Sunday Poster Session
Category: IBD
P1116 - Inflammatory Markers and Disease History Associated With Vitamin C Deficiency in Inflammatory Bowel Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- KT
Kathryn Thompson, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Kathryn Thompson, MD, Nicole Ruiz, MD, Hayalneh Gessessew, MD, William Breaux, MD, Jasna Beard, MD
Emory University School of Medicine, Atlanta, GA
Introduction: Though many micronutrient deficiencies are well-established in patients with inflammatory bowel disease (IBD), Vitamin C deficiency (VCD) is not well-studied in this population. Further, it is unknown if VCD is associated with IBD disease severity or other characteristics of disease history. The aim of this study was to identify whether inflammatory markers and IBD disease history are associated with VCD.
Methods: A retrospective cohort analysis was conducted in patients treated for IBD at Emory University clinics with a serum Vitamin C level from 12/2019-09/2024. Demographic data, IBD disease history, Vitamin C level, and inflammatory markers (C-reactive protein (CRP) and fecal calprotectin (FC)) were reviewed. CRP was defined as elevated if value was > 10 mg/L. Chi-square test and univariate logistic regression were used to assess if inflammatory markers and disease history were associated with VCD.
Results: Of 230 patients with IBD, 72 (32.2%) had VCD. Of the patients with VCD, the mean CRP was 43.5 mg/L and the median CRP was 15.8 mg/L which was statistically significantly higher compared to patients without VCD (p=0.04 and 0.003, respectively). Of the patients with VCD, the mean FC was 536.9 ug/g and the median FC was 162 ug/g of which the median was statistically significantly higher compared to patients without VCD (p=0.12 and 0.04, respectively). Despite this correlation, there was no statistically significant difference in IBD disease severity, presence of small bowel disease, history of small bowel resection, presence of extraintestinal manifestations, or use of immunomodulators or biologics in patients with and without VCD (Table 1). Using a univariate logistic regression, having an elevated CRP vs. a normal CRP resulted in an odds ratio (OR) of 2.18 (95% CI (1.21, 3.93), p=0.01) for VCD. However, univariate logistic regression showed that FC and other IBD disease characteristics did not have a statistically significant association with VCD (Table 2).
Discussion: Patients with VCD had a statistically significantly higher mean and median CRP and median FC compared to patients without VCD. The discrepancy between the mean and median CRP and FC is likely explained by outliers, specifically patients with significantly higher inflammatory markers compared to other patients in this cohort. IBD disease severity and other characteristics of disease history were not associated with VCD. This study suggests that acute inflammation, such as in IBD flares, may predispose patients to VCD.
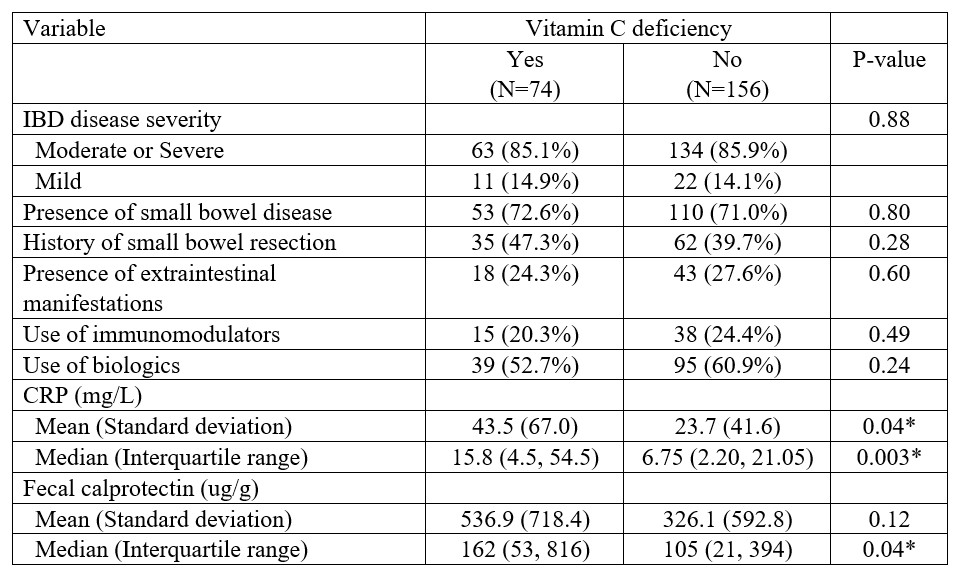
Figure: Table 1. Chi-square test of inflammatory markers and IBD disease history in patients with and without Vitamin C deficiency.
*Indicates statistically significant difference (p-value < 0.05)
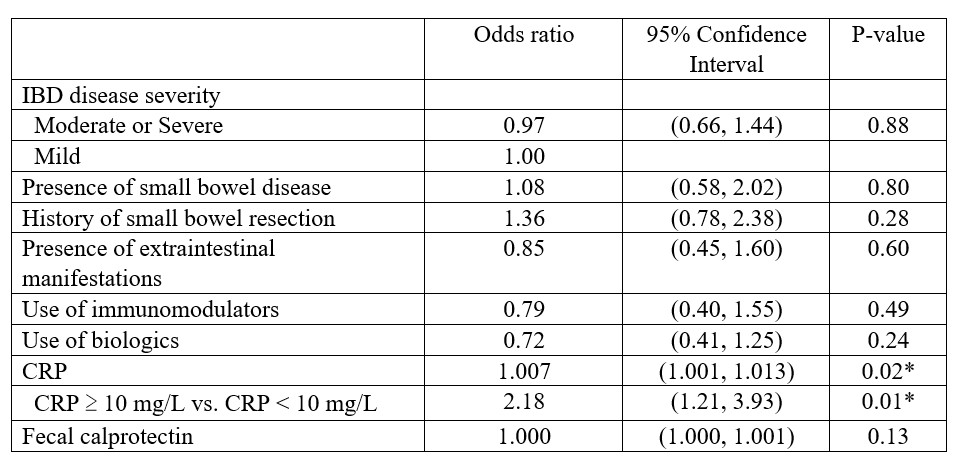
Figure: Table 2. Univariate logistic regression identifying inflammatory markers and IBD disease history associated with Vitamin C deficiency.
*Indicates statistically significant value (p-value < 0.05)
Disclosures:
Kathryn Thompson indicated no relevant financial relationships.
Nicole Ruiz indicated no relevant financial relationships.
Hayalneh Gessessew indicated no relevant financial relationships.
William Breaux indicated no relevant financial relationships.
Jasna Beard indicated no relevant financial relationships.
Kathryn Thompson, MD, Nicole Ruiz, MD, Hayalneh Gessessew, MD, William Breaux, MD, Jasna Beard, MD. P1116 - Inflammatory Markers and Disease History Associated With Vitamin C Deficiency in Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Emory University School of Medicine, Atlanta, GA
Introduction: Though many micronutrient deficiencies are well-established in patients with inflammatory bowel disease (IBD), Vitamin C deficiency (VCD) is not well-studied in this population. Further, it is unknown if VCD is associated with IBD disease severity or other characteristics of disease history. The aim of this study was to identify whether inflammatory markers and IBD disease history are associated with VCD.
Methods: A retrospective cohort analysis was conducted in patients treated for IBD at Emory University clinics with a serum Vitamin C level from 12/2019-09/2024. Demographic data, IBD disease history, Vitamin C level, and inflammatory markers (C-reactive protein (CRP) and fecal calprotectin (FC)) were reviewed. CRP was defined as elevated if value was > 10 mg/L. Chi-square test and univariate logistic regression were used to assess if inflammatory markers and disease history were associated with VCD.
Results: Of 230 patients with IBD, 72 (32.2%) had VCD. Of the patients with VCD, the mean CRP was 43.5 mg/L and the median CRP was 15.8 mg/L which was statistically significantly higher compared to patients without VCD (p=0.04 and 0.003, respectively). Of the patients with VCD, the mean FC was 536.9 ug/g and the median FC was 162 ug/g of which the median was statistically significantly higher compared to patients without VCD (p=0.12 and 0.04, respectively). Despite this correlation, there was no statistically significant difference in IBD disease severity, presence of small bowel disease, history of small bowel resection, presence of extraintestinal manifestations, or use of immunomodulators or biologics in patients with and without VCD (Table 1). Using a univariate logistic regression, having an elevated CRP vs. a normal CRP resulted in an odds ratio (OR) of 2.18 (95% CI (1.21, 3.93), p=0.01) for VCD. However, univariate logistic regression showed that FC and other IBD disease characteristics did not have a statistically significant association with VCD (Table 2).
Discussion: Patients with VCD had a statistically significantly higher mean and median CRP and median FC compared to patients without VCD. The discrepancy between the mean and median CRP and FC is likely explained by outliers, specifically patients with significantly higher inflammatory markers compared to other patients in this cohort. IBD disease severity and other characteristics of disease history were not associated with VCD. This study suggests that acute inflammation, such as in IBD flares, may predispose patients to VCD.
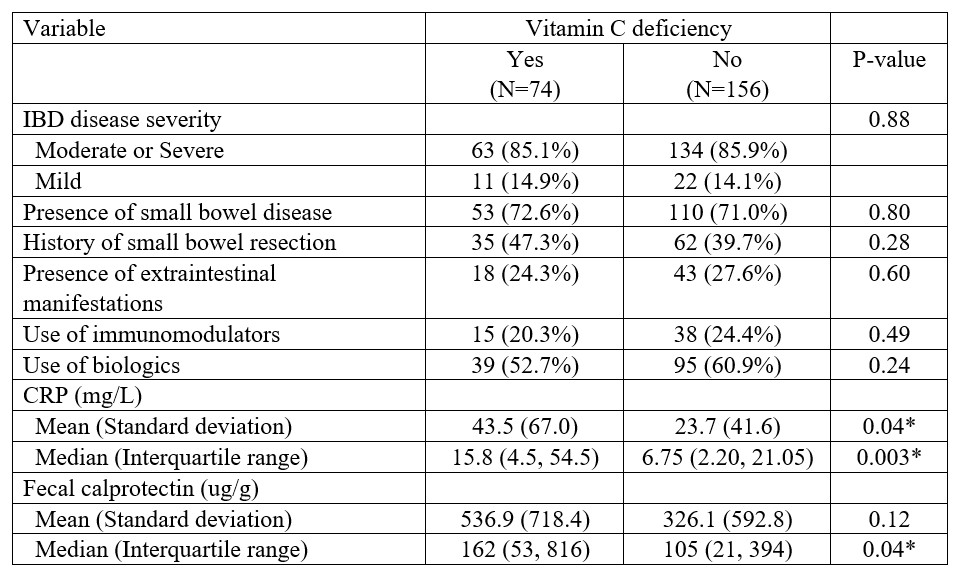
Figure: Table 1. Chi-square test of inflammatory markers and IBD disease history in patients with and without Vitamin C deficiency.
*Indicates statistically significant difference (p-value < 0.05)
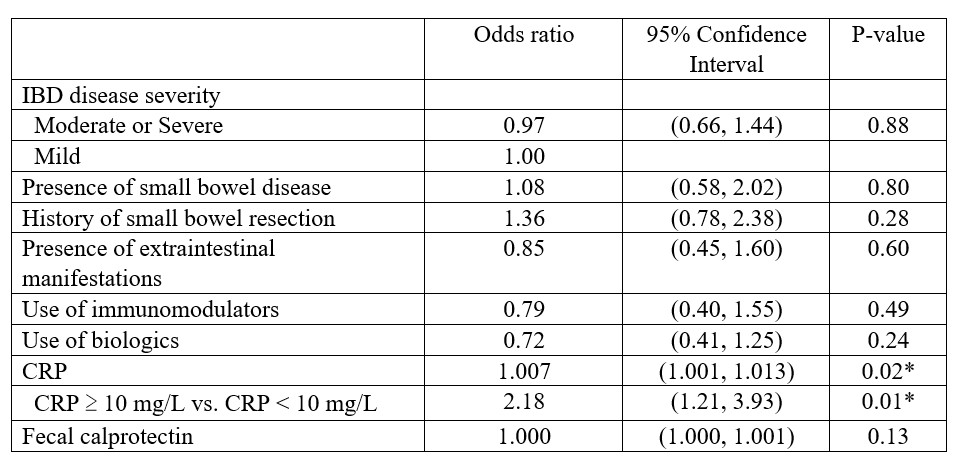
Figure: Table 2. Univariate logistic regression identifying inflammatory markers and IBD disease history associated with Vitamin C deficiency.
*Indicates statistically significant value (p-value < 0.05)
Disclosures:
Kathryn Thompson indicated no relevant financial relationships.
Nicole Ruiz indicated no relevant financial relationships.
Hayalneh Gessessew indicated no relevant financial relationships.
William Breaux indicated no relevant financial relationships.
Jasna Beard indicated no relevant financial relationships.
Kathryn Thompson, MD, Nicole Ruiz, MD, Hayalneh Gessessew, MD, William Breaux, MD, Jasna Beard, MD. P1116 - Inflammatory Markers and Disease History Associated With Vitamin C Deficiency in Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
