Sunday Poster Session
Category: IBD
P1077 - Impact of Tobacco Use in Patients With Inflammatory Bowel Disease: Nationwide Propensity-Matched Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohamed Eldesouki, MD
Saint Michael's Medical Center, New York Medical College
Newark, NJ
Presenting Author(s)
Mohamed Eldesouki, MD1, Mohammad Kloub, MD2, Abdulrahman Abusalim, MD3, Khaled Elfert, MBChB, MRCP4, Mohammed Y. Youssef, MD5, Mohammad Nabil Rayad, MD6, Yashwita Sai Pulakurthi, MD7, Kanwarpreet Tandon, MBBS4
1Saint Michael's Medical Center, New York Medical College, Newark, NJ; 2New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 3University of Wisconsin School of Medicine and Public Health, Madison, WI; 4West Virginia University School of Medicine, Morgantown, WV; 5Hunt Regional Medical Center, Greenville, TX; 6New York Medical College - Saint Micheal’s Medical Center, Newark, NJ; 7New York Medical College - Saint Michael's Medical Center, Newark, NJ
Introduction: Smoking has been shown to be an influential factor in patients with inflammatory bowel diseases (IBD), including ulcerative colitis (UC) and Crohn’s disease (CD). However, its impact on inpatient outcomes of IBD remains unclear. In this study, we aim to assess the effects of smoking on clinical outcomes in patients with UC and CD, using a large inpatient dataset.
Methods: We conducted a retrospective cohort study using data from the National Inpatient Sample (NIS) spanning from 2016 to 2019. Patients with UC and CD were identified using ICD-10 codes. Then, they were stratified according to the smoking status. A propensity score matching was utilized to balance relevant comorbidities between each group. Outcomes of interest included steroid use, surgeries, gastrointestinal (GI) bleeding, perianal abscess, and mortality. Statistical analysis was performed using Stata 17. Chi-square (for categorical variables), and t-tests (for continuous variables) were used to compare the baseline characteristics between the study groups. Odds ratios (ORs) with 95% confidence intervals (CIs) were used to compare the outcomes during the hospitalization.
Results: A total of 413,208 patients were included in our study, 180,558 patients had UC, and 232,650 patients had CD. After propensity-score matching, we had a total of 151,106 patients: 39,616 patients had UC, with a total of 19,808 in each group. The CD patients were 111,490, with a total of 55,745 patients in each group. For UC patients, smokers had lower odds of steroid use (aOR = 0.69, 95% CI = [0.61 - 0.79], p = 0.001), and all-cause mortality (aOR = 0.69, 95% CI = [0.3 - 0.96], p = 0.032). For CD patients, they had higher odds of steroid use (aOR = 1.13, 95% CI = [1.03 - 1.25], p = 0.009), and perianal abscess (aOR = 1.12, 95% CI = [1.10 - 1.36], p = 0.001). CD smokers recorded lower odds of all-cause mortality (aOR = 0.51, 95% CI = [0.27 - 0.98], p = 0.04). All other outcomes were non-statistically significant between the study cohorts.
Discussion: Smoking in hospitalized UC patients was associated with lower steroid use, while in CD patients, it correlated with higher steroid use and increased odds of perianal abscess. These findings highlight the complex impact of smoking on IBD outcomes, warranting further investigation into its clinical implications.
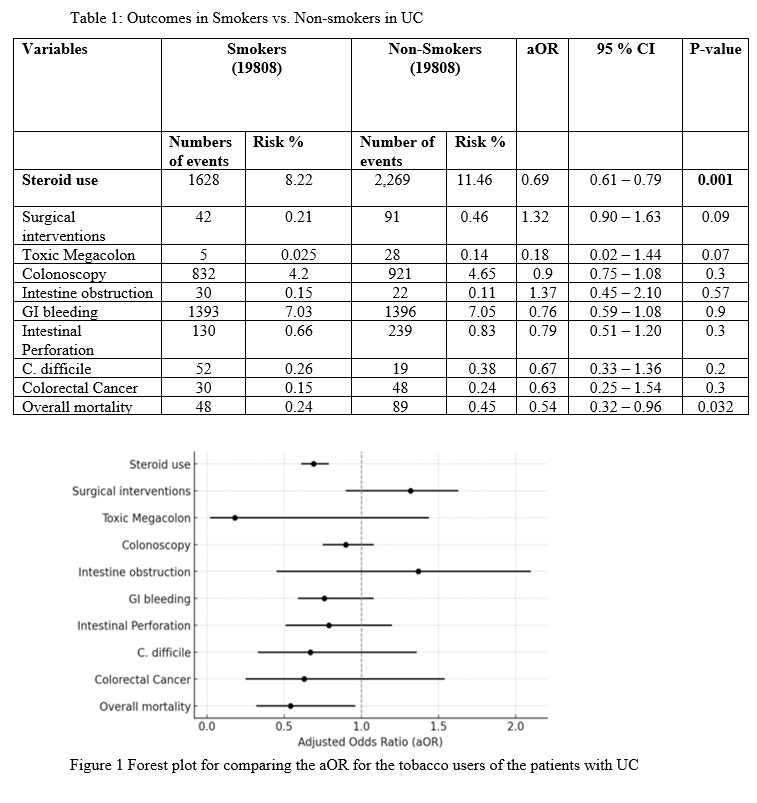
Figure: Outcomes in patients with UC (smokers vs non-smokers)
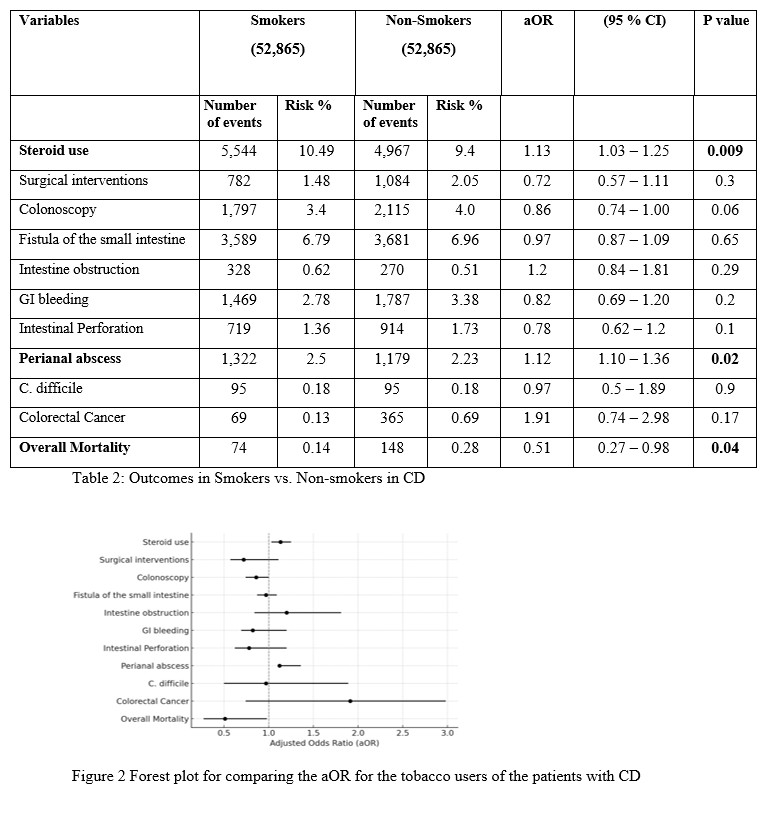
Figure: Outcomes in patients with CD (smokers vs non-smokers)
Disclosures:
Mohamed Eldesouki indicated no relevant financial relationships.
Mohammad Kloub indicated no relevant financial relationships.
Abdulrahman Abusalim indicated no relevant financial relationships.
Khaled Elfert indicated no relevant financial relationships.
Mohammed Y. Youssef indicated no relevant financial relationships.
Mohammad Nabil Rayad indicated no relevant financial relationships.
Yashwita Sai Pulakurthi indicated no relevant financial relationships.
Kanwarpreet Tandon indicated no relevant financial relationships.
Mohamed Eldesouki, MD1, Mohammad Kloub, MD2, Abdulrahman Abusalim, MD3, Khaled Elfert, MBChB, MRCP4, Mohammed Y. Youssef, MD5, Mohammad Nabil Rayad, MD6, Yashwita Sai Pulakurthi, MD7, Kanwarpreet Tandon, MBBS4. P1077 - Impact of Tobacco Use in Patients With Inflammatory Bowel Disease: Nationwide Propensity-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Michael's Medical Center, New York Medical College, Newark, NJ; 2New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 3University of Wisconsin School of Medicine and Public Health, Madison, WI; 4West Virginia University School of Medicine, Morgantown, WV; 5Hunt Regional Medical Center, Greenville, TX; 6New York Medical College - Saint Micheal’s Medical Center, Newark, NJ; 7New York Medical College - Saint Michael's Medical Center, Newark, NJ
Introduction: Smoking has been shown to be an influential factor in patients with inflammatory bowel diseases (IBD), including ulcerative colitis (UC) and Crohn’s disease (CD). However, its impact on inpatient outcomes of IBD remains unclear. In this study, we aim to assess the effects of smoking on clinical outcomes in patients with UC and CD, using a large inpatient dataset.
Methods: We conducted a retrospective cohort study using data from the National Inpatient Sample (NIS) spanning from 2016 to 2019. Patients with UC and CD were identified using ICD-10 codes. Then, they were stratified according to the smoking status. A propensity score matching was utilized to balance relevant comorbidities between each group. Outcomes of interest included steroid use, surgeries, gastrointestinal (GI) bleeding, perianal abscess, and mortality. Statistical analysis was performed using Stata 17. Chi-square (for categorical variables), and t-tests (for continuous variables) were used to compare the baseline characteristics between the study groups. Odds ratios (ORs) with 95% confidence intervals (CIs) were used to compare the outcomes during the hospitalization.
Results: A total of 413,208 patients were included in our study, 180,558 patients had UC, and 232,650 patients had CD. After propensity-score matching, we had a total of 151,106 patients: 39,616 patients had UC, with a total of 19,808 in each group. The CD patients were 111,490, with a total of 55,745 patients in each group. For UC patients, smokers had lower odds of steroid use (aOR = 0.69, 95% CI = [0.61 - 0.79], p = 0.001), and all-cause mortality (aOR = 0.69, 95% CI = [0.3 - 0.96], p = 0.032). For CD patients, they had higher odds of steroid use (aOR = 1.13, 95% CI = [1.03 - 1.25], p = 0.009), and perianal abscess (aOR = 1.12, 95% CI = [1.10 - 1.36], p = 0.001). CD smokers recorded lower odds of all-cause mortality (aOR = 0.51, 95% CI = [0.27 - 0.98], p = 0.04). All other outcomes were non-statistically significant between the study cohorts.
Discussion: Smoking in hospitalized UC patients was associated with lower steroid use, while in CD patients, it correlated with higher steroid use and increased odds of perianal abscess. These findings highlight the complex impact of smoking on IBD outcomes, warranting further investigation into its clinical implications.
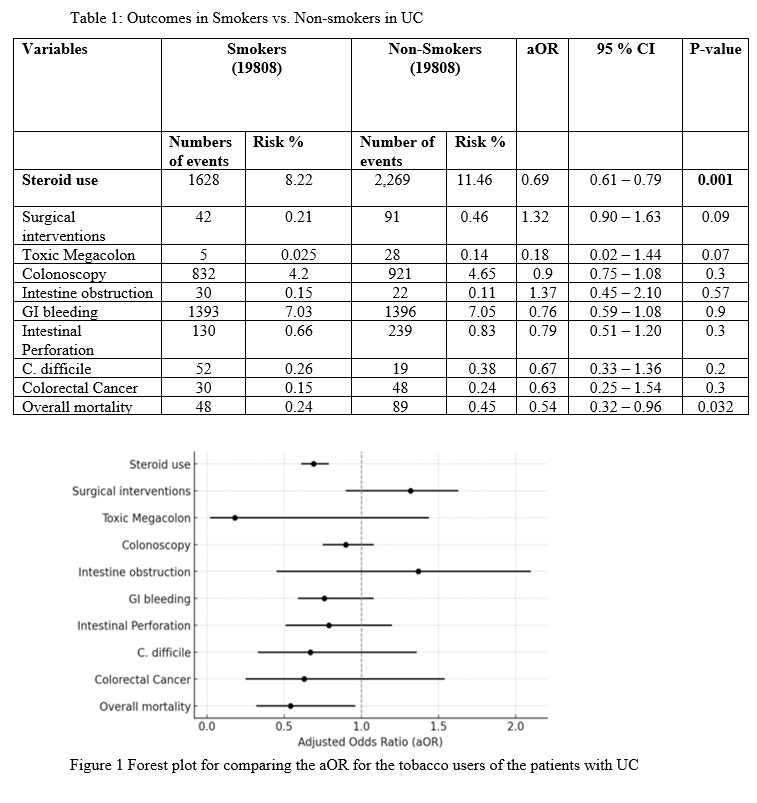
Figure: Outcomes in patients with UC (smokers vs non-smokers)
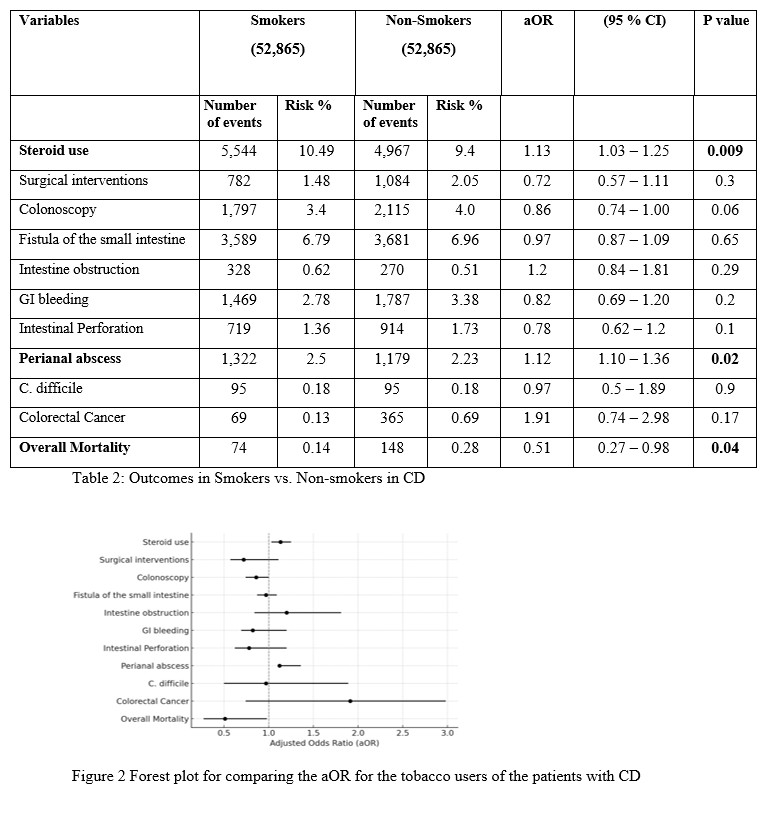
Figure: Outcomes in patients with CD (smokers vs non-smokers)
Disclosures:
Mohamed Eldesouki indicated no relevant financial relationships.
Mohammad Kloub indicated no relevant financial relationships.
Abdulrahman Abusalim indicated no relevant financial relationships.
Khaled Elfert indicated no relevant financial relationships.
Mohammed Y. Youssef indicated no relevant financial relationships.
Mohammad Nabil Rayad indicated no relevant financial relationships.
Yashwita Sai Pulakurthi indicated no relevant financial relationships.
Kanwarpreet Tandon indicated no relevant financial relationships.
Mohamed Eldesouki, MD1, Mohammad Kloub, MD2, Abdulrahman Abusalim, MD3, Khaled Elfert, MBChB, MRCP4, Mohammed Y. Youssef, MD5, Mohammad Nabil Rayad, MD6, Yashwita Sai Pulakurthi, MD7, Kanwarpreet Tandon, MBBS4. P1077 - Impact of Tobacco Use in Patients With Inflammatory Bowel Disease: Nationwide Propensity-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
