Sunday Poster Session
Category: IBD
P1130 - Impact of Delayed Diagnosis on Outcomes in Inflammatory Bowel Disease (IBD)
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Salman Almuammar, MBBS (he/him/his)
King Faisal Specialist Hospital and Research Centre
Riyadh, Ar Riyad, Saudi Arabia
Presenting Author(s)
Salman Almuammar, MBBS1, Badr Al Bawardy, MD2, Lina Alyahya, 3, Weam Mahmoud, 3, Abdulelah Almutairdi, MD1, Mashary Attamimi, MD1, Sameer Desai, 1
1King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia; 2Yale New Haven Hospital, New Haven, USA; King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia, New Haven, CT; 3Alfaisal University, Riyadh, Ar Riyad, Saudi Arabia
Introduction: Inflammatory Bowel Disease (IBD), encompassing Crohn’s disease (CD) and ulcerative colitis (UC), is a chronic inflammatory condition of the gastrointestinal tract. Delayed diagnosis is hypothesized to influence disease outcomes adversely, yet its impact remains underexplored, particularly in Saudi Arabia. This study investigates the association between diagnostic delay and clinical outcomes in IBD patients.
Methods: This cross-sectional study utilized data from a prospectively maintained IBD registry at King Faisal Specialist Hospital and Research Centre from September 2023 to September 2024. Inclusion criteria comprised patients aged ≥14 years with a confirmed diagnosis of IBD. Diagnostic delay, defined as the time from symptom onset to diagnosis, was categorized as < 1 year, 1–2 years, and >2 years. Clinical outcomes included the need for intestinal surgery, >2 advanced therapies, and a composite outcome (surgery, advanced therapies, or disease progression). Associations were assessed using Chi-squared and Fisher’s exact tests.
Results: The cohort included 412 patients (mean age at diagnosis: 24 years; 55% male; 68% CD, 32% UC). The average diagnostic delay was 1.48 years, with 26% experiencing delays >2 years. Patients with longer delays were more likely to have CD (p=0.049), older age at diagnosis (p=0.017), and stricturing disease phenotype in CD (p=0.013). Delayed diagnosis ( >2 years) was associated with a higher prevalence of intestinal surgery (32% vs. 23%; p=0.045) and borderline significance for the composite outcome (p=0.062). No significant associations were found between delay and use of >2 advanced therapies.
Discussion: Diagnostic delay in IBD is prevalent and associated with worse outcomes, particularly in patients with CD. Efforts to minimize diagnostic delays may improve clinical outcomes and reduce the need for surgical interventions. Further research with larger cohorts and longitudinal follow-up is warranted to elucidate these associations.
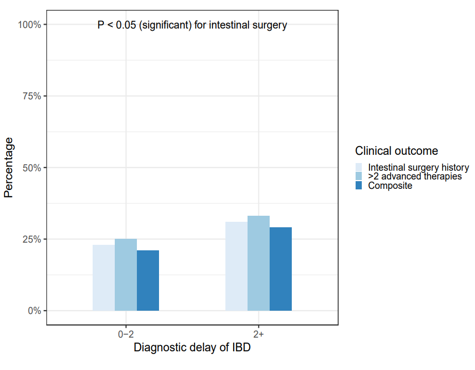
Figure: The effect of diagnostic delay in IBD
Disclosures:
Salman Almuammar indicated no relevant financial relationships.
Badr Al Bawardy: AbbVie – Advisor or Review Panel Member, Consultant, Speakers Bureau. Bristol Myers Squibb – Advisory Committee/Board Member, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Hikma – Speakers Bureau. Janssen – Advisory Committee/Board Member, Speakers Bureau. Pfizer – Advisory Committee/Board Member. TAKEDA – Advisor or Review Panel Member, Speakers Bureau.
Lina Alyahya indicated no relevant financial relationships.
Weam Mahmoud indicated no relevant financial relationships.
Abdulelah Almutairdi: AbbVie – Advisory Committee/Board Member, Speakers Bureau. Amgen – Advisory Committee/Board Member. Bristol myers squibb – Advisory Committee/Board Member, Speakers Bureau. Janssen – Advisory Committee/Board Member, Speakers Bureau. Lilly – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Mashary Attamimi: AbbVie – Speakers Bureau. Hikma – Speakers Bureau. Janssen – Speakers Bureau. Lilly – Speakers Bureau. Pfizer – Speakers Bureau. Sandoz – Speakers Bureau. Takeda – Speakers Bureau.
Sameer Desai indicated no relevant financial relationships.
Salman Almuammar, MBBS1, Badr Al Bawardy, MD2, Lina Alyahya, 3, Weam Mahmoud, 3, Abdulelah Almutairdi, MD1, Mashary Attamimi, MD1, Sameer Desai, 1. P1130 - Impact of Delayed Diagnosis on Outcomes in Inflammatory Bowel Disease (IBD), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia; 2Yale New Haven Hospital, New Haven, USA; King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia, New Haven, CT; 3Alfaisal University, Riyadh, Ar Riyad, Saudi Arabia
Introduction: Inflammatory Bowel Disease (IBD), encompassing Crohn’s disease (CD) and ulcerative colitis (UC), is a chronic inflammatory condition of the gastrointestinal tract. Delayed diagnosis is hypothesized to influence disease outcomes adversely, yet its impact remains underexplored, particularly in Saudi Arabia. This study investigates the association between diagnostic delay and clinical outcomes in IBD patients.
Methods: This cross-sectional study utilized data from a prospectively maintained IBD registry at King Faisal Specialist Hospital and Research Centre from September 2023 to September 2024. Inclusion criteria comprised patients aged ≥14 years with a confirmed diagnosis of IBD. Diagnostic delay, defined as the time from symptom onset to diagnosis, was categorized as < 1 year, 1–2 years, and >2 years. Clinical outcomes included the need for intestinal surgery, >2 advanced therapies, and a composite outcome (surgery, advanced therapies, or disease progression). Associations were assessed using Chi-squared and Fisher’s exact tests.
Results: The cohort included 412 patients (mean age at diagnosis: 24 years; 55% male; 68% CD, 32% UC). The average diagnostic delay was 1.48 years, with 26% experiencing delays >2 years. Patients with longer delays were more likely to have CD (p=0.049), older age at diagnosis (p=0.017), and stricturing disease phenotype in CD (p=0.013). Delayed diagnosis ( >2 years) was associated with a higher prevalence of intestinal surgery (32% vs. 23%; p=0.045) and borderline significance for the composite outcome (p=0.062). No significant associations were found between delay and use of >2 advanced therapies.
Discussion: Diagnostic delay in IBD is prevalent and associated with worse outcomes, particularly in patients with CD. Efforts to minimize diagnostic delays may improve clinical outcomes and reduce the need for surgical interventions. Further research with larger cohorts and longitudinal follow-up is warranted to elucidate these associations.
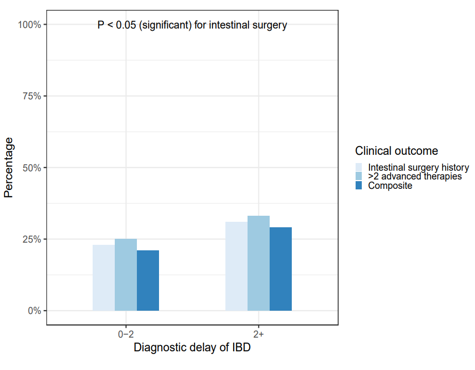
Figure: The effect of diagnostic delay in IBD
Disclosures:
Salman Almuammar indicated no relevant financial relationships.
Badr Al Bawardy: AbbVie – Advisor or Review Panel Member, Consultant, Speakers Bureau. Bristol Myers Squibb – Advisory Committee/Board Member, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Hikma – Speakers Bureau. Janssen – Advisory Committee/Board Member, Speakers Bureau. Pfizer – Advisory Committee/Board Member. TAKEDA – Advisor or Review Panel Member, Speakers Bureau.
Lina Alyahya indicated no relevant financial relationships.
Weam Mahmoud indicated no relevant financial relationships.
Abdulelah Almutairdi: AbbVie – Advisory Committee/Board Member, Speakers Bureau. Amgen – Advisory Committee/Board Member. Bristol myers squibb – Advisory Committee/Board Member, Speakers Bureau. Janssen – Advisory Committee/Board Member, Speakers Bureau. Lilly – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Mashary Attamimi: AbbVie – Speakers Bureau. Hikma – Speakers Bureau. Janssen – Speakers Bureau. Lilly – Speakers Bureau. Pfizer – Speakers Bureau. Sandoz – Speakers Bureau. Takeda – Speakers Bureau.
Sameer Desai indicated no relevant financial relationships.
Salman Almuammar, MBBS1, Badr Al Bawardy, MD2, Lina Alyahya, 3, Weam Mahmoud, 3, Abdulelah Almutairdi, MD1, Mashary Attamimi, MD1, Sameer Desai, 1. P1130 - Impact of Delayed Diagnosis on Outcomes in Inflammatory Bowel Disease (IBD), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
