Sunday Poster Session
Category: IBD
P1053 - Trends, Burden and Impact of Infections on Outcomes in Patients With Ulcerative Colitis: A Nationwide Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- CS
Carol Singh, MBBS
Dayanand Medical College and Hospital
New Jersey, NJ
Presenting Author(s)
Tanisha Sehgal, MBBS1, Nishma Dhand, MBBS2, Carol Singh, MBBS3, Sampada Bhasker, MBBS4, Anmol Singh, MBBS5, Vikash Kumar, MD6, Aalam Sohal, MD6, Dalbir Sandhu, MD6
1Dayanand Medical College and Hospital, Singapore, Singapore; 2Dayanand Medical College and Hospital, Moga, Punjab, India; 3Dayanand Medical College and Hospital, New Jersey, NJ; 4Punjab Institute of Medical Sciences, Jalandhar, Punjab, India; 5Tristar Centennial Medical Center, Nashville, TN, Nashville, TN; 6Creighton University School of Medicine, Phoenix, AZ
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease characterized by mucosal inflammation in the colon. Patients with UC are predisposed to infections due to underlying immune dysfunction and immunosuppressive therapy. This study investigates recent trends, burden, and the clinical impact of infections among hospitalized UC patients.
Methods: The National Inpatient Sample database 2016-2022 was used to identify adult patients with UC. Patients were stratified into two groups—those with and without infections. We collected data on patient demographics, comorbidities, types of infections, and clinical outcomes. The study outcomes included in-hospital mortality, sepsis, shock, acute kidney injury (AKI), intensive care unit (ICU) stay, blood transfusions, and surgical procedures. A multivariate logistic/linear regression analysis was used to assess the impact of infections on these outcomes.
Results: Among the 826,945 patients diagnosed with UC, 216,595 (26.2%) developed infections. The most frequent infections observed include UTI (9.2%), hospital-acquired pneumonia (HAP) (7.0%), and Clostridioides difficile infection (CDI) (6.2%). From 2016-2022, rising trends were noted in HAP, cholangitis and bacteremia, while the trends among UTI remained stable (Figure 1.). Infections were associated with significantly worse clinical outcomes, including in-hospital mortality (4.9% vs. 1.3%), sepsis (5.9% vs 2.7%), AKI (28.5% vs. 14.8%), shock (9.2% vs 2.6%), ICU admissions (7.0% vs. 2.3%), blood transfusions (0.7% vs 0.3%), but decreased rates of surgical procedures (2.6% vs. 4.9%). After adjusting for confounding factors, patients with infections had higher odds of in-hospital mortality (aOR-2.87, 95% CI-2.68-3.08,p < 0.001), sepsis (aOR-2.24, 95% CI- 2.12-2.37, p< 0.001), AKI (aOR-1.84, 95% CI- 1.78-1.89, p< 0.001), shock (aOR-3.18, 95% CI-3.02-3.35, p< 0.001), ICU admissions (aOR-2.74, 95% CI-2.60-2.93, p< 0.001), blood transfusions (aOR-1.98, 95% CI-1.68-2.32, p< 0.001), but decreased odds of surgical procedures (aOR-0.68, 95% CI-0.63-0.73, p< 0.001) (Table 1).
Discussion: Our study reveals that infections significantly worsen clinical outcomes and increase healthcare utilization in UC patients. Therefore, prevention, early identification and management of infections are critical in improving patient prognosis.
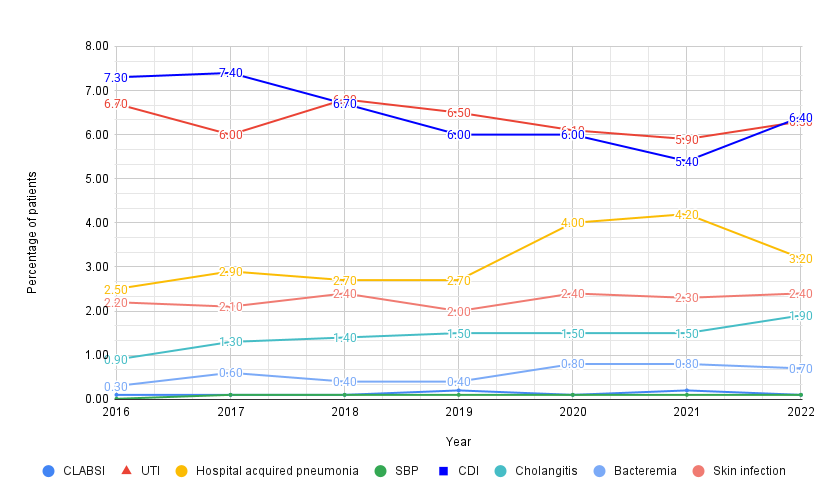
Figure: Figure 1. Trends of Infections in Ulcerative colitis between 2016-2022

Figure: Table 1. Results of multivariate logistic regression, assessing the impact of infections on outcomes and resource utilization.
Disclosures:
Tanisha Sehgal indicated no relevant financial relationships.
Nishma Dhand indicated no relevant financial relationships.
Carol Singh indicated no relevant financial relationships.
Sampada Bhasker indicated no relevant financial relationships.
Anmol Singh indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Tanisha Sehgal, MBBS1, Nishma Dhand, MBBS2, Carol Singh, MBBS3, Sampada Bhasker, MBBS4, Anmol Singh, MBBS5, Vikash Kumar, MD6, Aalam Sohal, MD6, Dalbir Sandhu, MD6. P1053 - Trends, Burden and Impact of Infections on Outcomes in Patients With Ulcerative Colitis: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Dayanand Medical College and Hospital, Singapore, Singapore; 2Dayanand Medical College and Hospital, Moga, Punjab, India; 3Dayanand Medical College and Hospital, New Jersey, NJ; 4Punjab Institute of Medical Sciences, Jalandhar, Punjab, India; 5Tristar Centennial Medical Center, Nashville, TN, Nashville, TN; 6Creighton University School of Medicine, Phoenix, AZ
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease characterized by mucosal inflammation in the colon. Patients with UC are predisposed to infections due to underlying immune dysfunction and immunosuppressive therapy. This study investigates recent trends, burden, and the clinical impact of infections among hospitalized UC patients.
Methods: The National Inpatient Sample database 2016-2022 was used to identify adult patients with UC. Patients were stratified into two groups—those with and without infections. We collected data on patient demographics, comorbidities, types of infections, and clinical outcomes. The study outcomes included in-hospital mortality, sepsis, shock, acute kidney injury (AKI), intensive care unit (ICU) stay, blood transfusions, and surgical procedures. A multivariate logistic/linear regression analysis was used to assess the impact of infections on these outcomes.
Results: Among the 826,945 patients diagnosed with UC, 216,595 (26.2%) developed infections. The most frequent infections observed include UTI (9.2%), hospital-acquired pneumonia (HAP) (7.0%), and Clostridioides difficile infection (CDI) (6.2%). From 2016-2022, rising trends were noted in HAP, cholangitis and bacteremia, while the trends among UTI remained stable (Figure 1.). Infections were associated with significantly worse clinical outcomes, including in-hospital mortality (4.9% vs. 1.3%), sepsis (5.9% vs 2.7%), AKI (28.5% vs. 14.8%), shock (9.2% vs 2.6%), ICU admissions (7.0% vs. 2.3%), blood transfusions (0.7% vs 0.3%), but decreased rates of surgical procedures (2.6% vs. 4.9%). After adjusting for confounding factors, patients with infections had higher odds of in-hospital mortality (aOR-2.87, 95% CI-2.68-3.08,p < 0.001), sepsis (aOR-2.24, 95% CI- 2.12-2.37, p< 0.001), AKI (aOR-1.84, 95% CI- 1.78-1.89, p< 0.001), shock (aOR-3.18, 95% CI-3.02-3.35, p< 0.001), ICU admissions (aOR-2.74, 95% CI-2.60-2.93, p< 0.001), blood transfusions (aOR-1.98, 95% CI-1.68-2.32, p< 0.001), but decreased odds of surgical procedures (aOR-0.68, 95% CI-0.63-0.73, p< 0.001) (Table 1).
Discussion: Our study reveals that infections significantly worsen clinical outcomes and increase healthcare utilization in UC patients. Therefore, prevention, early identification and management of infections are critical in improving patient prognosis.
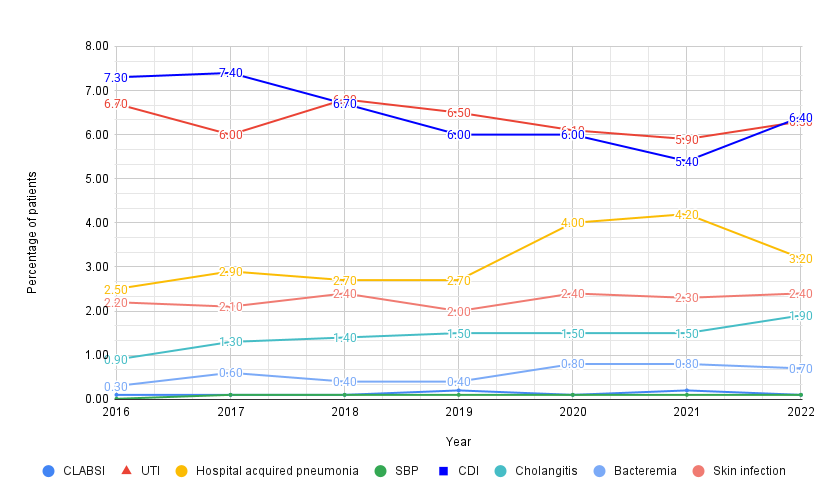
Figure: Figure 1. Trends of Infections in Ulcerative colitis between 2016-2022

Figure: Table 1. Results of multivariate logistic regression, assessing the impact of infections on outcomes and resource utilization.
Disclosures:
Tanisha Sehgal indicated no relevant financial relationships.
Nishma Dhand indicated no relevant financial relationships.
Carol Singh indicated no relevant financial relationships.
Sampada Bhasker indicated no relevant financial relationships.
Anmol Singh indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Tanisha Sehgal, MBBS1, Nishma Dhand, MBBS2, Carol Singh, MBBS3, Sampada Bhasker, MBBS4, Anmol Singh, MBBS5, Vikash Kumar, MD6, Aalam Sohal, MD6, Dalbir Sandhu, MD6. P1053 - Trends, Burden and Impact of Infections on Outcomes in Patients With Ulcerative Colitis: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
