2.46; Figure 2). Patients with a high AI-ESe had higher odds of receiving advanced therapy vs no advanced therapy (OR, 1.82; 95% CI, 1.21–2.71) and higher odds of receiving any therapy vs no therapy (OR, 1.99; 95% CI, 1.39–2.83; Figure 2). Multivariable analysis results were similar.
Discussion: AI-based endoscopic scores correlated with treatment plan for patients with UC. However, disease severity alone may not drive treatment selection and patients with moderate to severe disease may be undertreated in routine care. AI may support standardized treatment decisions and care continuity across providers and experience levels.
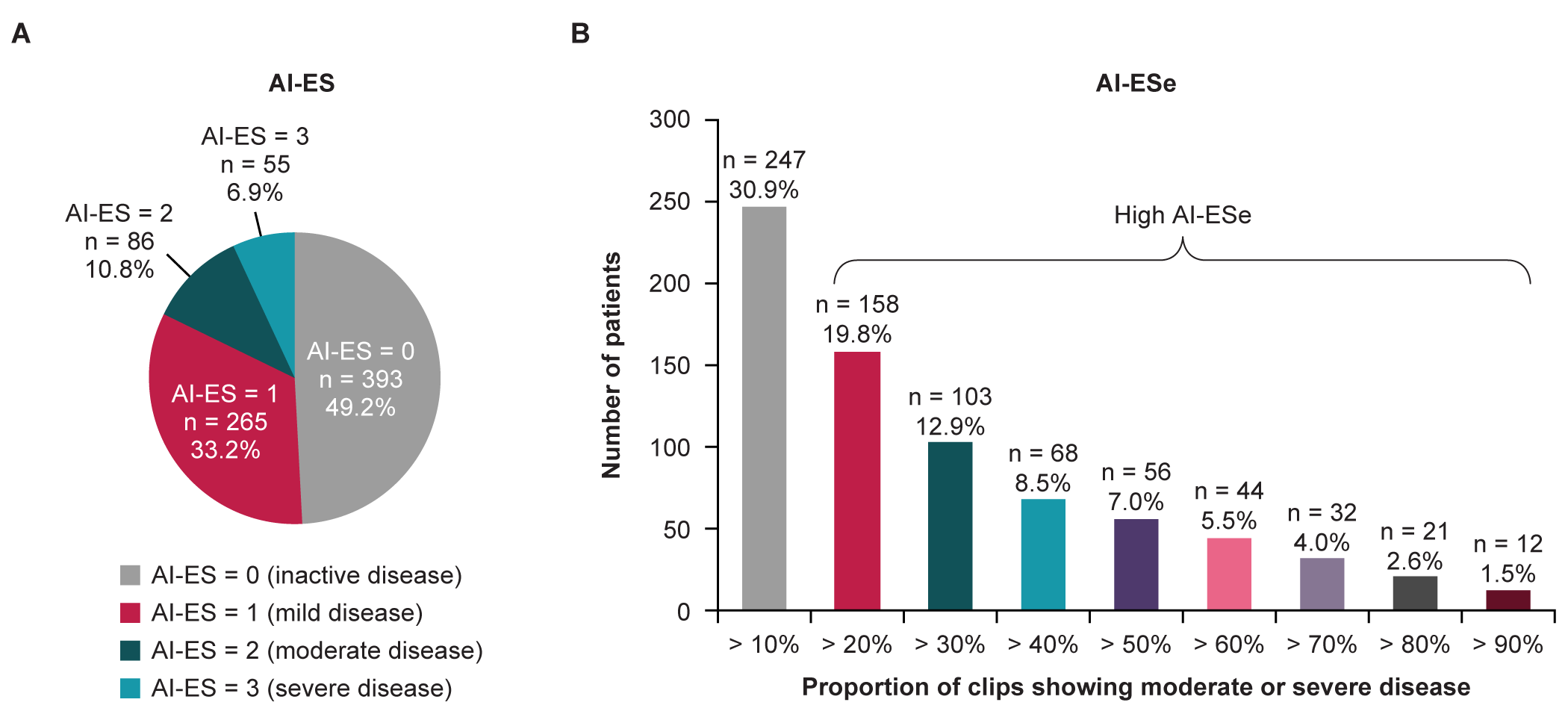
Figure: Figure 1. AI-ES and AI-ESe assessed using the Iterative Health endoscopic video recording technology and computer vision.
For AI-ESe, patients could be in more than one threshold category. AI-ES, Artificial Intelligence Endoscopic Score; AI-ESe, Artificial Intelligence Endoscopic Score for disease extent.
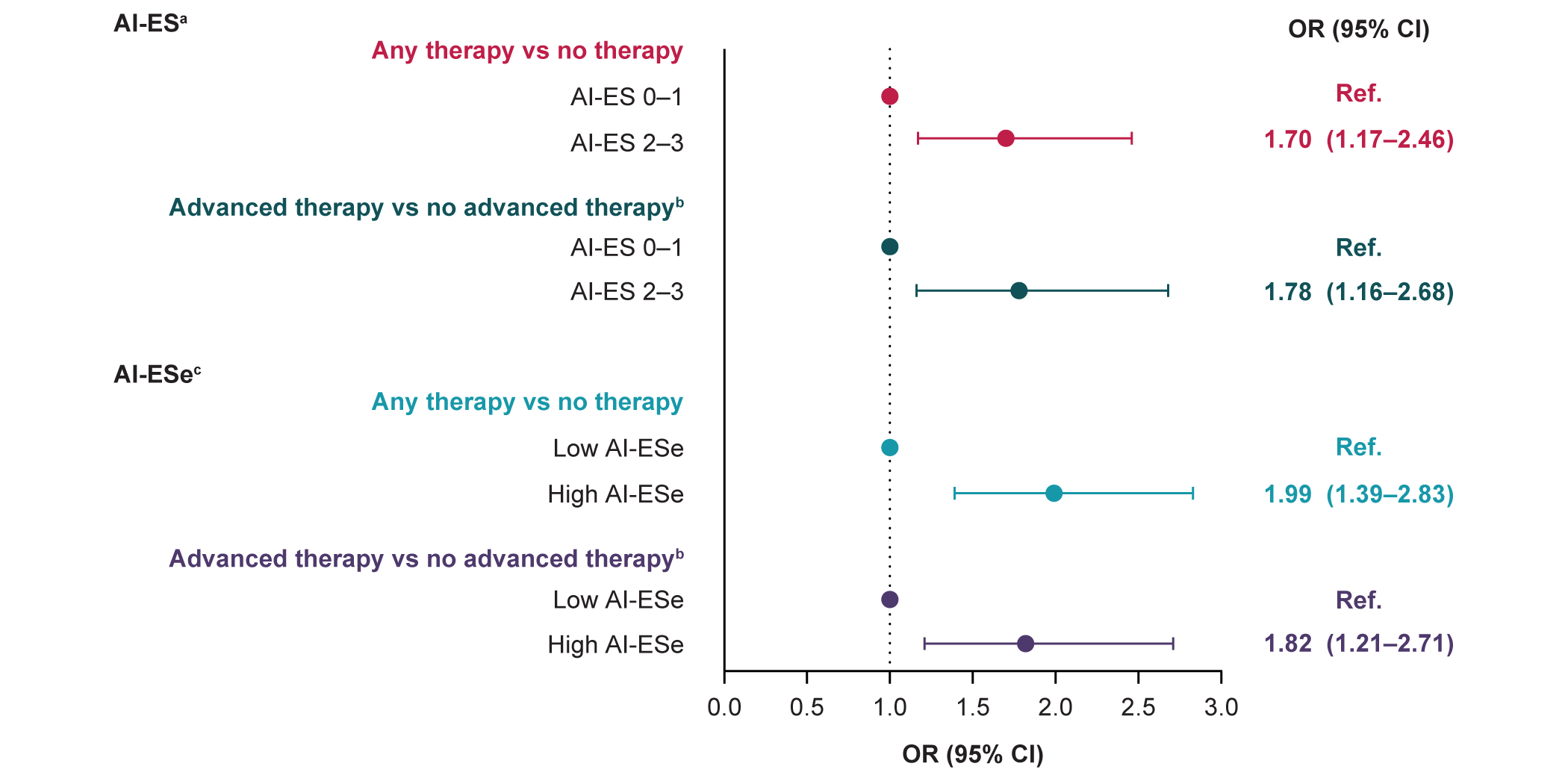
Figure: Figure 2. Univariable logistic regression to assess the relationship between AI-ES or AI-ESe and treatment selection after endoscopy.
aMayo endoscopic score model of disease severity where 0 = inactive, 1 = mild, 2 = moderate, and 3 = severe. bConventional therapy or no therapy. cDisease severity index where high is defined as ≥ 20% of clips showing mucosal surface with moderate or severe inflammation. AI-ES, Artificial Intelligence Endoscopic Score; AI-ESe, Artificial Intelligence Endoscopic Score for disease extent; CI, confidence interval; OR, odds ratio; Ref., reference.
Disclosures:
Parambir S. Dulai: AbbVie – Consultant. Abivax – Consultant. Adiso – Consultant. Alimentiv – Consultant. Bristol Myers Squibb – Consultant. Celltrion – Consultant. Digbi Health – Stock Options. Genentech – Consultant. Geneoscopy – Consultant. GSK – Consultant. Janssen – Consultant. Lilly – Consultant. Pfizer – Consultant, Grant/Research Support. Precidiag – Royalties. Takeda – Consultant, Grant/Research Support.
Ronen Arai: AbbVie – Speakers Bureau. Bristol Myers Squibb – Speakers Bureau. Castle Biosciences – Speakers Bureau. Celltrion – Speakers Bureau. Janssen – Speakers Bureau. Lilly – Speakers Bureau. Pfizer – Speakers Bureau. Phathom Pharmaceuticals – Speakers Bureau. Prometheus Pharmaceuticals – Consultant. Takeda – Speakers Bureau.
Shrujal Baxi: Iterative Health – Employee.
Darren Thomason: Iterative Health – Employee.
Yeli Wang: Iterative Health – Employee.
Maggie McCue: Takeda – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Chris Blair: Takeda – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Lisa Young: Takeda – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Megan Gower: Takeda – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Vijay Vajnik: Takeda – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Parambir S. Dulai, MD1, Ronen Arai, MD2, Shrujal Baxi, MD, MPH3, Darren Thomason, MBA4, Yeli Wang, PhD3, Maggie McCue, MS, RD5, Chris Blair, MS5, Lisa Young, PhD5, Megan Gower, PharmD5, Vijay Vajnik, MD, PhD5. P1146 - Evaluation of the Relationship Between Endoscopic Disease Severity and Treatment Choice for Patients With Ulcerative Colitis Using a Real-World Data Set Linked to Endoscopic Videos Evaluated With Computer Vision, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
