Sunday Poster Session
Category: GI Bleeding
P0995 - A Rare Hidden Hemorrhage: Fatal Stomal Varices in Portal Hypertension
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Wagmah Javed Khan, MD
St. Luke's Hospital
Chesterfield, MO
Presenting Author(s)
Wagmah Javed. Khan, MD1, Muhammad Arsalan, MD1, Hameed Ullah, MD1, Yusra Arooj, MD1, Anas M. Hasic, MD2, Elie Chahla, MD1
1St. Luke's Hospital, Chesterfield, MO; 2Sarajevo School of Science & Technology, Saint Louis, MO
Introduction: Stomal varices are a rare but clinically significant complication of portal hypertension, often seen in patients with a history of abdominal surgery resulting in an enterocutaneous fistula. Stomal varices account for less than 5% of all variceal bleeding in the setting of portal hypertension. The incidence of overt bleeding is 3-5%; however, mortality is substantial due to delayed recognition and the potential for massive hemorrhage. We present a strikingly rare case of a 60-year-old female who passed away from massive stomal variceal bleeding.
Case Description/
Methods: A 62-year-old female diagnosed with metastatic rectal cancer to the liver post-subtotal colectomy and end ileostomy presented with a significant drop in hemoglobin. She had a prior history of Grade II esophageal varices managed with band ligation, transfusions, and iron infusions. Initially, dark stool output in the ostomy bag raised suspicion for an upper GI bleed. EGD detected Grade I esophageal varices, portal hypertensive gastropathy, and post-banding ulcers with recent bleeding, and appropriate treatment was initiated. The following morning, while clearing her fresh blood-filled ostomy bag, the patient experienced cardiac arrest. Prompt ICU transfer was initiated after return of spontaneous circulation.
CTA confirmed dilated para-stomal vessel with no extravasation. A bedside ileoscopy revealed friable, engorged varices in the stoma that bled on light touch, leading to partial obstruction of the ostomy lumen. TIPS was recommended, and a specialized center transfer was initiated. However, within 24 hours, the patient became hypotensive, acutely hypoxic, and showed signs raising suspicion of DIC. Given her rapid deterioration and underlying malignancy, comfort care measures were initiated, and she passed away soon after.
Discussion: With only about 234 cases reported in the literature since 2008, this case emphasizes the need for awareness and prompt intervention in cases of rare bleeding stomal varices. Stomal varices should be considered in patients with an ileostomy presenting with unexplained bleeding or anemia in the setting of portal hypertension. The presence of an ostomy appliance can limit the direct inspection of stomal variceal bleeding, leading to late detection, highlighting the need for a thorough physical examination. CTA or MRA can help with diagnosis; however, intermittent or subtle bleeds may be missed. Direct endoscopic evaluation through the stoma remains definitive, and treatment options include TIPS.
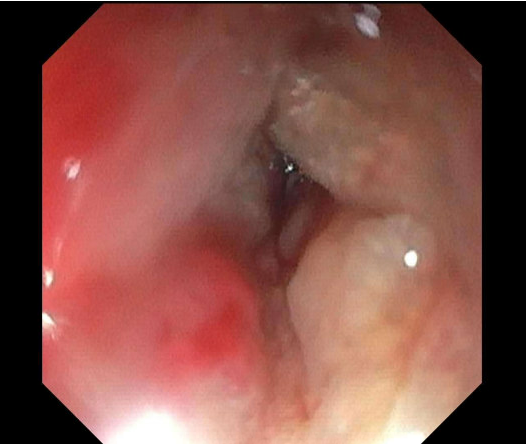
Figure: Stomal varices visualized by ileoscopy
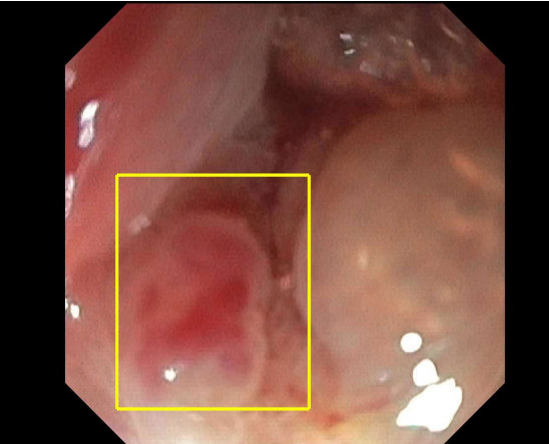
Figure: Partial obstruction of the ileostomy opening; friable and engorged mucosa
Disclosures:
Wagmah Khan indicated no relevant financial relationships.
Muhammad Arsalan indicated no relevant financial relationships.
Hameed Ullah indicated no relevant financial relationships.
Yusra Arooj indicated no relevant financial relationships.
Anas Hasic indicated no relevant financial relationships.
Elie Chahla indicated no relevant financial relationships.
Wagmah Javed. Khan, MD1, Muhammad Arsalan, MD1, Hameed Ullah, MD1, Yusra Arooj, MD1, Anas M. Hasic, MD2, Elie Chahla, MD1. P0995 - A Rare Hidden Hemorrhage: Fatal Stomal Varices in Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Luke's Hospital, Chesterfield, MO; 2Sarajevo School of Science & Technology, Saint Louis, MO
Introduction: Stomal varices are a rare but clinically significant complication of portal hypertension, often seen in patients with a history of abdominal surgery resulting in an enterocutaneous fistula. Stomal varices account for less than 5% of all variceal bleeding in the setting of portal hypertension. The incidence of overt bleeding is 3-5%; however, mortality is substantial due to delayed recognition and the potential for massive hemorrhage. We present a strikingly rare case of a 60-year-old female who passed away from massive stomal variceal bleeding.
Case Description/
Methods: A 62-year-old female diagnosed with metastatic rectal cancer to the liver post-subtotal colectomy and end ileostomy presented with a significant drop in hemoglobin. She had a prior history of Grade II esophageal varices managed with band ligation, transfusions, and iron infusions. Initially, dark stool output in the ostomy bag raised suspicion for an upper GI bleed. EGD detected Grade I esophageal varices, portal hypertensive gastropathy, and post-banding ulcers with recent bleeding, and appropriate treatment was initiated. The following morning, while clearing her fresh blood-filled ostomy bag, the patient experienced cardiac arrest. Prompt ICU transfer was initiated after return of spontaneous circulation.
CTA confirmed dilated para-stomal vessel with no extravasation. A bedside ileoscopy revealed friable, engorged varices in the stoma that bled on light touch, leading to partial obstruction of the ostomy lumen. TIPS was recommended, and a specialized center transfer was initiated. However, within 24 hours, the patient became hypotensive, acutely hypoxic, and showed signs raising suspicion of DIC. Given her rapid deterioration and underlying malignancy, comfort care measures were initiated, and she passed away soon after.
Discussion: With only about 234 cases reported in the literature since 2008, this case emphasizes the need for awareness and prompt intervention in cases of rare bleeding stomal varices. Stomal varices should be considered in patients with an ileostomy presenting with unexplained bleeding or anemia in the setting of portal hypertension. The presence of an ostomy appliance can limit the direct inspection of stomal variceal bleeding, leading to late detection, highlighting the need for a thorough physical examination. CTA or MRA can help with diagnosis; however, intermittent or subtle bleeds may be missed. Direct endoscopic evaluation through the stoma remains definitive, and treatment options include TIPS.
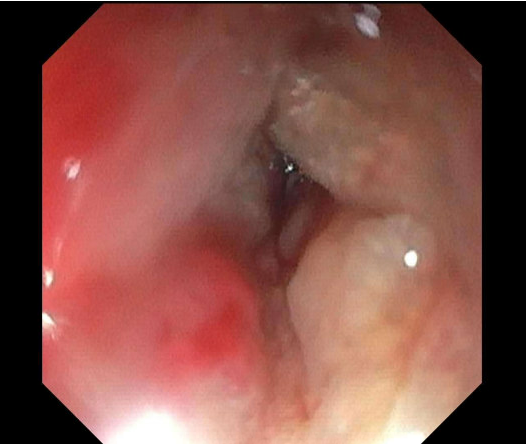
Figure: Stomal varices visualized by ileoscopy
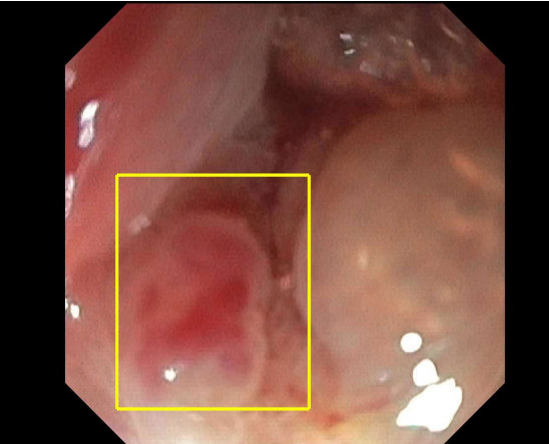
Figure: Partial obstruction of the ileostomy opening; friable and engorged mucosa
Disclosures:
Wagmah Khan indicated no relevant financial relationships.
Muhammad Arsalan indicated no relevant financial relationships.
Hameed Ullah indicated no relevant financial relationships.
Yusra Arooj indicated no relevant financial relationships.
Anas Hasic indicated no relevant financial relationships.
Elie Chahla indicated no relevant financial relationships.
Wagmah Javed. Khan, MD1, Muhammad Arsalan, MD1, Hameed Ullah, MD1, Yusra Arooj, MD1, Anas M. Hasic, MD2, Elie Chahla, MD1. P0995 - A Rare Hidden Hemorrhage: Fatal Stomal Varices in Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
