Sunday Poster Session
Category: GI Bleeding
P1003 - Coil Migration into Duodenum: Uncommon Cause of Recurrent Gastrointestinal Bleeding
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Amy Man, MD (she/her/hers)
University of Tennessee Health Science Center
Memphis, TN
Presenting Author(s)
Amy Man, MD1, Akhil Adla, DO1, Shanthan Ramidi, MD2, Leonard Baidoo, MD, FACG1, Muhammad Siddiq, MD1, Jiten Kothadia, MD1
1University of Tennessee Health Science Center, Memphis, TN; 2Atrium Health, Concord, NC
Introduction: Endoscopic hemostatic intervention is the first-line treatment for upper gastrointestinal (GI) bleeding, but patients often require transarterial angiographic embolization (TAE) for refractory bleeding. TAE has high success rates; however, it is important to acknowledge its complications such as bowel perforation, recurrent bleeding, vessel perforation, ischemia, and rarely, coil migration. Coil migration has been noted to occur in up to 3% of all cases that undergo TAE for GI bleeding [1, 2]. Timely recognition and coordination of interventions are critical to improving outcomes. We present a case of recurrent bleeding duodenal ulcer secondary to a TAE coil migration through the duodenal wall.
Case Description/
Methods: A 76-year-old man with a history of hypertension, chronic kidney disease, and right femur fracture status post repair presented with complaints of right leg pain and was found to have a dehiscence of his right leg wound. He was incidentally found to have a subacute pulmonary embolism. After initiation of heparin, he developed melena and became hemodynamically unstable requiring vasopressor support. Imaging revealed a duodenal ulcer, and extravasation from the gastroduodenal artery (GA) prompting emergent angiography. A moderate size pseudoaneurysm in the GA was noted and he underwent successful coil embolization. After stabilization, he underwent debridement of his right femur, and an IVC filter was placed instead of anticoagulation. The patient again began to experience melena with decreasing hemoglobin despite multiple transfusions. Given persistent melena and needing frequent blood transfusions, the patient underwent esophagogastroduodenoscopy that showed a 4cm duodenal bulb ulcer with a clean ulcer base (Forrest Class III) with surrounding erythema. Multiple loops of coil from recent TAE were seen protruding adjacent to the clean-based ulcer from the duodenal wall (Figure A, B). After transfer to the ICU, general surgery was consulted for urgent surgical evaluation. Unfortunately, due to extensive comorbidities, the patient was not deemed as a surgical candidate, subsequently was switched to comfort care, and passed away shortly thereafter.
Discussion: Coil migration is an uncommon serious complication after TAE. A retrospective case review of 10 cases showed multidisciplinary management is key and often requires surgical intervention. Although rare, Coil migration should be considered in differential in patients presenting with recurrent upper GI bleeding despite TAE.
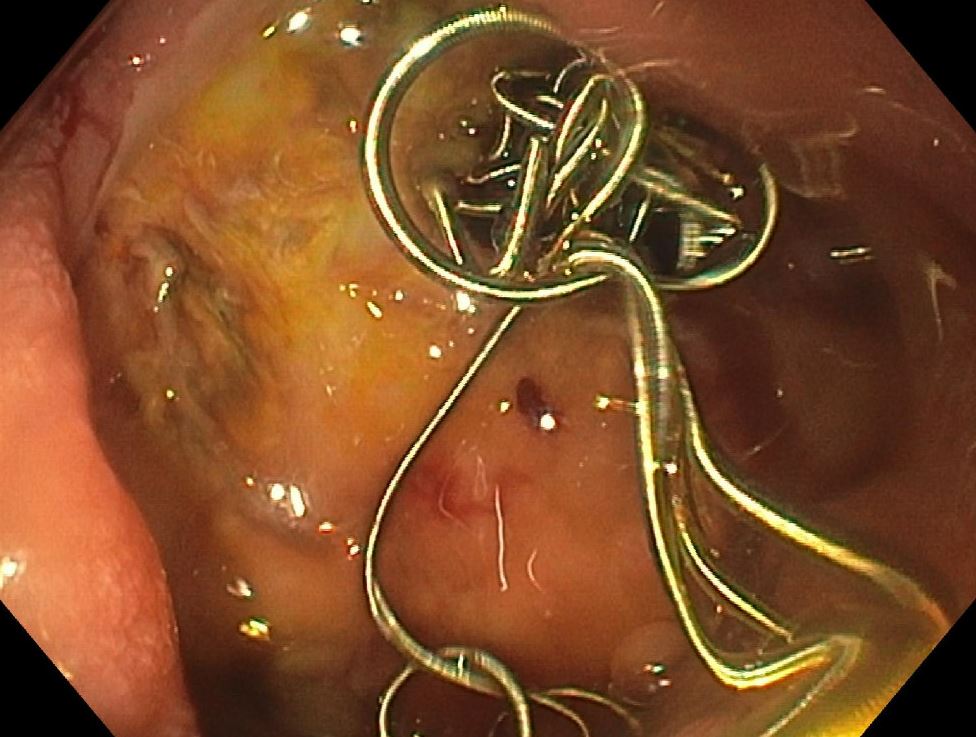
Figure: Figure A: Figure A shows coil exiting out of the duodenal ulcer into the duodenum.

Figure: Figure B: Coil further migrated into the intestine.
Disclosures:
Amy Man indicated no relevant financial relationships.
Akhil Adla indicated no relevant financial relationships.
Shanthan Ramidi indicated no relevant financial relationships.
Leonard Baidoo: Johnson and Johnson – Speakers Bureau. Lily Pharmaceuticals – Speakers Bureau. Pfizer – Speakers Bureau.
Muhammad Siddiq indicated no relevant financial relationships.
Jiten Kothadia indicated no relevant financial relationships.
Amy Man, MD1, Akhil Adla, DO1, Shanthan Ramidi, MD2, Leonard Baidoo, MD, FACG1, Muhammad Siddiq, MD1, Jiten Kothadia, MD1. P1003 - Coil Migration into Duodenum: Uncommon Cause of Recurrent Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Tennessee Health Science Center, Memphis, TN; 2Atrium Health, Concord, NC
Introduction: Endoscopic hemostatic intervention is the first-line treatment for upper gastrointestinal (GI) bleeding, but patients often require transarterial angiographic embolization (TAE) for refractory bleeding. TAE has high success rates; however, it is important to acknowledge its complications such as bowel perforation, recurrent bleeding, vessel perforation, ischemia, and rarely, coil migration. Coil migration has been noted to occur in up to 3% of all cases that undergo TAE for GI bleeding [1, 2]. Timely recognition and coordination of interventions are critical to improving outcomes. We present a case of recurrent bleeding duodenal ulcer secondary to a TAE coil migration through the duodenal wall.
Case Description/
Methods: A 76-year-old man with a history of hypertension, chronic kidney disease, and right femur fracture status post repair presented with complaints of right leg pain and was found to have a dehiscence of his right leg wound. He was incidentally found to have a subacute pulmonary embolism. After initiation of heparin, he developed melena and became hemodynamically unstable requiring vasopressor support. Imaging revealed a duodenal ulcer, and extravasation from the gastroduodenal artery (GA) prompting emergent angiography. A moderate size pseudoaneurysm in the GA was noted and he underwent successful coil embolization. After stabilization, he underwent debridement of his right femur, and an IVC filter was placed instead of anticoagulation. The patient again began to experience melena with decreasing hemoglobin despite multiple transfusions. Given persistent melena and needing frequent blood transfusions, the patient underwent esophagogastroduodenoscopy that showed a 4cm duodenal bulb ulcer with a clean ulcer base (Forrest Class III) with surrounding erythema. Multiple loops of coil from recent TAE were seen protruding adjacent to the clean-based ulcer from the duodenal wall (Figure A, B). After transfer to the ICU, general surgery was consulted for urgent surgical evaluation. Unfortunately, due to extensive comorbidities, the patient was not deemed as a surgical candidate, subsequently was switched to comfort care, and passed away shortly thereafter.
Discussion: Coil migration is an uncommon serious complication after TAE. A retrospective case review of 10 cases showed multidisciplinary management is key and often requires surgical intervention. Although rare, Coil migration should be considered in differential in patients presenting with recurrent upper GI bleeding despite TAE.
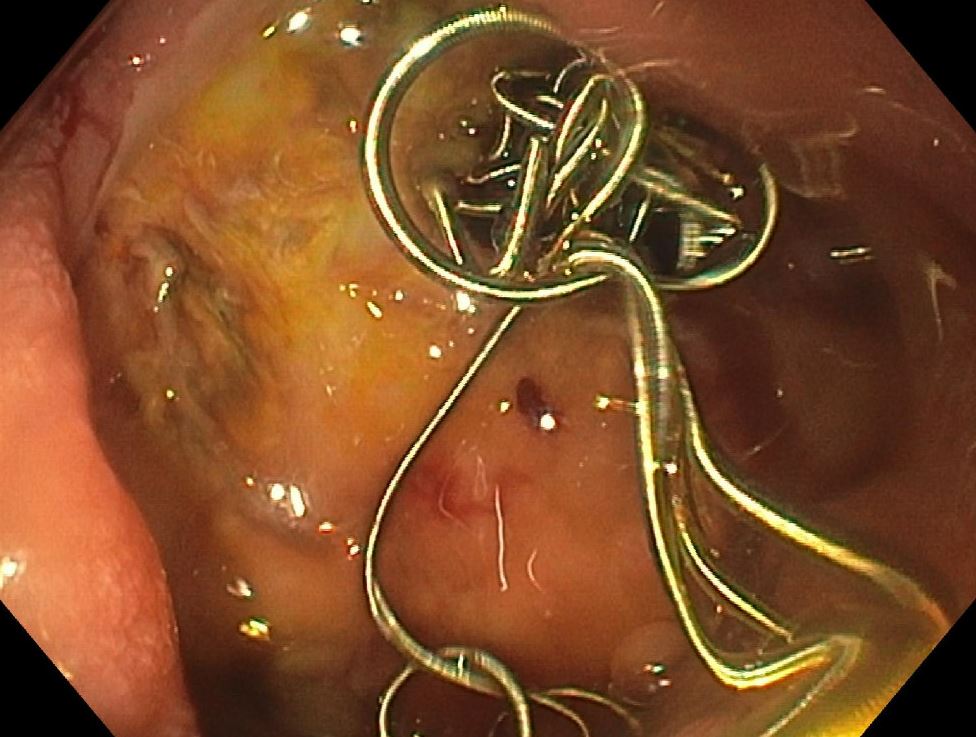
Figure: Figure A: Figure A shows coil exiting out of the duodenal ulcer into the duodenum.

Figure: Figure B: Coil further migrated into the intestine.
Disclosures:
Amy Man indicated no relevant financial relationships.
Akhil Adla indicated no relevant financial relationships.
Shanthan Ramidi indicated no relevant financial relationships.
Leonard Baidoo: Johnson and Johnson – Speakers Bureau. Lily Pharmaceuticals – Speakers Bureau. Pfizer – Speakers Bureau.
Muhammad Siddiq indicated no relevant financial relationships.
Jiten Kothadia indicated no relevant financial relationships.
Amy Man, MD1, Akhil Adla, DO1, Shanthan Ramidi, MD2, Leonard Baidoo, MD, FACG1, Muhammad Siddiq, MD1, Jiten Kothadia, MD1. P1003 - Coil Migration into Duodenum: Uncommon Cause of Recurrent Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
