Sunday Poster Session
Category: GI Bleeding
P1017 - A Case of Gastrointestinal Bleeding Caused by Brunner's Gland Hamartoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Laura DiBenedetto, DO
New York University Langone Health
Astoria, NY
Presenting Author(s)
Laura DiBenedetto, DO1, Vincent Wong, MD2, Nathan Starkman, MD3, Naunihal Singh, DO4, Stephanie Ren, MD5, David Friedel, MD5, Mansoor Nasim, MD, PhD6
1New York University Langone Health, Astoria, NY; 2New York University Langone Health, Mineola, NY; 3NYU Grossman School of Medicine, Mineola, NY; 4New York University Langone Health, West Hempstead, NY; 5NYU Langone Health, Mineola, NY; 6New York University Langone Health, Patchogue, NY
Introduction: Brunner’s gland hamartomas are uncommon benign duodenal tumors. They make up less than 1% of tumors in the small intestine and have a low risk of progression to adenocarcinoma. While most patients are asymptomatic, patients with larger polyps tend to have symptoms such as gastrointestinal bleeding from superficial erosions and ulceration, or obstruction. In this case, we describe a patient with an upper gastrointestinal bleed from a pedunculated duodenal hamartoma.
Case Description/
Methods: A 67-year-old male with history of Barrett’s Esophagus, coronary artery disease, diverticulosis with prior sigmoid colectomy, hypertension, and gastroesophageal reflux disease presented from an outpatient hematologist for two days of melena, dizziness. He had a hemoglobin of 9.8 from his baseline of 14.4 g/dL. As part of a recent iron deficiency anemia workup, he had an upper endoscopy, video capsule endoscopy and colonoscopy that did not identify a source of blood loss. He underwent enteroscopy which revealed a 25 mm pedunculated polyp extending from the duodenal bulb with a 5 cm stalk. Two endoloops, epinephrine and a hot snare were used for removal followed by closure with two hemostatic clips. CT enterography was negative. Pathology revealed a duodenal hamartoma with mucosal lining showing reactive changes, mild chronic duodenitis and gastric foveolar metaplasia. A month later, the patient reported no additional episodes of melena and his hemoglobin improved to 13.1.
Discussion: Duodenal hamartomas are benign lesions that can arise from Brunner’s glands. Their sizes usually range from approximately 1 to 5 cm, with bleeding commonly occurring in lesions larger than 3 cm. Brunner’s gland hamartomas should be considered in the differential for a duodenal mass; although many are benign, there have been few reports of malignancy arising from them. Therefore, these lesions should be endoscopically resected if they are found due to the risk of bleeding.
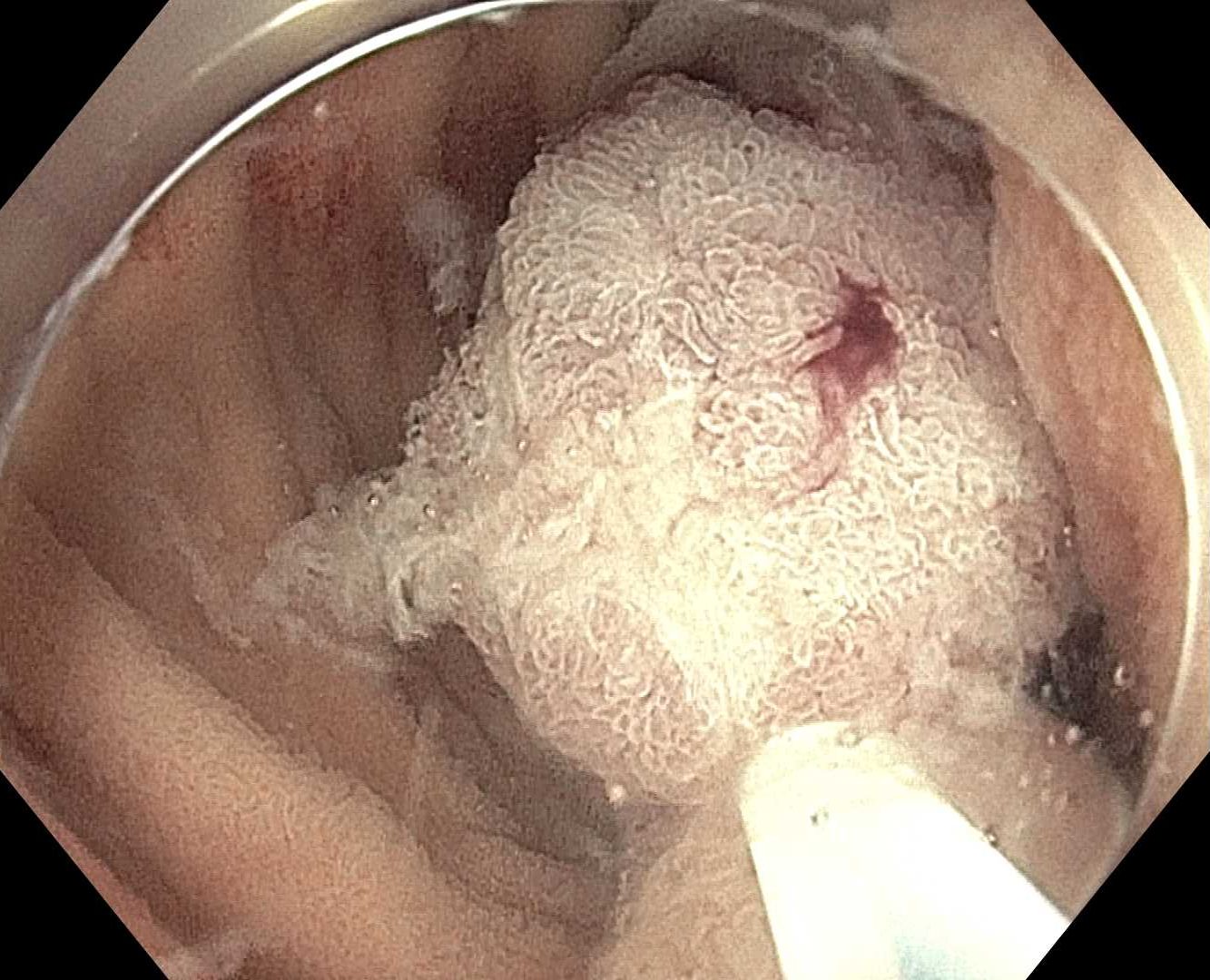
Figure: 2.5 cm pedunculated polyp seen endoscopically in the duodenal bulb

Figure: High magnification shows lobulated proliferations of Brunner’s gland with glandular epithelium composed of uniform, mucin-secreting columnar cells without cytologic atypia or mitotic activity.
Disclosures:
Laura DiBenedetto indicated no relevant financial relationships.
Vincent Wong indicated no relevant financial relationships.
Nathan Starkman indicated no relevant financial relationships.
Naunihal Singh indicated no relevant financial relationships.
Stephanie Ren indicated no relevant financial relationships.
David Friedel indicated no relevant financial relationships.
Mansoor Nasim indicated no relevant financial relationships.
Laura DiBenedetto, DO1, Vincent Wong, MD2, Nathan Starkman, MD3, Naunihal Singh, DO4, Stephanie Ren, MD5, David Friedel, MD5, Mansoor Nasim, MD, PhD6. P1017 - A Case of Gastrointestinal Bleeding Caused by Brunner's Gland Hamartoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1New York University Langone Health, Astoria, NY; 2New York University Langone Health, Mineola, NY; 3NYU Grossman School of Medicine, Mineola, NY; 4New York University Langone Health, West Hempstead, NY; 5NYU Langone Health, Mineola, NY; 6New York University Langone Health, Patchogue, NY
Introduction: Brunner’s gland hamartomas are uncommon benign duodenal tumors. They make up less than 1% of tumors in the small intestine and have a low risk of progression to adenocarcinoma. While most patients are asymptomatic, patients with larger polyps tend to have symptoms such as gastrointestinal bleeding from superficial erosions and ulceration, or obstruction. In this case, we describe a patient with an upper gastrointestinal bleed from a pedunculated duodenal hamartoma.
Case Description/
Methods: A 67-year-old male with history of Barrett’s Esophagus, coronary artery disease, diverticulosis with prior sigmoid colectomy, hypertension, and gastroesophageal reflux disease presented from an outpatient hematologist for two days of melena, dizziness. He had a hemoglobin of 9.8 from his baseline of 14.4 g/dL. As part of a recent iron deficiency anemia workup, he had an upper endoscopy, video capsule endoscopy and colonoscopy that did not identify a source of blood loss. He underwent enteroscopy which revealed a 25 mm pedunculated polyp extending from the duodenal bulb with a 5 cm stalk. Two endoloops, epinephrine and a hot snare were used for removal followed by closure with two hemostatic clips. CT enterography was negative. Pathology revealed a duodenal hamartoma with mucosal lining showing reactive changes, mild chronic duodenitis and gastric foveolar metaplasia. A month later, the patient reported no additional episodes of melena and his hemoglobin improved to 13.1.
Discussion: Duodenal hamartomas are benign lesions that can arise from Brunner’s glands. Their sizes usually range from approximately 1 to 5 cm, with bleeding commonly occurring in lesions larger than 3 cm. Brunner’s gland hamartomas should be considered in the differential for a duodenal mass; although many are benign, there have been few reports of malignancy arising from them. Therefore, these lesions should be endoscopically resected if they are found due to the risk of bleeding.
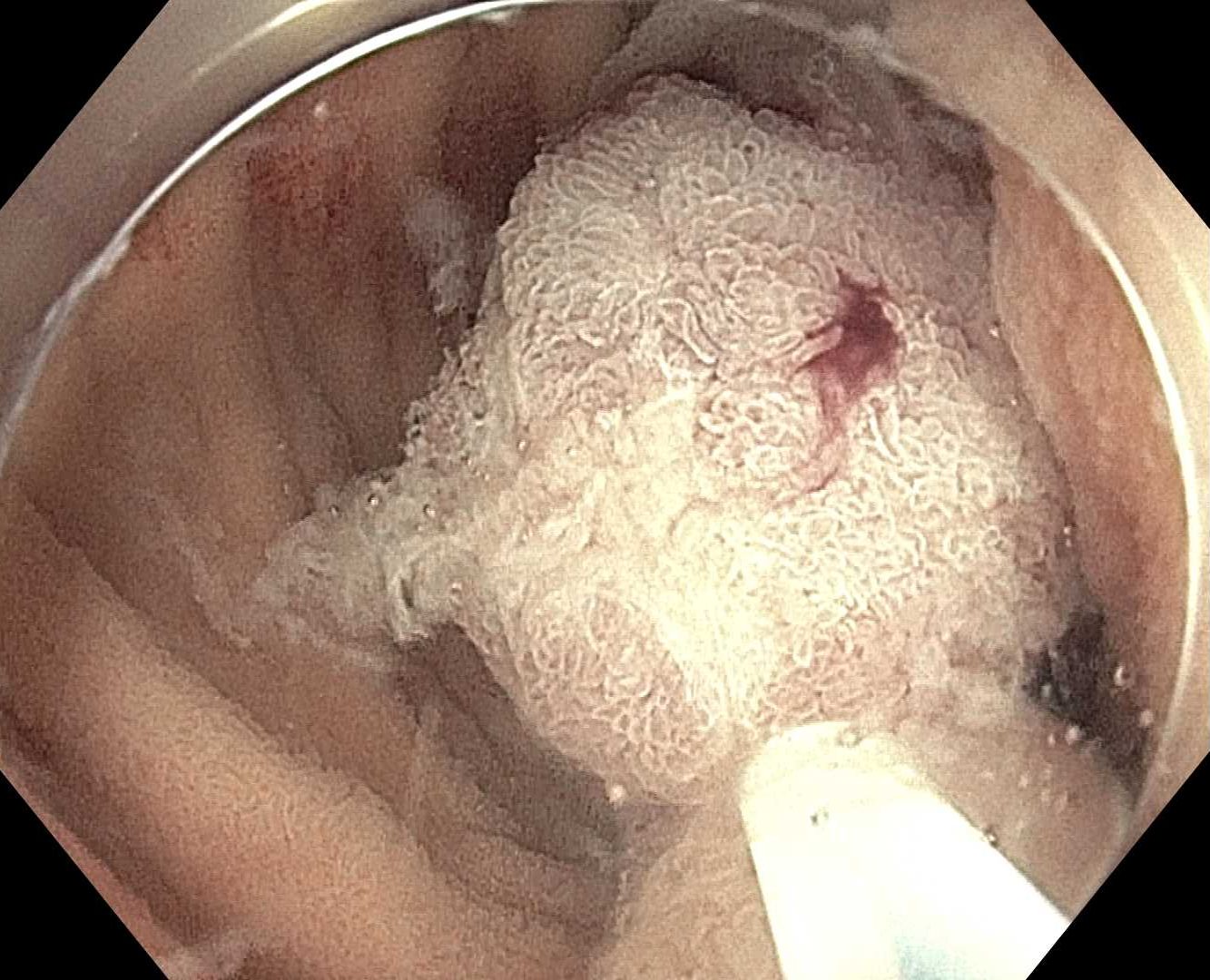
Figure: 2.5 cm pedunculated polyp seen endoscopically in the duodenal bulb

Figure: High magnification shows lobulated proliferations of Brunner’s gland with glandular epithelium composed of uniform, mucin-secreting columnar cells without cytologic atypia or mitotic activity.
Disclosures:
Laura DiBenedetto indicated no relevant financial relationships.
Vincent Wong indicated no relevant financial relationships.
Nathan Starkman indicated no relevant financial relationships.
Naunihal Singh indicated no relevant financial relationships.
Stephanie Ren indicated no relevant financial relationships.
David Friedel indicated no relevant financial relationships.
Mansoor Nasim indicated no relevant financial relationships.
Laura DiBenedetto, DO1, Vincent Wong, MD2, Nathan Starkman, MD3, Naunihal Singh, DO4, Stephanie Ren, MD5, David Friedel, MD5, Mansoor Nasim, MD, PhD6. P1017 - A Case of Gastrointestinal Bleeding Caused by Brunner's Gland Hamartoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
