Sunday Poster Session
Category: IBD
P1142 - Evaluating the Risk of Inflammatory Bowel Disease Following Cholecystectomy: A Multicenter Propensity Score-Matched Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Nirav Agrawal, MD, MPH
Anne Arundel Medical Center, Luminus Health
Annapolis, MD
Presenting Author(s)
Aditya Chandrashekar, MBBS1, Nirav Agrawal, MD, MPH2, Arpita Jajoo, MD1, Jianing Li, MD1, Venkata Akshintala, MD, PhD1
1The Johns Hopkins Hospital, Baltimore, MD; 2Anne Arundel Medical Center, Luminus Health, Annapolis, MD
Introduction: Previous studies suggest that post-cholecystectomy (CCY) patients have increased secondary bile acids, along with a shift in gut microbiota that alters the populations of both beneficial and pathogenic bacteria. Patients with Inflammatory Bowel Disease (IBD) exhibit higher levels of primary bile acids and lower concentrations of beneficial secondary bile acids. Secondary bile acids have been shown to have anti-inflammatory effects in colitis models, indicating protective roles against mucosal inflammation. However, the connection between cholecystectomy and IBD risk is still debated. We aimed to quantify the risk of incident Ulcerative colitis (UC) and Crohn’s disease (CD) after CCY.
Methods: We queried the TriNetX database for adults (≥18 y) with cholelithiasis (2000‑2025). Patients were classified as post-CCY or nonoperative controls. Propensity‑score matching (1:1) balanced age, sex, ethnicity, and known IBD risk factors such as tobacco use, long-term antibiotics, and NSAID use, yielding two cohorts of 582,529 patients (Figure 1). Incident IBD was identified with ICD-10 codes ≥1 day after the index date. Risk ratios (RRs) and odds ratios (ORs) were calculated. Time-to-event was assessed using Kaplan–Meier curves and Cox models, which provided hazard ratios (HRs).
Results: During a median follow-up of 6.2 years, UC occurred in 0.39% of post CCY patients versus 0.47% of controls, resulting in a risk ratio of 0.826 (95% CI 0.782, 0.874; p < 0.001) and a hazard ratio of 0.808 (0.764, 0.854; p < 0.001). CD developed in 0.24 % post‑CCY vs. 0.29% of controls (RR 0.799 (0.744, 0.858), HR 0.781(0.728, 0.839); both p < 0.001). Risk reductions persisted across all UC and CD phenotypes, with no phenotype demonstrating an increased risk. Kaplan-Meier curves revealed higher IBD-free survival post-CCY (log-rank p < 0.001 for both UC and CD)(Figure 2).
Discussion: Cholecystectomy was associated with an increased IBD risk, with a 17–20 % relative risk reduction for both UC and CD, sustained across disease phenotypes. Prospective studies integrating bile acid profiling and microbiota sequencing are warranted to elucidate the underlying mechanisms, but the current literature suggests that anti-inflammatory alterations in secondary bile acids and the gut microbiota may play a role.
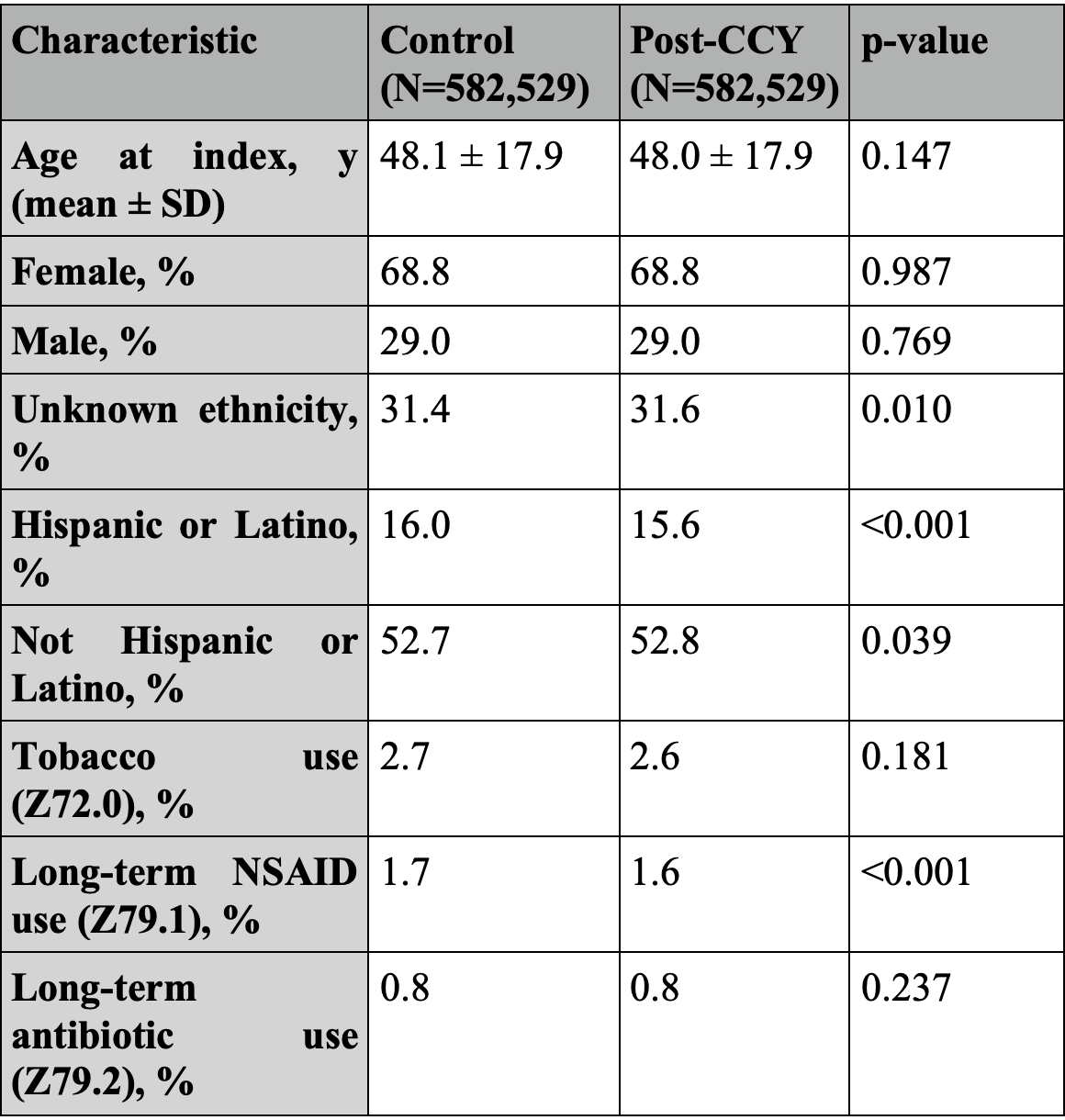
Figure: Figure 1: Baseline characteristics before and after propensity matching.
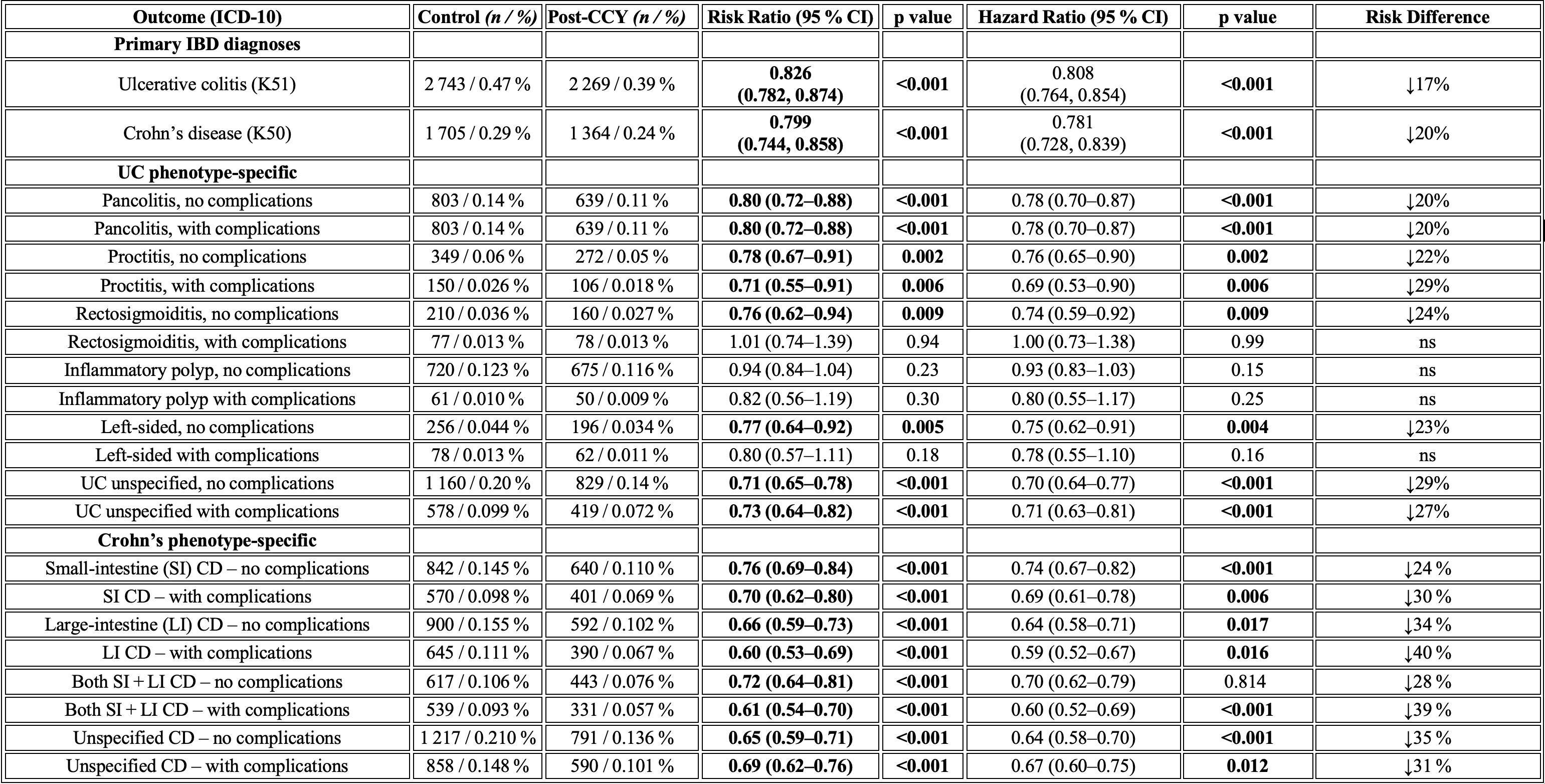
Figure: Figure 2: Risk of Developing Inflammatory Bowel Disease After Cholecystectomy: Incidence, Risk Ratios, and Hazard Ratios in Propensity-Score Matched Cohorts (Patients with outcomes before the index event were excluded).
Disclosures:
Aditya Chandrashekar indicated no relevant financial relationships.
Nirav Agrawal indicated no relevant financial relationships.
Arpita Jajoo indicated no relevant financial relationships.
Jianing Li indicated no relevant financial relationships.
Venkata Akshintala indicated no relevant financial relationships.
Aditya Chandrashekar, MBBS1, Nirav Agrawal, MD, MPH2, Arpita Jajoo, MD1, Jianing Li, MD1, Venkata Akshintala, MD, PhD1. P1142 - Evaluating the Risk of Inflammatory Bowel Disease Following Cholecystectomy: A Multicenter Propensity Score-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The Johns Hopkins Hospital, Baltimore, MD; 2Anne Arundel Medical Center, Luminus Health, Annapolis, MD
Introduction: Previous studies suggest that post-cholecystectomy (CCY) patients have increased secondary bile acids, along with a shift in gut microbiota that alters the populations of both beneficial and pathogenic bacteria. Patients with Inflammatory Bowel Disease (IBD) exhibit higher levels of primary bile acids and lower concentrations of beneficial secondary bile acids. Secondary bile acids have been shown to have anti-inflammatory effects in colitis models, indicating protective roles against mucosal inflammation. However, the connection between cholecystectomy and IBD risk is still debated. We aimed to quantify the risk of incident Ulcerative colitis (UC) and Crohn’s disease (CD) after CCY.
Methods: We queried the TriNetX database for adults (≥18 y) with cholelithiasis (2000‑2025). Patients were classified as post-CCY or nonoperative controls. Propensity‑score matching (1:1) balanced age, sex, ethnicity, and known IBD risk factors such as tobacco use, long-term antibiotics, and NSAID use, yielding two cohorts of 582,529 patients (Figure 1). Incident IBD was identified with ICD-10 codes ≥1 day after the index date. Risk ratios (RRs) and odds ratios (ORs) were calculated. Time-to-event was assessed using Kaplan–Meier curves and Cox models, which provided hazard ratios (HRs).
Results: During a median follow-up of 6.2 years, UC occurred in 0.39% of post CCY patients versus 0.47% of controls, resulting in a risk ratio of 0.826 (95% CI 0.782, 0.874; p < 0.001) and a hazard ratio of 0.808 (0.764, 0.854; p < 0.001). CD developed in 0.24 % post‑CCY vs. 0.29% of controls (RR 0.799 (0.744, 0.858), HR 0.781(0.728, 0.839); both p < 0.001). Risk reductions persisted across all UC and CD phenotypes, with no phenotype demonstrating an increased risk. Kaplan-Meier curves revealed higher IBD-free survival post-CCY (log-rank p < 0.001 for both UC and CD)(Figure 2).
Discussion: Cholecystectomy was associated with an increased IBD risk, with a 17–20 % relative risk reduction for both UC and CD, sustained across disease phenotypes. Prospective studies integrating bile acid profiling and microbiota sequencing are warranted to elucidate the underlying mechanisms, but the current literature suggests that anti-inflammatory alterations in secondary bile acids and the gut microbiota may play a role.
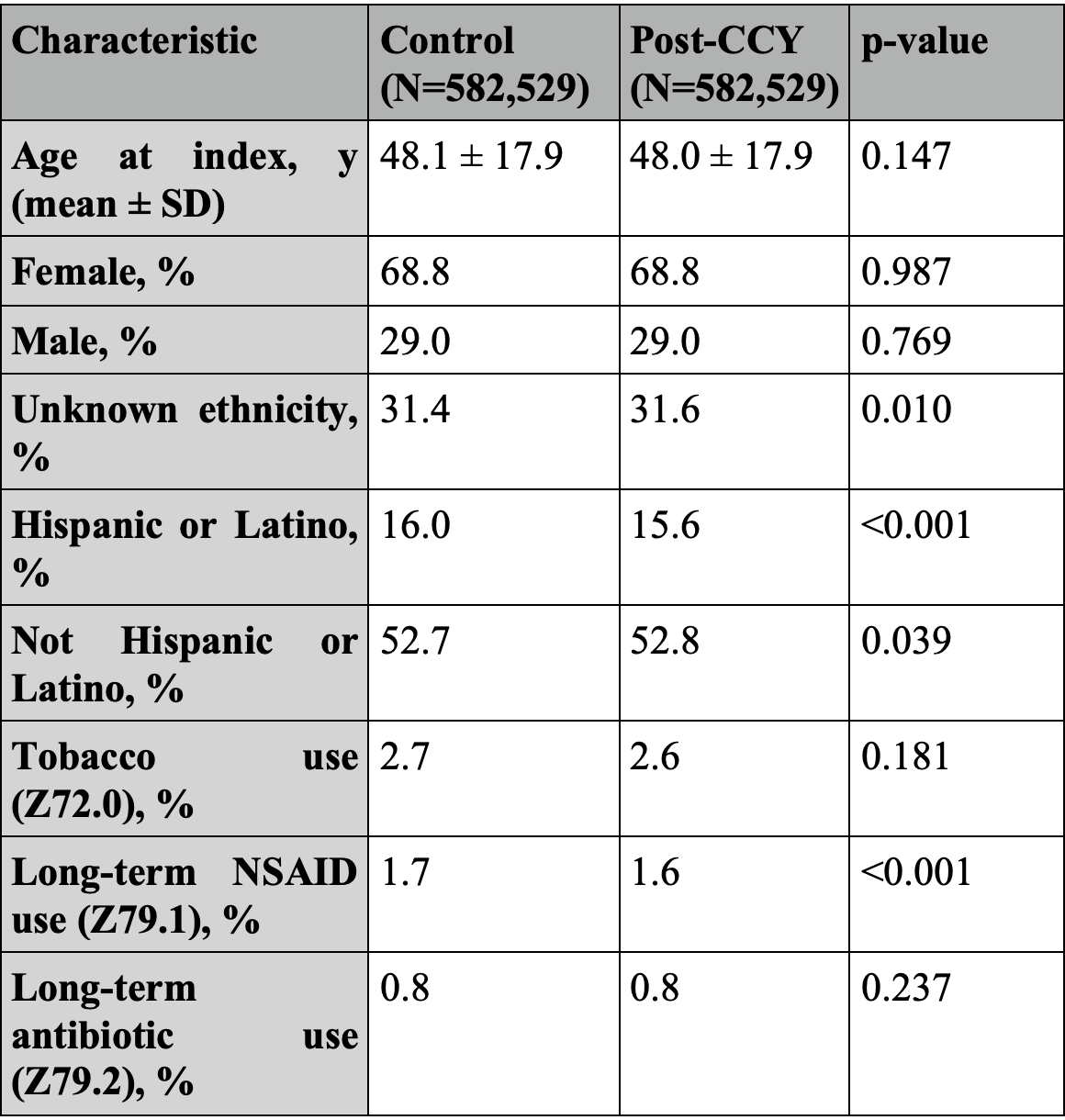
Figure: Figure 1: Baseline characteristics before and after propensity matching.
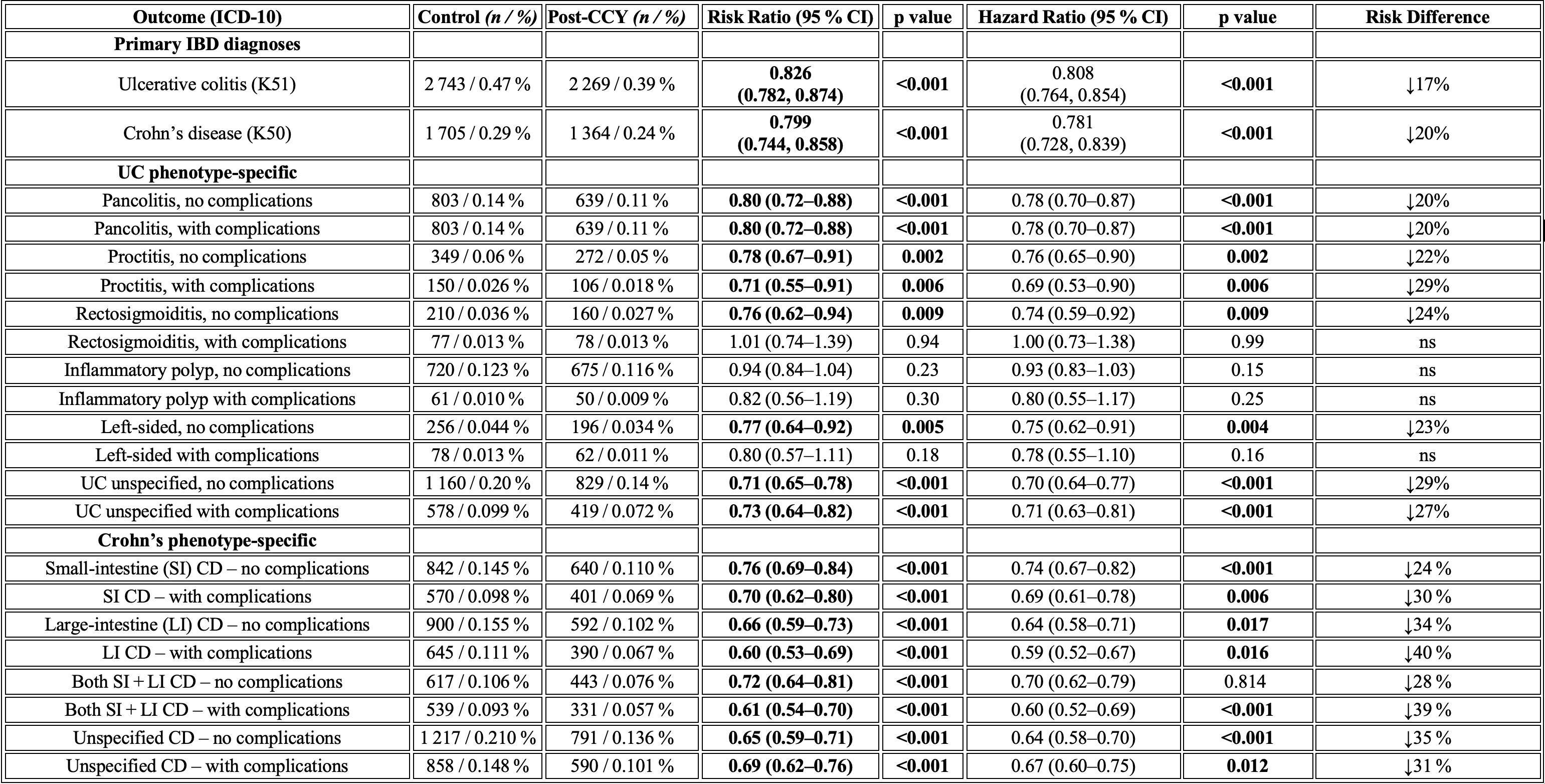
Figure: Figure 2: Risk of Developing Inflammatory Bowel Disease After Cholecystectomy: Incidence, Risk Ratios, and Hazard Ratios in Propensity-Score Matched Cohorts (Patients with outcomes before the index event were excluded).
Disclosures:
Aditya Chandrashekar indicated no relevant financial relationships.
Nirav Agrawal indicated no relevant financial relationships.
Arpita Jajoo indicated no relevant financial relationships.
Jianing Li indicated no relevant financial relationships.
Venkata Akshintala indicated no relevant financial relationships.
Aditya Chandrashekar, MBBS1, Nirav Agrawal, MD, MPH2, Arpita Jajoo, MD1, Jianing Li, MD1, Venkata Akshintala, MD, PhD1. P1142 - Evaluating the Risk of Inflammatory Bowel Disease Following Cholecystectomy: A Multicenter Propensity Score-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
