Sunday Poster Session
Category: IBD
P1084 - Absence of Pseudopolyps and Submucosal Edema on Abdominopelvic CT Are Associated with Increased Mortality in Toxic Megacolon
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Joseph Gunderson, MD
University of Texas Southwestern Medical Center
Dallas, TX
Presenting Author(s)
Joseph Gunderson, MD1, David J. Schaub, MD2, Christopher Miller, MD3, Alisia C. Gunderson, MD1, Fariba Hossain, BS4, Chiu-Hsieh Hsu, PhD5, Sasha Taleban, MD, FACG4
1University of Texas Southwestern Medical Center, Dallas, TX; 2Banner - University of Arizona Tucson, Tucson, AZ; 3Banner University Medical Center Tucson, Tucson, AZ; 4University of Arizona College of Medicine, Tucson, AZ; 5University of Arizona, Tucson, AZ
Introduction: Toxic megacolon (TM) is a rare, life-threatening complication of inflammatory bowel disease (IBD) and other etiologies. While diagnosis has classically relied on radiographic imaging, few studies have explored the role of computed tomography (CT) in TM. This study aims to describe common CT findings in TM, their prevalence across TM etiologies, and their impact on clinical outcomes.
Methods: We conducted a retrospective analysis of patients ≥18 years old with TM from January 2014 to June 2024 using ICD-9/10 codes across 1,238 Banner Health sites. Patients with verified TM who underwent contrast-enhanced abdominopelvic CT within 48 hours of diagnosis were included. Data on TM etiologies, demographics, clinical features, and treatment were collected. CT images were reviewed by an abdominal radiologist blinded to imaging reports. The primary outcome was 30-day mortality. Statistical analysis included Fisher’s exact test and ANOVA.
Results: We identified 70 patients with TM who underwent CT (median age 62 years, 42.9% female, 71.4% non-Hispanic White). TM etiologies included Clostridioides difficile (C. diff) (38.6%), ischemic colitis (IsC) (28.6%), IBD (25.7%), and others (7.7%).
The most common CT findings included loss of haustra (95.7%), colonic distention >6 cm (94.3%), colonic wall thickening (85.7%), peri-colonic fat stranding (85.7%), submucosal edema (50%), colonic wall thinning (45.7%), ascites (42.9%), small bowel distention (20%), and pseudopolyps (12.9%). The median colonic diameter was 8.8 cm.
Loss of haustra was less common in IsC (85% vs. 100% for IBD vs. 100% for C. diff, P = 0.045) while pseudopolyps were more common in IBD (33.3% vs. 3.7% for C. diff vs. 5% for IsC, P = 0.008). Pneumatosis coli was more common in IsC (20% vs. 5.6% for IBD vs. 0% for C. diff, P = 0.041).
The colon perforation rate was 28.6% (N = 20); 9 perforations were detected via imaging. The colectomy rate was 55.7%.
The 30-day mortality rate was 32.9% (N = 23). The absence of pseudopolyps (37.7% vs. 0%, P = 0.025) and submucosal edema (45.7% vs. 20%, P = 0.041) were associated with increased 30-day mortality.
Discussion: We identified several common CT findings in TM. While IsC was linked to pneumatosis coli, IBD and C. diff were more commonly associated with sequelae of chronic inflammation. The absence of submucosal edema and pseudopolyps are associated with increased mortality in TM. Additional studies are needed to further assess the role of CT in TM diagnosis, treatment, and impact on outcomes.
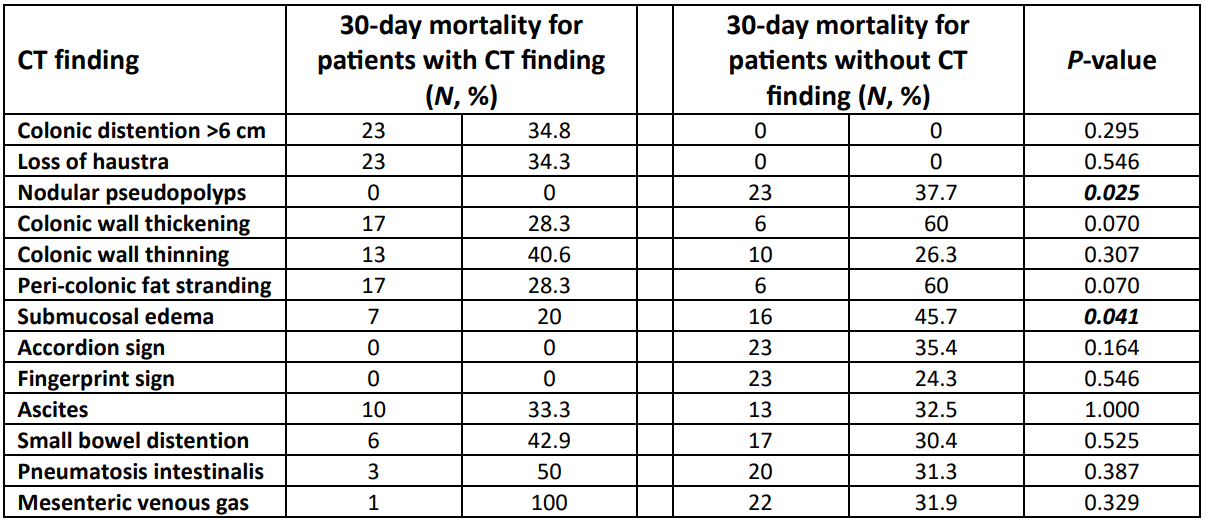
Figure: Table 1. Prevalence of each computed tomography (CT) finding across the most common toxic megacolon etiologies
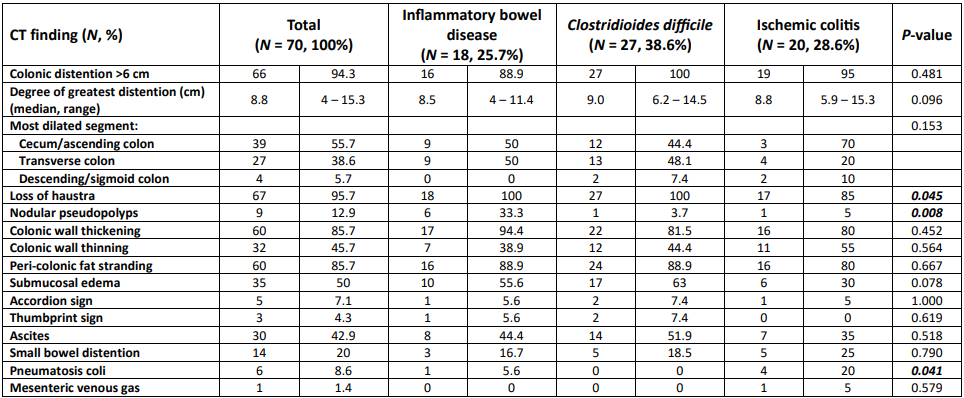
Figure: Table 2. 30-day mortality in patients with and without specific computed tomography (CT) findings in toxic megacolon
Disclosures:
Joseph Gunderson indicated no relevant financial relationships.
David Schaub indicated no relevant financial relationships.
Christopher Miller indicated no relevant financial relationships.
Alisia Gunderson indicated no relevant financial relationships.
Fariba Hossain indicated no relevant financial relationships.
Chiu-Hsieh Hsu indicated no relevant financial relationships.
Sasha Taleban: AbbVie – Grant/Research Support. Boehringer-Ingelheim – Grant/Research Support. Eli Lilly – Grant/Research Support. Janssen – Advisory Committee/Board Member, Grant/Research Support. Pfizer – Grant/Research Support. Takeda – Grant/Research Support.
Joseph Gunderson, MD1, David J. Schaub, MD2, Christopher Miller, MD3, Alisia C. Gunderson, MD1, Fariba Hossain, BS4, Chiu-Hsieh Hsu, PhD5, Sasha Taleban, MD, FACG4. P1084 - Absence of Pseudopolyps and Submucosal Edema on Abdominopelvic CT Are Associated with Increased Mortality in Toxic Megacolon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Southwestern Medical Center, Dallas, TX; 2Banner - University of Arizona Tucson, Tucson, AZ; 3Banner University Medical Center Tucson, Tucson, AZ; 4University of Arizona College of Medicine, Tucson, AZ; 5University of Arizona, Tucson, AZ
Introduction: Toxic megacolon (TM) is a rare, life-threatening complication of inflammatory bowel disease (IBD) and other etiologies. While diagnosis has classically relied on radiographic imaging, few studies have explored the role of computed tomography (CT) in TM. This study aims to describe common CT findings in TM, their prevalence across TM etiologies, and their impact on clinical outcomes.
Methods: We conducted a retrospective analysis of patients ≥18 years old with TM from January 2014 to June 2024 using ICD-9/10 codes across 1,238 Banner Health sites. Patients with verified TM who underwent contrast-enhanced abdominopelvic CT within 48 hours of diagnosis were included. Data on TM etiologies, demographics, clinical features, and treatment were collected. CT images were reviewed by an abdominal radiologist blinded to imaging reports. The primary outcome was 30-day mortality. Statistical analysis included Fisher’s exact test and ANOVA.
Results: We identified 70 patients with TM who underwent CT (median age 62 years, 42.9% female, 71.4% non-Hispanic White). TM etiologies included Clostridioides difficile (C. diff) (38.6%), ischemic colitis (IsC) (28.6%), IBD (25.7%), and others (7.7%).
The most common CT findings included loss of haustra (95.7%), colonic distention >6 cm (94.3%), colonic wall thickening (85.7%), peri-colonic fat stranding (85.7%), submucosal edema (50%), colonic wall thinning (45.7%), ascites (42.9%), small bowel distention (20%), and pseudopolyps (12.9%). The median colonic diameter was 8.8 cm.
Loss of haustra was less common in IsC (85% vs. 100% for IBD vs. 100% for C. diff, P = 0.045) while pseudopolyps were more common in IBD (33.3% vs. 3.7% for C. diff vs. 5% for IsC, P = 0.008). Pneumatosis coli was more common in IsC (20% vs. 5.6% for IBD vs. 0% for C. diff, P = 0.041).
The colon perforation rate was 28.6% (N = 20); 9 perforations were detected via imaging. The colectomy rate was 55.7%.
The 30-day mortality rate was 32.9% (N = 23). The absence of pseudopolyps (37.7% vs. 0%, P = 0.025) and submucosal edema (45.7% vs. 20%, P = 0.041) were associated with increased 30-day mortality.
Discussion: We identified several common CT findings in TM. While IsC was linked to pneumatosis coli, IBD and C. diff were more commonly associated with sequelae of chronic inflammation. The absence of submucosal edema and pseudopolyps are associated with increased mortality in TM. Additional studies are needed to further assess the role of CT in TM diagnosis, treatment, and impact on outcomes.
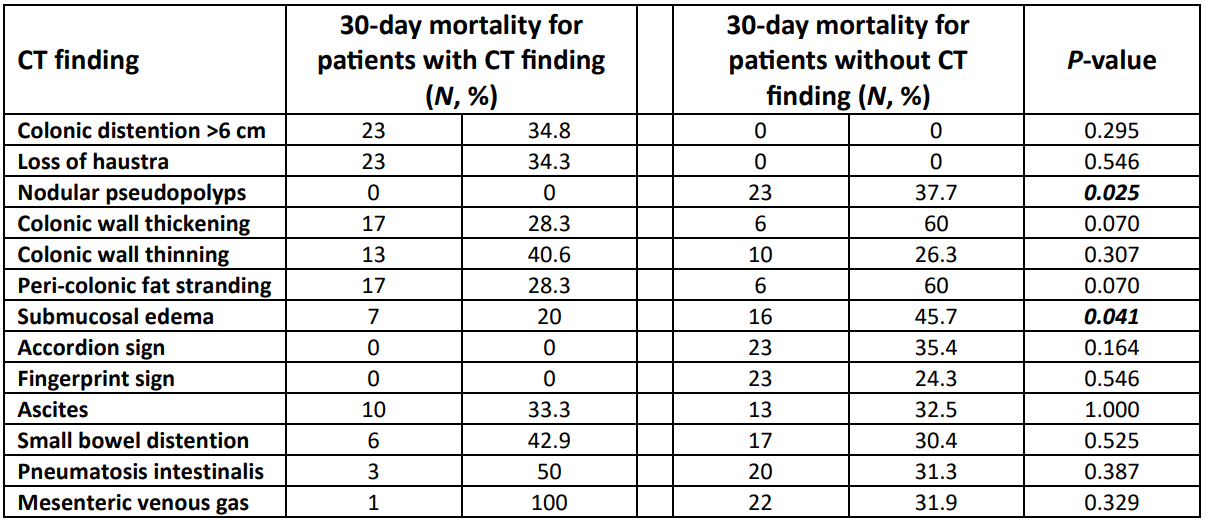
Figure: Table 1. Prevalence of each computed tomography (CT) finding across the most common toxic megacolon etiologies
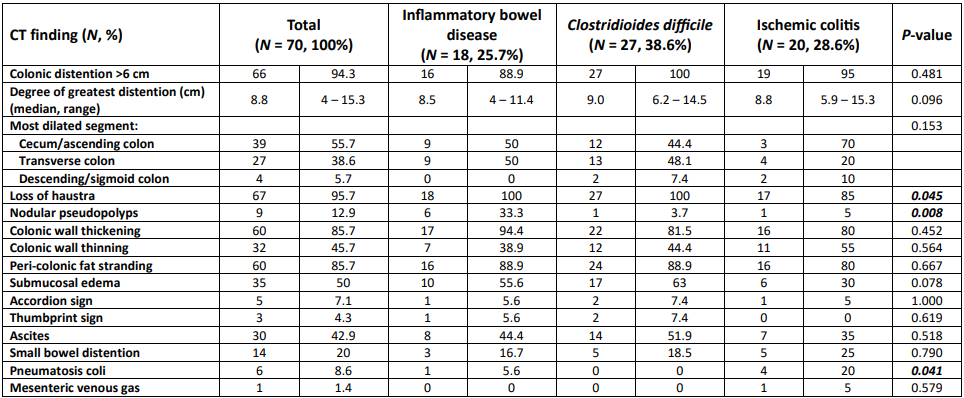
Figure: Table 2. 30-day mortality in patients with and without specific computed tomography (CT) findings in toxic megacolon
Disclosures:
Joseph Gunderson indicated no relevant financial relationships.
David Schaub indicated no relevant financial relationships.
Christopher Miller indicated no relevant financial relationships.
Alisia Gunderson indicated no relevant financial relationships.
Fariba Hossain indicated no relevant financial relationships.
Chiu-Hsieh Hsu indicated no relevant financial relationships.
Sasha Taleban: AbbVie – Grant/Research Support. Boehringer-Ingelheim – Grant/Research Support. Eli Lilly – Grant/Research Support. Janssen – Advisory Committee/Board Member, Grant/Research Support. Pfizer – Grant/Research Support. Takeda – Grant/Research Support.
Joseph Gunderson, MD1, David J. Schaub, MD2, Christopher Miller, MD3, Alisia C. Gunderson, MD1, Fariba Hossain, BS4, Chiu-Hsieh Hsu, PhD5, Sasha Taleban, MD, FACG4. P1084 - Absence of Pseudopolyps and Submucosal Edema on Abdominopelvic CT Are Associated with Increased Mortality in Toxic Megacolon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

