Sunday Poster Session
Category: IBD
P1072 - Burden and Outcomes of Opportunistic Infections Among IBD Patients: Analysis of the 2022 National Inpatient Sample
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rafia Irfan Waheed, MD (she/her/hers)
University of South Dakota Sanford School of Medicine
Sioux Falls, SD
Presenting Author(s)
Rafia Irfan Waheed, MD1, Dawood Shehzad, MD1, Hareem Tahir, MD1, Gulzar Ahmed, MBBS2, Dawlat Khan, MD1
1University of South Dakota Sanford School of Medicine, Sioux Falls, SD; 2Dow Medical College, Karachi, Sindh, Pakistan
Introduction: Inflammatory Bowel Disease (IBD), including both Crohn’s Disease and Ulcerative Colitis, is frequently treated with immunosuppressive therapies to control disease activity. While these treatments are effective, they also increase patients’ vulnerability to opportunistic infections. This study aims to identify the incidence of opportunistic infections (OI) among IBD patients and determine the clinical outcomes including overall mortality.
Methods: The National Inpatient Sample (NIS) database was used to identify patients who had a discharge diagnosis of IBD and OI as a primary or secondary diagnosis via ICD-10 codes during the year 2022. The primary outcome was in-hospital mortality; secondary endpoints included length of stay (LOS) and total hospital charges. Linear and logistic regression analyses were performed to evaluate associations between OIs and clinical outcomes.
Results: 4,366 individuals were found to have both IBD and at least one OI. The mean age was higher in IBD with OI,56.5(95% CI: 55.7- 57.3), compared to those without OI, 54.6(95% CI: 54.22- 55.03) .Females had a higher proportion of OI(59.5%) compared to males(40.5%), with a p value < 0. 001. Racial distribution varied significantly by OI status, p< 0.001, with white being in the majority in both groups. The most common OI observed was C. difficile, followed by Candida, as outlined in Figure 1 . The in-hospital mortality was double among these patients with an odds ratio(OR) of 2.39 (95% CI: 2.06–2.78). Additionally, these patients experienced a significantly longer length of stay(LOS) with an OR 4.68 (95% CI: 4.29–5.07), and substantially higher total hospital charges (TOTCHG), averaging $49,531.59 (95% CI: $42,142.74–$56,920.45), both with p-values < 0.0001. The most common adverse outcome was ARDS with an OR of 3.57(95% CI: 2.49- 5.122), followed by sepsis with an OR of 2.66(95% CI: 2.46- 2.89) (Figure 2).
Discussion: This study demonstrated that OIs in individuals with IBD were associated with higher in-hospital mortality, longer hospital stays, and significantly increased healthcare costs. Women above the age of 50 and the white population had a higher prevalence. C. difficile and Candida were the most common OIs. Adverse outcomes such as ARDS and sepsis were notably more frequent among patients with OIs. This highlights the need for a screening protocol to identify the high-risk population early, ensure that patients are up to date with their vaccinations, and use prophylactic antimicrobials when indicated.
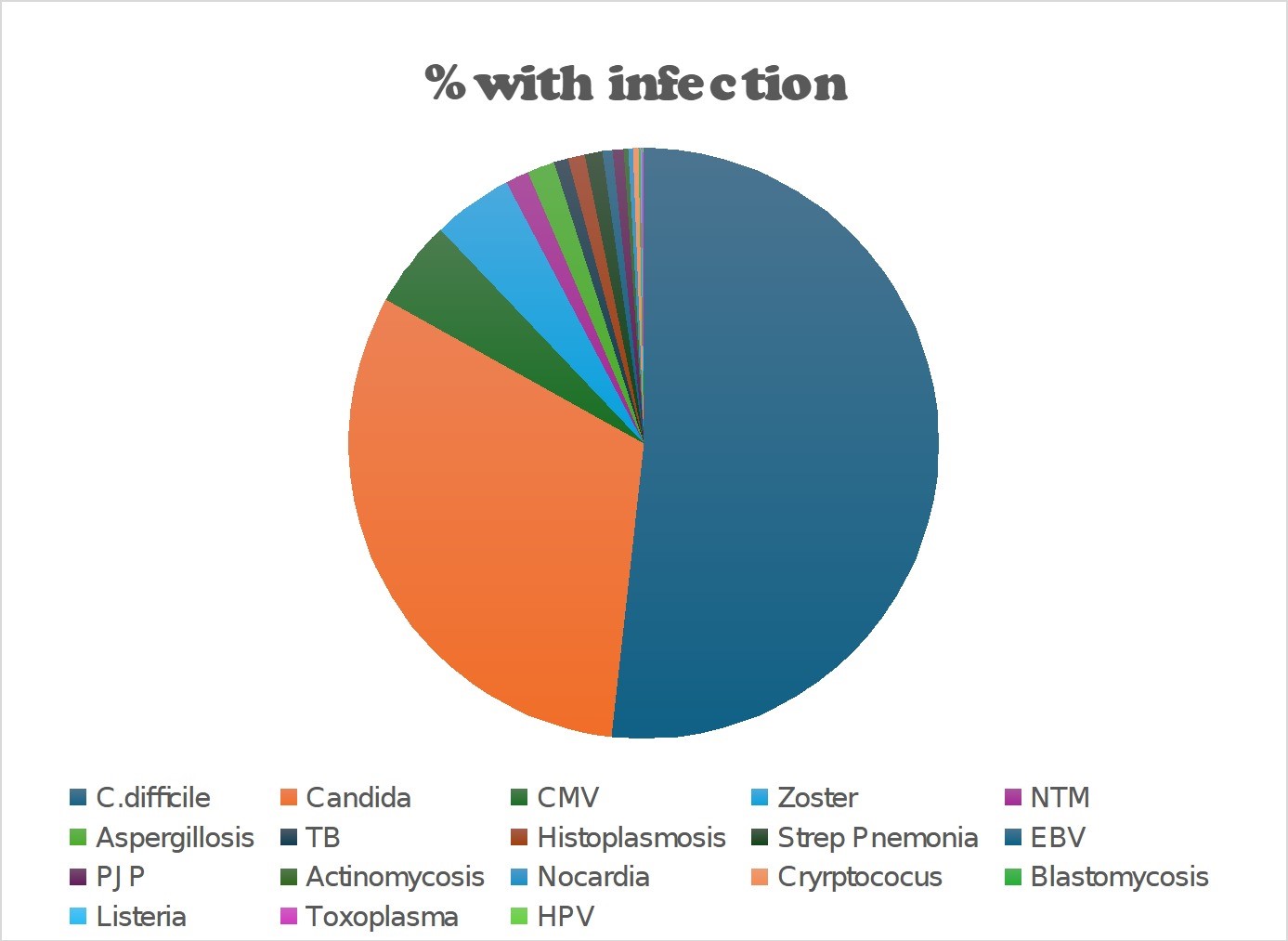
Figure: Figure 1:Pie chart showing % infection
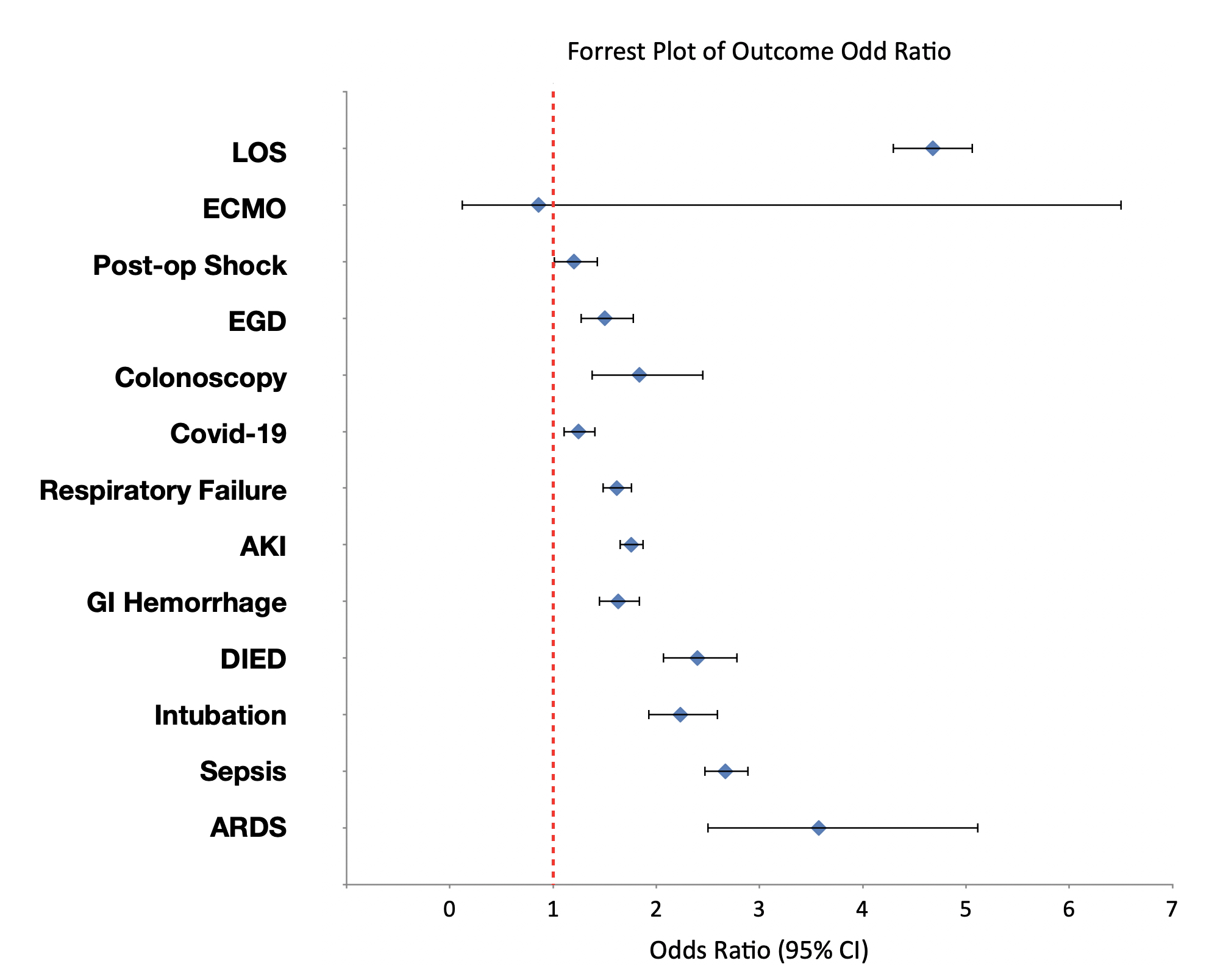
Figure: Figure 2: Forest plot of Outcomes Odd Ratio
Disclosures:
Rafia Irfan Waheed indicated no relevant financial relationships.
Dawood Shehzad indicated no relevant financial relationships.
Hareem Tahir indicated no relevant financial relationships.
Gulzar Ahmed indicated no relevant financial relationships.
Dawlat Khan indicated no relevant financial relationships.
Rafia Irfan Waheed, MD1, Dawood Shehzad, MD1, Hareem Tahir, MD1, Gulzar Ahmed, MBBS2, Dawlat Khan, MD1. P1072 - Burden and Outcomes of Opportunistic Infections Among IBD Patients: Analysis of the 2022 National Inpatient Sample, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of South Dakota Sanford School of Medicine, Sioux Falls, SD; 2Dow Medical College, Karachi, Sindh, Pakistan
Introduction: Inflammatory Bowel Disease (IBD), including both Crohn’s Disease and Ulcerative Colitis, is frequently treated with immunosuppressive therapies to control disease activity. While these treatments are effective, they also increase patients’ vulnerability to opportunistic infections. This study aims to identify the incidence of opportunistic infections (OI) among IBD patients and determine the clinical outcomes including overall mortality.
Methods: The National Inpatient Sample (NIS) database was used to identify patients who had a discharge diagnosis of IBD and OI as a primary or secondary diagnosis via ICD-10 codes during the year 2022. The primary outcome was in-hospital mortality; secondary endpoints included length of stay (LOS) and total hospital charges. Linear and logistic regression analyses were performed to evaluate associations between OIs and clinical outcomes.
Results: 4,366 individuals were found to have both IBD and at least one OI. The mean age was higher in IBD with OI,56.5(95% CI: 55.7- 57.3), compared to those without OI, 54.6(95% CI: 54.22- 55.03) .Females had a higher proportion of OI(59.5%) compared to males(40.5%), with a p value < 0. 001. Racial distribution varied significantly by OI status, p< 0.001, with white being in the majority in both groups. The most common OI observed was C. difficile, followed by Candida, as outlined in Figure 1 . The in-hospital mortality was double among these patients with an odds ratio(OR) of 2.39 (95% CI: 2.06–2.78). Additionally, these patients experienced a significantly longer length of stay(LOS) with an OR 4.68 (95% CI: 4.29–5.07), and substantially higher total hospital charges (TOTCHG), averaging $49,531.59 (95% CI: $42,142.74–$56,920.45), both with p-values < 0.0001. The most common adverse outcome was ARDS with an OR of 3.57(95% CI: 2.49- 5.122), followed by sepsis with an OR of 2.66(95% CI: 2.46- 2.89) (Figure 2).
Discussion: This study demonstrated that OIs in individuals with IBD were associated with higher in-hospital mortality, longer hospital stays, and significantly increased healthcare costs. Women above the age of 50 and the white population had a higher prevalence. C. difficile and Candida were the most common OIs. Adverse outcomes such as ARDS and sepsis were notably more frequent among patients with OIs. This highlights the need for a screening protocol to identify the high-risk population early, ensure that patients are up to date with their vaccinations, and use prophylactic antimicrobials when indicated.
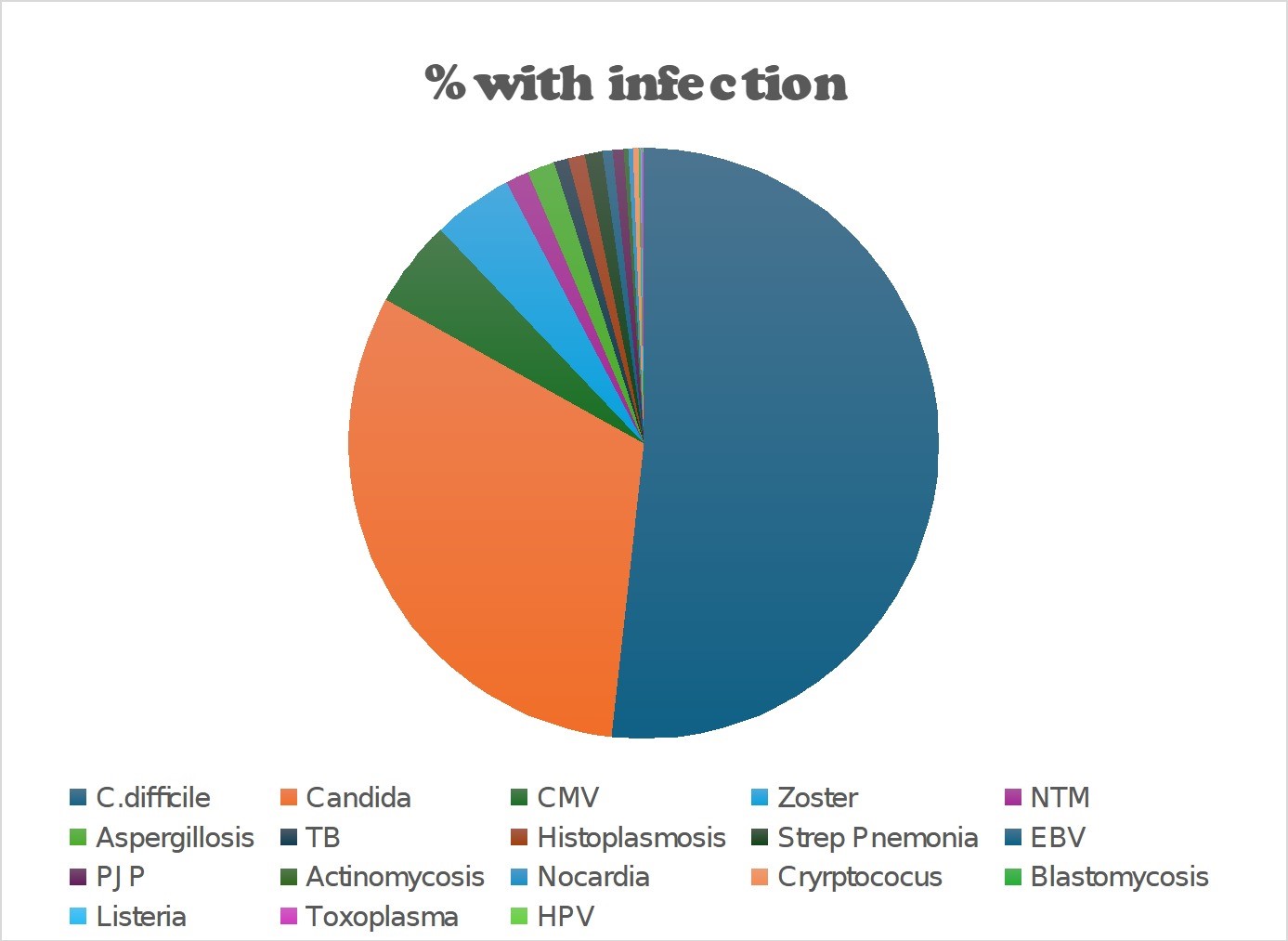
Figure: Figure 1:Pie chart showing % infection
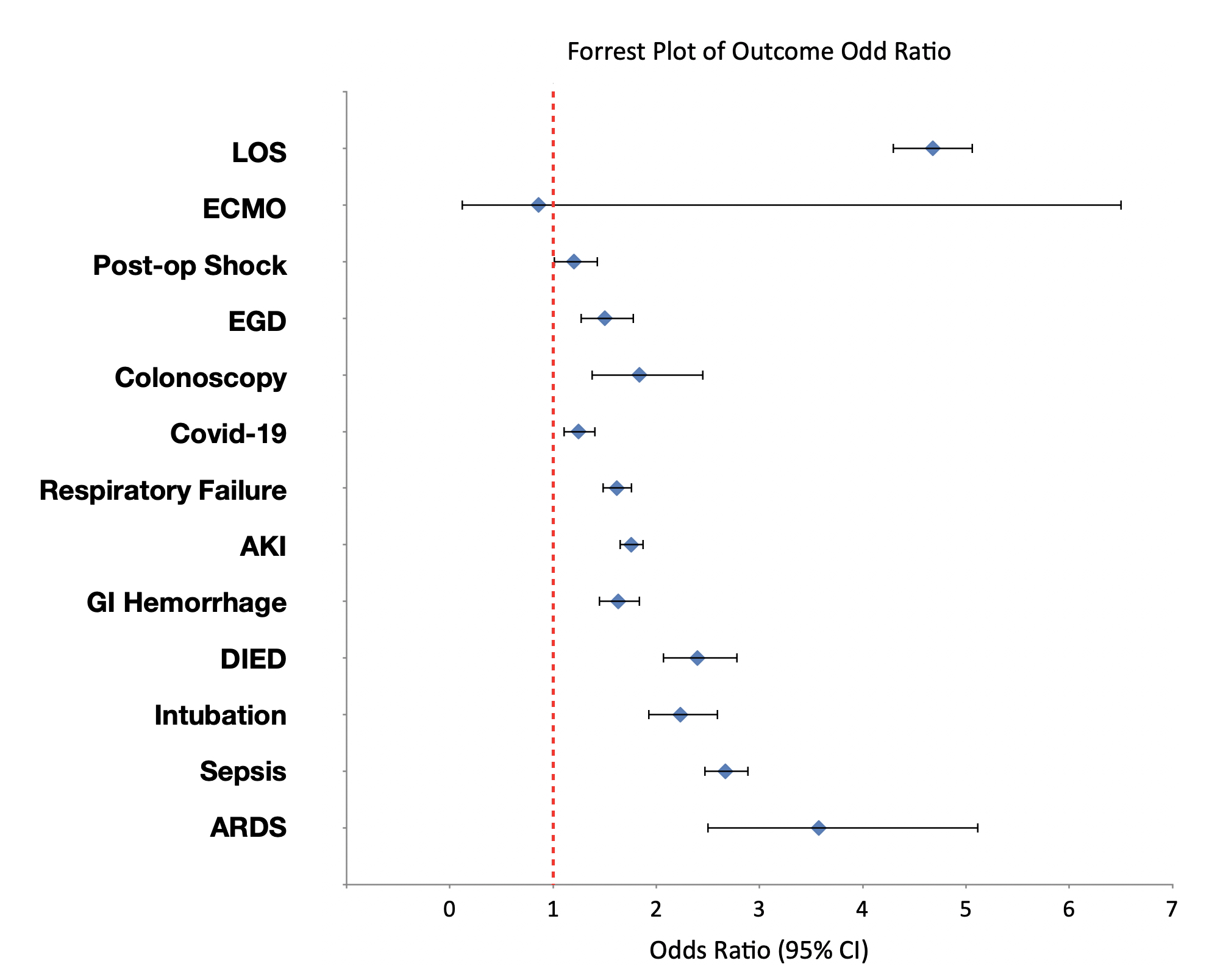
Figure: Figure 2: Forest plot of Outcomes Odd Ratio
Disclosures:
Rafia Irfan Waheed indicated no relevant financial relationships.
Dawood Shehzad indicated no relevant financial relationships.
Hareem Tahir indicated no relevant financial relationships.
Gulzar Ahmed indicated no relevant financial relationships.
Dawlat Khan indicated no relevant financial relationships.
Rafia Irfan Waheed, MD1, Dawood Shehzad, MD1, Hareem Tahir, MD1, Gulzar Ahmed, MBBS2, Dawlat Khan, MD1. P1072 - Burden and Outcomes of Opportunistic Infections Among IBD Patients: Analysis of the 2022 National Inpatient Sample, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
