Sunday Poster Session
Category: IBD
P1127 - Impact of Obesity on Recurrence and Treatment Escalation in Pouchitis After IPAA in Patients With Ulcerative Colitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Hany Habib, MD
Allegheny Health Network Medicine Institute
Pittsburgh, PA
Presenting Author(s)
Hany Habib, MD1, Himsikhar Khataniar, MD2, Gursimran Kochhar, MD3, Aakash Desai, MD3
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA
Introduction: Acute pouchitis is the most common complication after ileal pouch–anal anastomosis (IPAA) in ulcerative colitis (UC), affecting up to 50% of patients. About 10–15% progress to chronic antibiotic-dependent or -refractory pouchitis. Obesity has been associated with increased risk of pouch inflammation, but its impact on recurrence and treatment escalation remains unclear.
Methods: We conducted a retrospective cohort study using the TriNetX database to assess whether obesity influences outcomes in patients with UC-IPAA and a history of pouchitis. Patients were categorized by BMI into obese and non-obese cohorts. Non-obese cohort included BMI between 18.5 and 24.9 kg/m². The primary outcome was a composite of repeat antibiotic use or advanced therapy (AT) initiation at 1 and 2 years. Secondary outcomes included pouch excision, mesalamine and oral or topical steroid use. Subgroup analyses were conducted for BMI 30–39 and ≥40 kg/m². Adjusted odds ratios (aORs) were calculated after 1:1 propensity score matching.
Results: We identified 449 patients with obesity (mean age 44.4 ± 14.3 years; 53.9% male; 75.7% White) and 712 without obesity (mean age 35.2 ± 15.1 years; 53.3% male; 81.7% White). Within 1 and 2 years of the index pouchitis episode, there was no significant difference in the composite primary outcome between patients with and without obesity (1-year: 56.6% vs 51.2%; aOR 1.24, 95% CI 0.92–1.66, p=0.15; 2-year: 64.2% vs 58.8%; aOR 1.25, 95% CI 0.92–1.69, p=0.14). Similarly, the risk of recurrent pouchitis did not differ significantly at either timepoint. However, patients with obesity had higher AT use at both 1 year (10.7% vs 4.7%; aOR 2.38, 95% CI 1.31–4.30; p=0.003) and 2 years (14.1% vs 7.6%; aOR 1.99, 95% CI 1.21–3.26; p=0.005), as well as increased steroid use at 1 year (26.1% vs 19.7%; aOR 1.44, 95% CI 1.01–2.05; p=0.04) and 2 years (30.7% vs 23.9%; aOR 1.40, 95% CI 1.01–1.96; p=0.04). In subgroup analysis, patients with BMI 30–39 had significantly greater AT use compared to patients without obesity (15.4% vs 8.4%; aOR 1.98, 95% CI 1.23–3.18; p=0.003). At 2 years, Crohn’s-like disease of pouch occurred in 11.1% of patients with obesity vs 10.7% without obesity (p=0.83).
Discussion: Obesity was associated with an increased risk for AT initiation but not repeat antibiotic use in patients with UC-IPAA and obesity with a history of pouchitis.
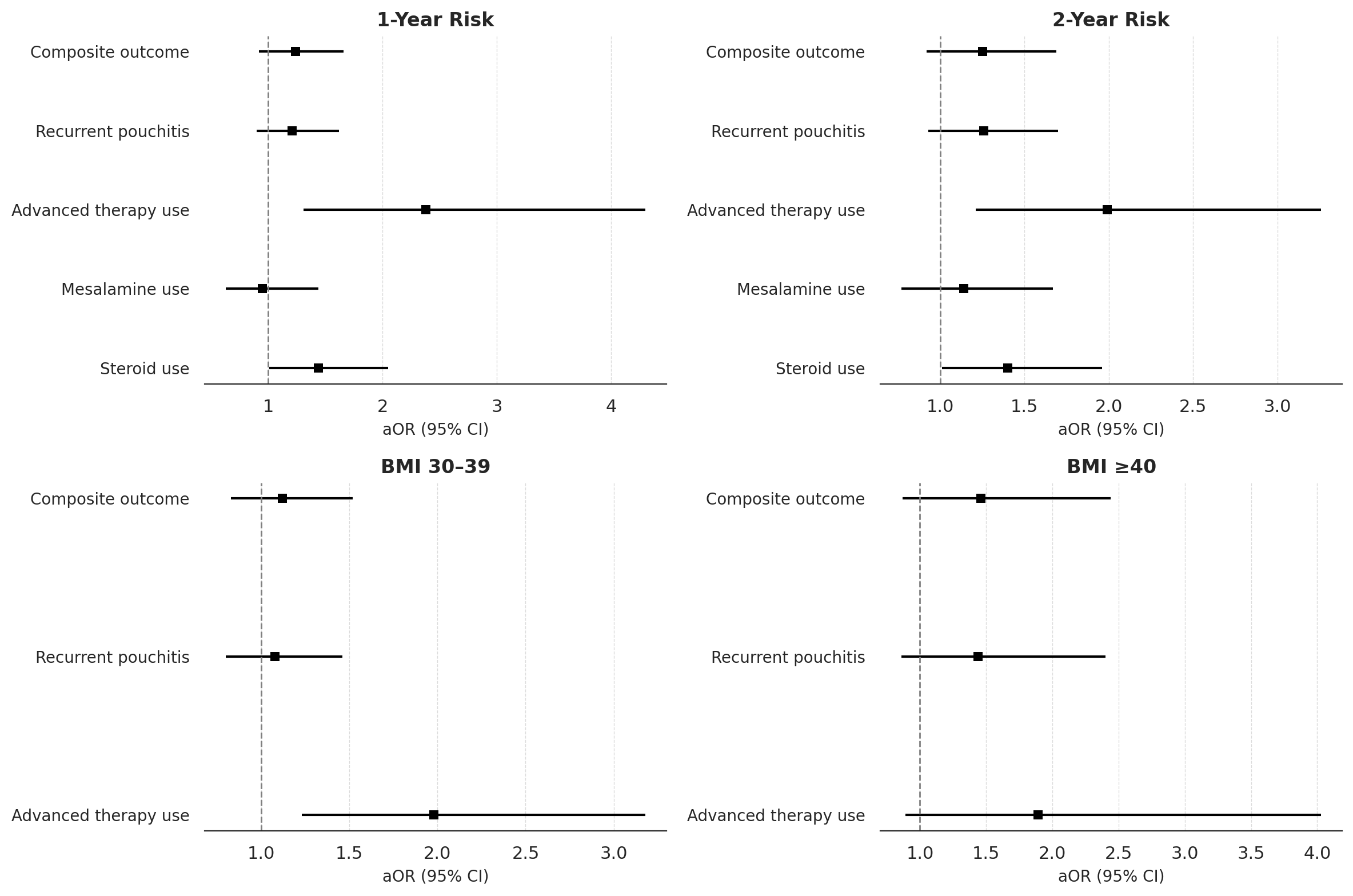
Figure: Figure 1. Forest plots comparing adjusted odds ratio of outcomes following index pouchitis episode between obese and non-obese UC-IPAA cohorts at 1-year and 2-year follow-up. Subgroup analysis shown for patients with BMI 30–39 and BMI ≥40 compared to patients without obesity.
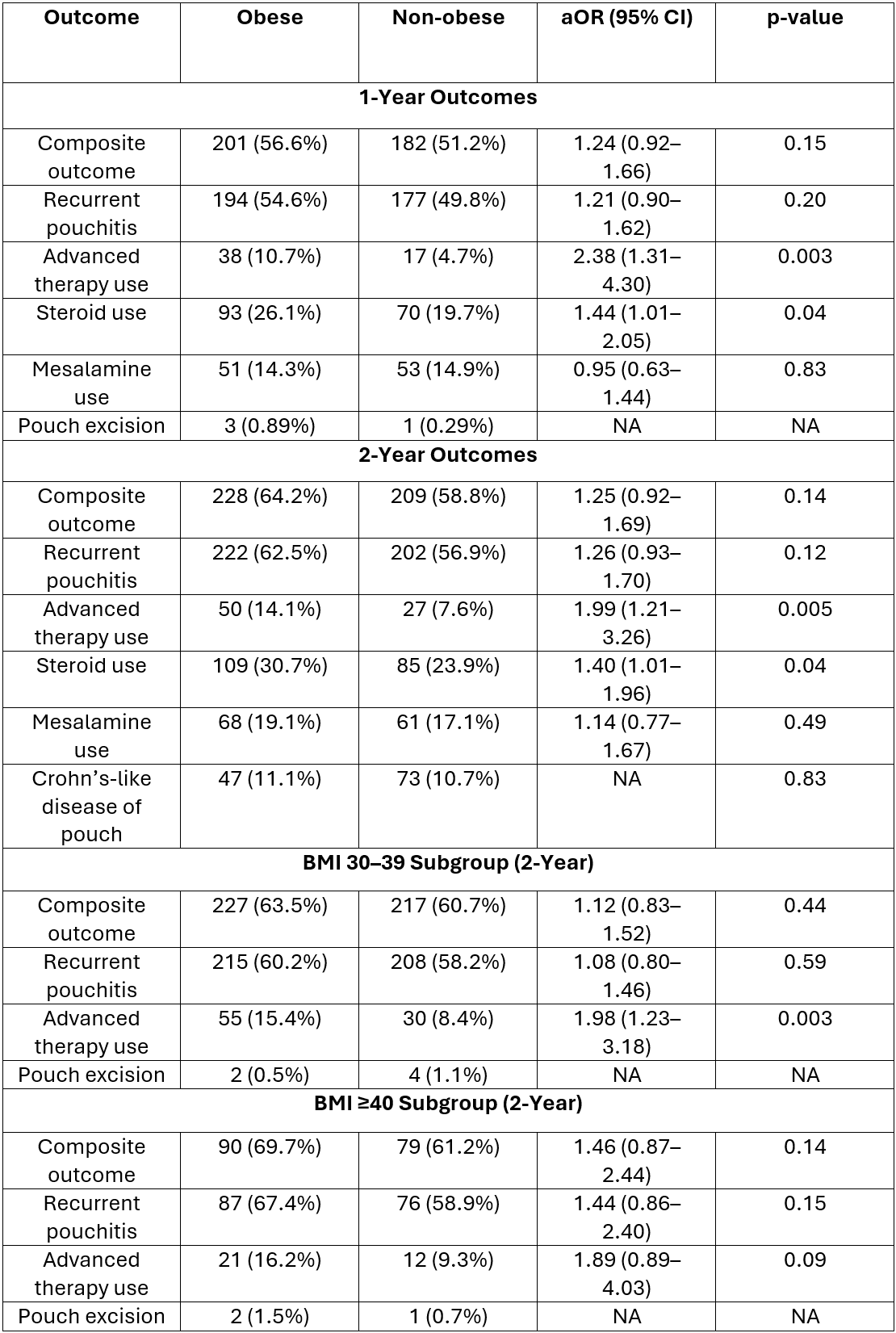
Figure: Table 1. Comparison of outcomes between obese and non-obese UC-IPAA cohorts after 1:1 propensity score matching. Outcomes assessed at 1- and 2-years following index pouchitis episode. Subgroup analyses conducted for patients with BMI 30–39 and BMI ≥40 compared to patients without obesity.
Disclosures:
Hany Habib indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Gursimran Kochhar indicated no relevant financial relationships.
Aakash Desai indicated no relevant financial relationships.
Hany Habib, MD1, Himsikhar Khataniar, MD2, Gursimran Kochhar, MD3, Aakash Desai, MD3. P1127 - Impact of Obesity on Recurrence and Treatment Escalation in Pouchitis After IPAA in Patients With Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA
Introduction: Acute pouchitis is the most common complication after ileal pouch–anal anastomosis (IPAA) in ulcerative colitis (UC), affecting up to 50% of patients. About 10–15% progress to chronic antibiotic-dependent or -refractory pouchitis. Obesity has been associated with increased risk of pouch inflammation, but its impact on recurrence and treatment escalation remains unclear.
Methods: We conducted a retrospective cohort study using the TriNetX database to assess whether obesity influences outcomes in patients with UC-IPAA and a history of pouchitis. Patients were categorized by BMI into obese and non-obese cohorts. Non-obese cohort included BMI between 18.5 and 24.9 kg/m². The primary outcome was a composite of repeat antibiotic use or advanced therapy (AT) initiation at 1 and 2 years. Secondary outcomes included pouch excision, mesalamine and oral or topical steroid use. Subgroup analyses were conducted for BMI 30–39 and ≥40 kg/m². Adjusted odds ratios (aORs) were calculated after 1:1 propensity score matching.
Results: We identified 449 patients with obesity (mean age 44.4 ± 14.3 years; 53.9% male; 75.7% White) and 712 without obesity (mean age 35.2 ± 15.1 years; 53.3% male; 81.7% White). Within 1 and 2 years of the index pouchitis episode, there was no significant difference in the composite primary outcome between patients with and without obesity (1-year: 56.6% vs 51.2%; aOR 1.24, 95% CI 0.92–1.66, p=0.15; 2-year: 64.2% vs 58.8%; aOR 1.25, 95% CI 0.92–1.69, p=0.14). Similarly, the risk of recurrent pouchitis did not differ significantly at either timepoint. However, patients with obesity had higher AT use at both 1 year (10.7% vs 4.7%; aOR 2.38, 95% CI 1.31–4.30; p=0.003) and 2 years (14.1% vs 7.6%; aOR 1.99, 95% CI 1.21–3.26; p=0.005), as well as increased steroid use at 1 year (26.1% vs 19.7%; aOR 1.44, 95% CI 1.01–2.05; p=0.04) and 2 years (30.7% vs 23.9%; aOR 1.40, 95% CI 1.01–1.96; p=0.04). In subgroup analysis, patients with BMI 30–39 had significantly greater AT use compared to patients without obesity (15.4% vs 8.4%; aOR 1.98, 95% CI 1.23–3.18; p=0.003). At 2 years, Crohn’s-like disease of pouch occurred in 11.1% of patients with obesity vs 10.7% without obesity (p=0.83).
Discussion: Obesity was associated with an increased risk for AT initiation but not repeat antibiotic use in patients with UC-IPAA and obesity with a history of pouchitis.
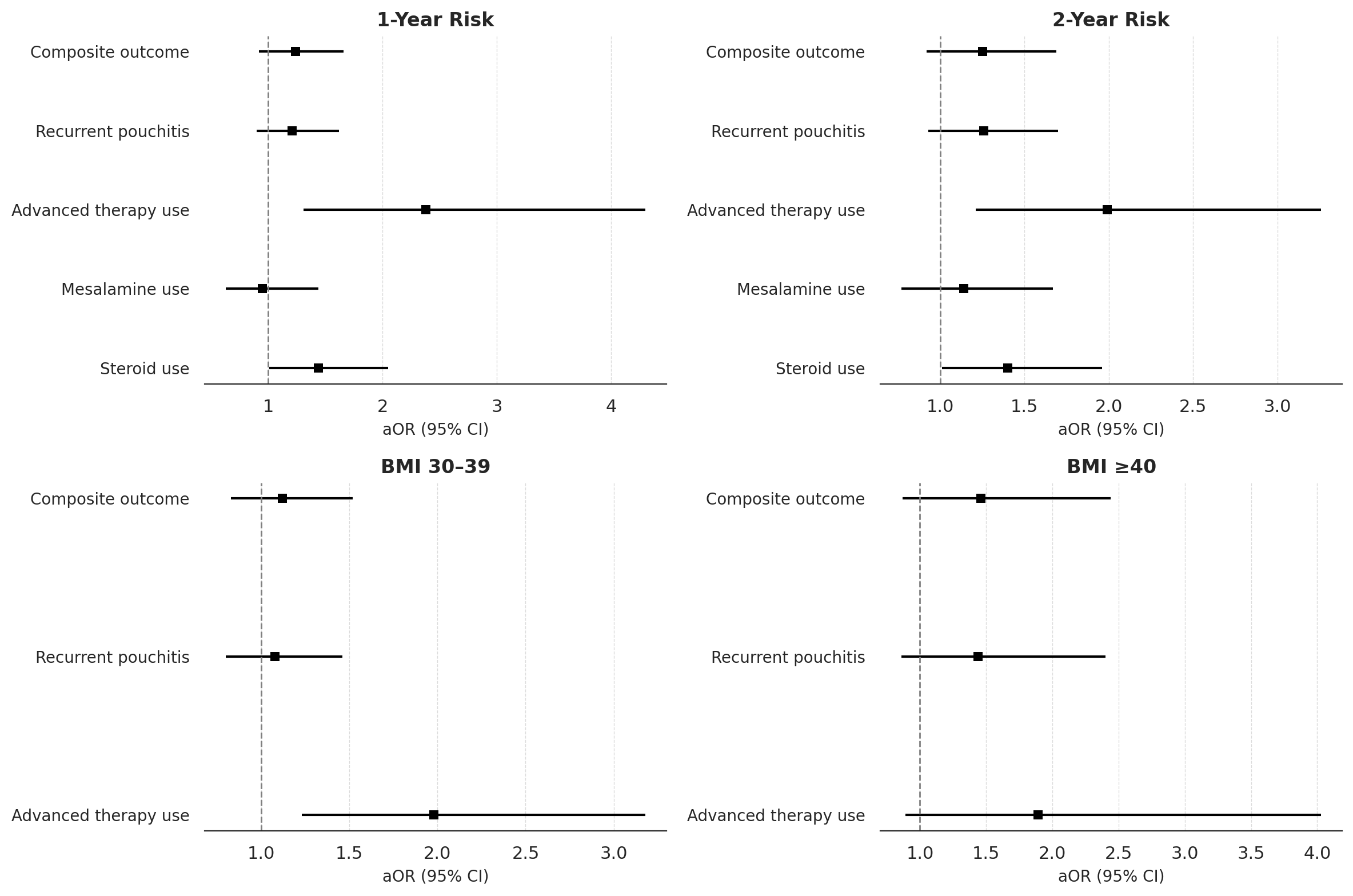
Figure: Figure 1. Forest plots comparing adjusted odds ratio of outcomes following index pouchitis episode between obese and non-obese UC-IPAA cohorts at 1-year and 2-year follow-up. Subgroup analysis shown for patients with BMI 30–39 and BMI ≥40 compared to patients without obesity.
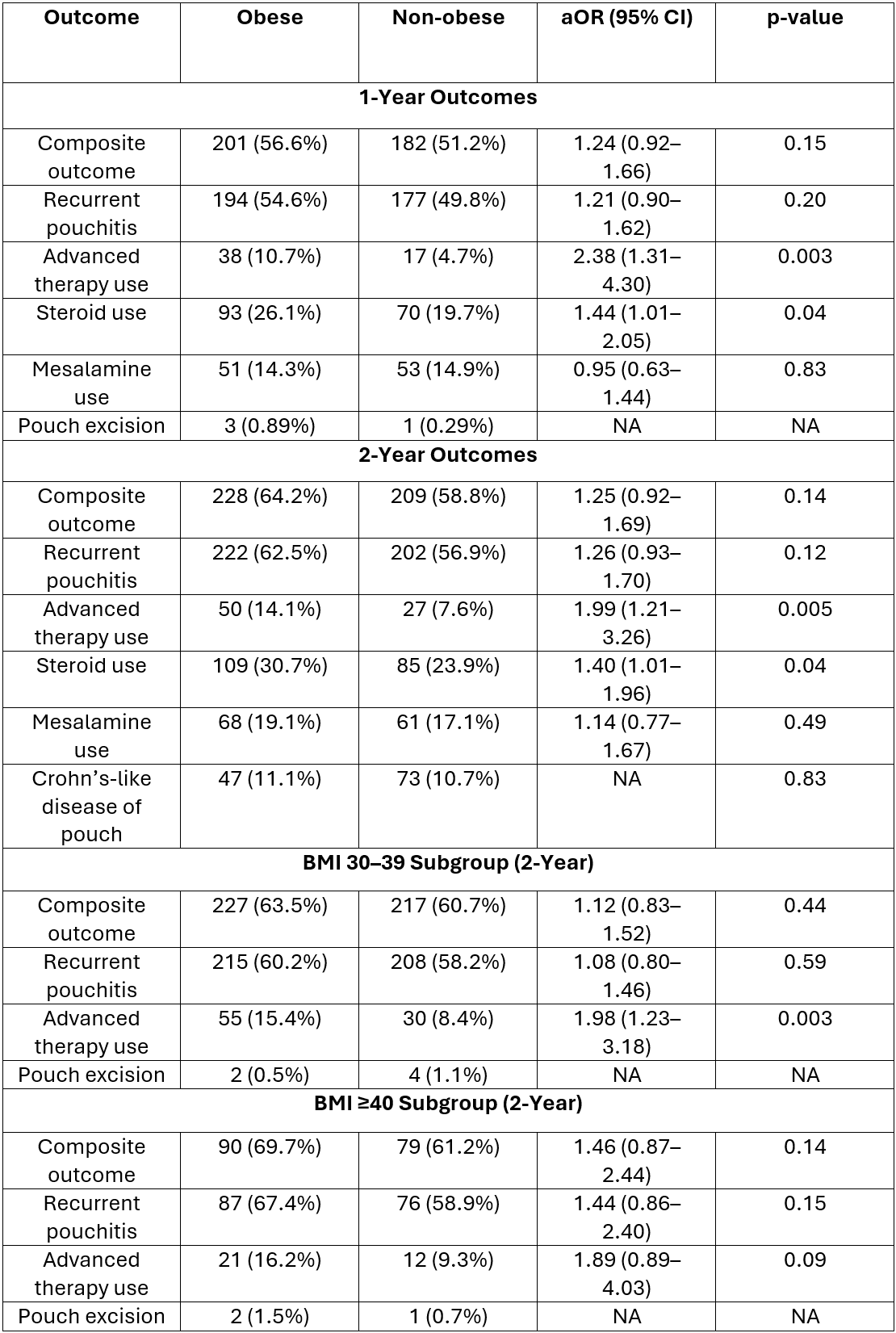
Figure: Table 1. Comparison of outcomes between obese and non-obese UC-IPAA cohorts after 1:1 propensity score matching. Outcomes assessed at 1- and 2-years following index pouchitis episode. Subgroup analyses conducted for patients with BMI 30–39 and BMI ≥40 compared to patients without obesity.
Disclosures:
Hany Habib indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Gursimran Kochhar indicated no relevant financial relationships.
Aakash Desai indicated no relevant financial relationships.
Hany Habib, MD1, Himsikhar Khataniar, MD2, Gursimran Kochhar, MD3, Aakash Desai, MD3. P1127 - Impact of Obesity on Recurrence and Treatment Escalation in Pouchitis After IPAA in Patients With Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
