Sunday Poster Session
Category: GI Bleeding
P0998 - The Colitis Enigma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Christina Kanagawa, DO
Cooper University Hospital
Cherry Hill, NJ
Presenting Author(s)
Christina Kanagawa, DO1, Yara Sarkis, MD2, Chelsea Edirisuriya, MD2, Joshua DeSipio, MD3, Krysta Contino, MD4
1Cooper University Hospital, Cherry Hill, NJ; 2Cooper University Hospital, Camden, NJ; 3Cooper Health Gastroenterology, Camden, NJ; 4Cooper Health Gastroenterology, Mount Laurel, NJ
Introduction: Rare conditions such as amyloidosis can present as colitis.
Case Description/
Methods: 73-year-old male with atrial fibrillation on apixaban and coronary artery disease presented with hematochezia and hypotension. Colonoscopy showed diffuse colitis with ulcerations and friability from rectosigmoid to transverse colon. There was initial concern for ischemic colitis. He was treated conservatively and discharged off apixaban with plan for repeat colonoscopy to assess healing and rule out inflammatory bowel disease (IBD). Patient was readmitted 2 weeks later for recurrent hematochezia. He informed us that he was just diagnosed with Multiple Myeloma (MM). Repeat colonoscopy showed persistent ulcerations without healing. Due to the recent diagnosis of MM, biopsies were sent for Congo Red stain as well as IBD. Pathology was positive for amyloidosis. To evaluate the extent of disease, endoscopy was done and revealed normal mucosa in stomach and duodenum with positive biopsies for amyloid. Video capsule endoscopy was also done and did not show small bowel (SB) abnormalities. Chemotherapy for MM was initiated with the goal of preventing further amyloid deposits in the gastrointestinal (GI) tract; however, it will not be curative. Unfortunately, he represented with similar symptoms 2 weeks later. Colorectal surgery evaluated him, and the decision was made to temporize bleeding with tranexamic acid as a bridge to allow for further chemotherapy and healing.
Discussion: Amyloidosis of the GI tract can have variable endoscopic findings. As evidenced in our patient, normal mucosa does not correlate with extent of disease, and endoscopic findings can mimic other pathologies, like IBD or ischemia. Diagnosis requires a high index of suspicion and special testing with Congo Red staining. There is no specific protocol to assess the extent of amyloid involvement, and it is unclear if deep enteroscopy for SB biopsy will change management. Moreover, there is no curative treatment for amyloidosis colitis as available therapies focus on underlying etiologies to prevent further deposits. Chemotherapy agents used to treat MM can be toxic to the colon and can worsen GI bleeding. Further studies are needed to implement a standardized protocol for diagnosis and management of this disease.
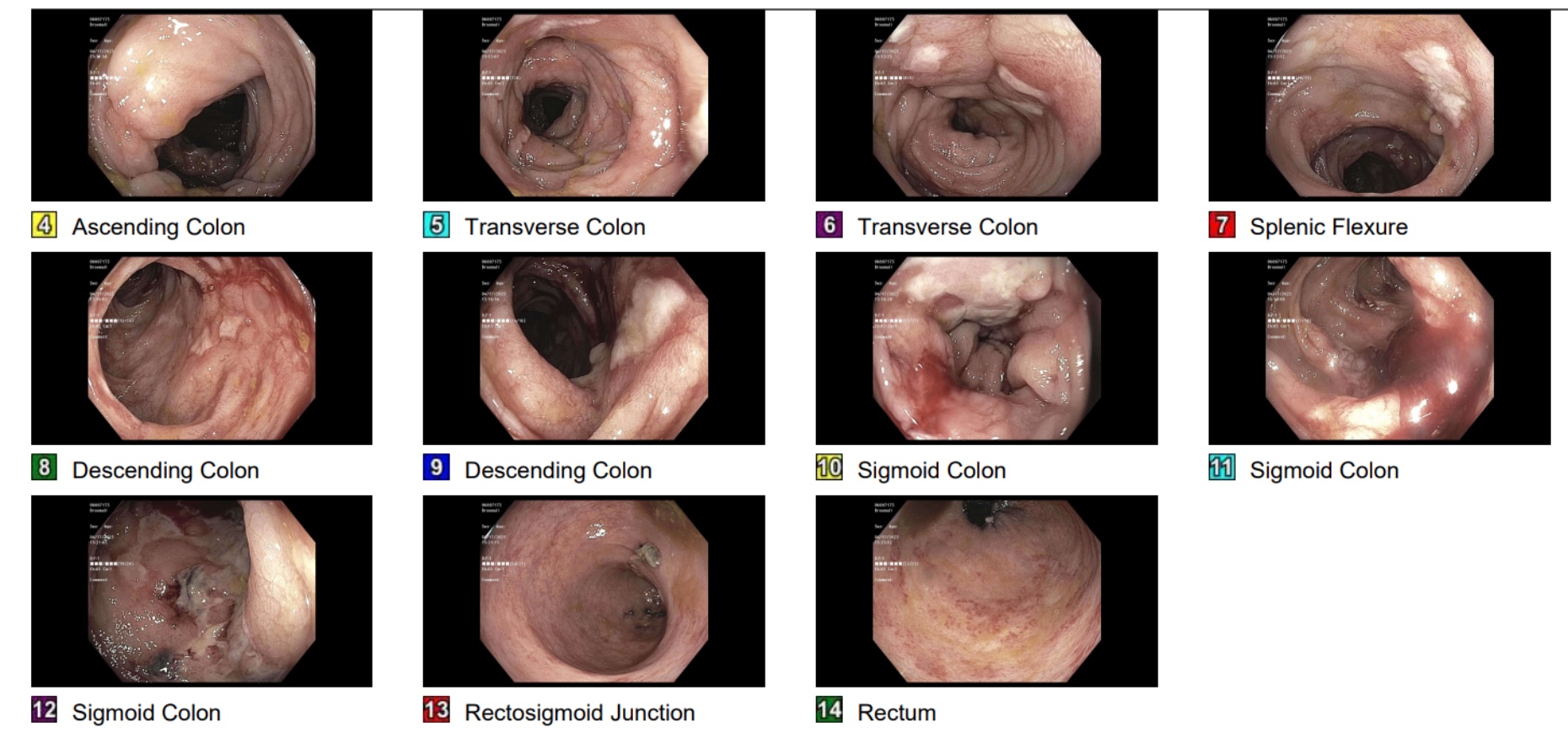
Figure: Figure 1. Colonoscopy showing diffuse colitis with ulcerations found in the sigmoid, descending, and transverse colon and scattered area of mildly friable mucosa found in the rectum.
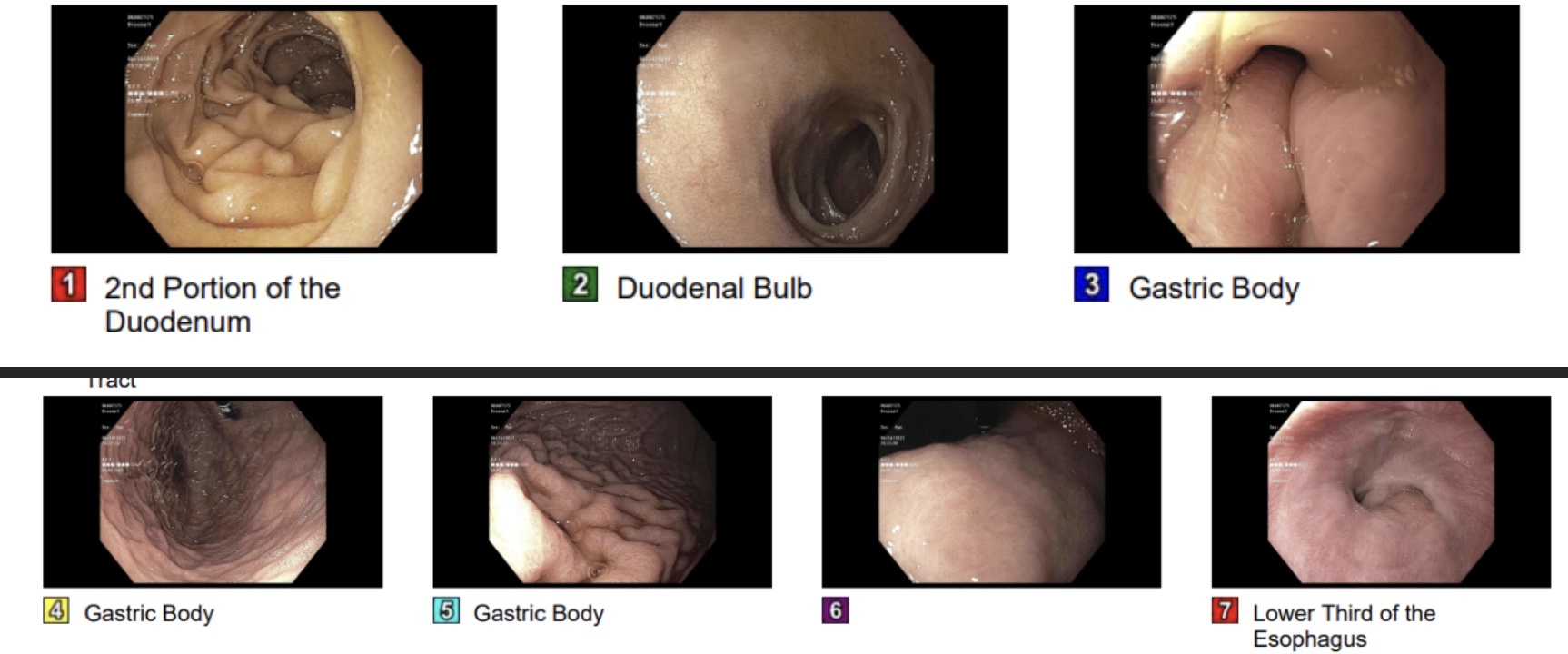
Figure: Figure 2. EGD showing normal mucosa in esophagus and duodenum with erythematous mucosa and thickened folds in the gastric fundus, body, incisura, and antrum.
Disclosures:
Christina Kanagawa indicated no relevant financial relationships.
Yara Sarkis indicated no relevant financial relationships.
Chelsea Edirisuriya indicated no relevant financial relationships.
Joshua DeSipio indicated no relevant financial relationships.
Krysta Contino indicated no relevant financial relationships.
Christina Kanagawa, DO1, Yara Sarkis, MD2, Chelsea Edirisuriya, MD2, Joshua DeSipio, MD3, Krysta Contino, MD4. P0998 - The Colitis Enigma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cooper University Hospital, Cherry Hill, NJ; 2Cooper University Hospital, Camden, NJ; 3Cooper Health Gastroenterology, Camden, NJ; 4Cooper Health Gastroenterology, Mount Laurel, NJ
Introduction: Rare conditions such as amyloidosis can present as colitis.
Case Description/
Methods: 73-year-old male with atrial fibrillation on apixaban and coronary artery disease presented with hematochezia and hypotension. Colonoscopy showed diffuse colitis with ulcerations and friability from rectosigmoid to transverse colon. There was initial concern for ischemic colitis. He was treated conservatively and discharged off apixaban with plan for repeat colonoscopy to assess healing and rule out inflammatory bowel disease (IBD). Patient was readmitted 2 weeks later for recurrent hematochezia. He informed us that he was just diagnosed with Multiple Myeloma (MM). Repeat colonoscopy showed persistent ulcerations without healing. Due to the recent diagnosis of MM, biopsies were sent for Congo Red stain as well as IBD. Pathology was positive for amyloidosis. To evaluate the extent of disease, endoscopy was done and revealed normal mucosa in stomach and duodenum with positive biopsies for amyloid. Video capsule endoscopy was also done and did not show small bowel (SB) abnormalities. Chemotherapy for MM was initiated with the goal of preventing further amyloid deposits in the gastrointestinal (GI) tract; however, it will not be curative. Unfortunately, he represented with similar symptoms 2 weeks later. Colorectal surgery evaluated him, and the decision was made to temporize bleeding with tranexamic acid as a bridge to allow for further chemotherapy and healing.
Discussion: Amyloidosis of the GI tract can have variable endoscopic findings. As evidenced in our patient, normal mucosa does not correlate with extent of disease, and endoscopic findings can mimic other pathologies, like IBD or ischemia. Diagnosis requires a high index of suspicion and special testing with Congo Red staining. There is no specific protocol to assess the extent of amyloid involvement, and it is unclear if deep enteroscopy for SB biopsy will change management. Moreover, there is no curative treatment for amyloidosis colitis as available therapies focus on underlying etiologies to prevent further deposits. Chemotherapy agents used to treat MM can be toxic to the colon and can worsen GI bleeding. Further studies are needed to implement a standardized protocol for diagnosis and management of this disease.
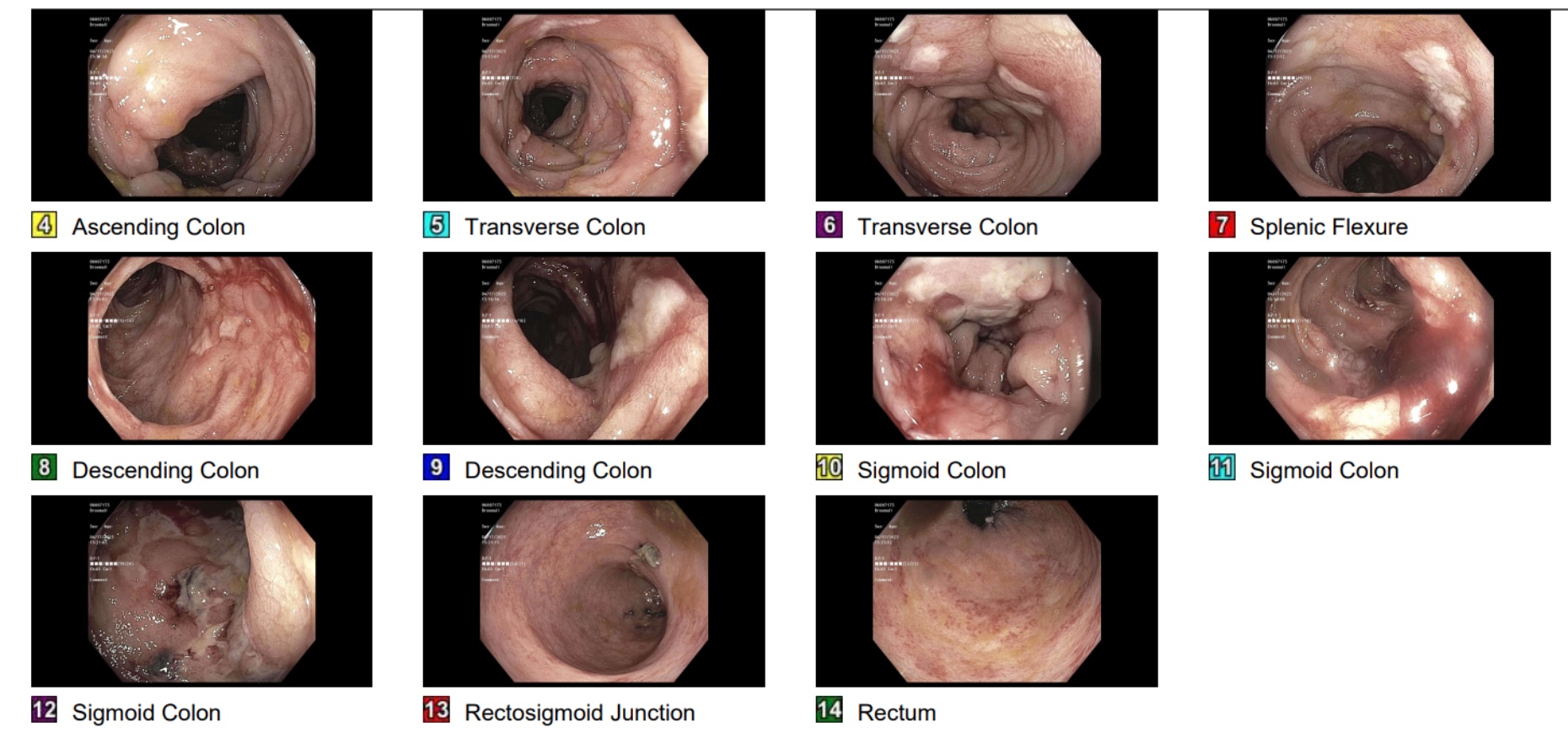
Figure: Figure 1. Colonoscopy showing diffuse colitis with ulcerations found in the sigmoid, descending, and transverse colon and scattered area of mildly friable mucosa found in the rectum.
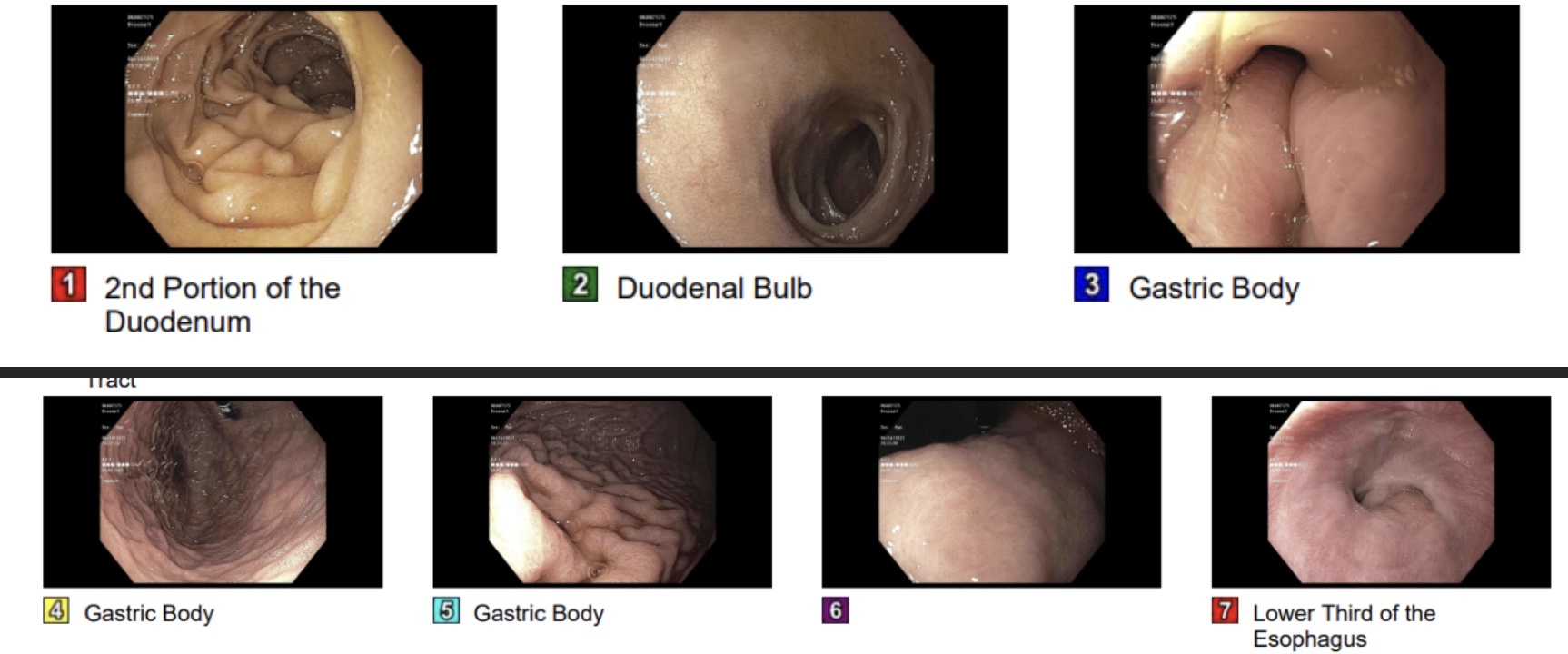
Figure: Figure 2. EGD showing normal mucosa in esophagus and duodenum with erythematous mucosa and thickened folds in the gastric fundus, body, incisura, and antrum.
Disclosures:
Christina Kanagawa indicated no relevant financial relationships.
Yara Sarkis indicated no relevant financial relationships.
Chelsea Edirisuriya indicated no relevant financial relationships.
Joshua DeSipio indicated no relevant financial relationships.
Krysta Contino indicated no relevant financial relationships.
Christina Kanagawa, DO1, Yara Sarkis, MD2, Chelsea Edirisuriya, MD2, Joshua DeSipio, MD3, Krysta Contino, MD4. P0998 - The Colitis Enigma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
