Sunday Poster Session
Category: GI Bleeding
P0992 - Melena Uncovering Gastric Polyps as an Unusual Site of Renal Cell Carcinoma Metastases
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- BS
Brandon Stahl, MD (he/him/his)
Albany Medical Center
Albany, NY
Presenting Author(s)
Award: ACG Presidential Poster Award
Brandon Stahl, MD, Anika Paradkar, MD, Lynn Guo, MD, Seth Richter, MD, FACG
Albany Medical Center, Albany, NY
Introduction: Renal cell carcinoma (RCC) is the ninth most common cancer diagnosis in the US. Metastases most commonly occur to lungs, bones, lymph nodes, and liver, and metastases to the GI tract occur in less than 1% of patients. Our patient has a longstanding history of RCC and underwent left nephrectomy at the time of his initial diagnosis. Ten years later he was found to have metastatic disease after a pathologic fracture of the right humerus. During admission to address the fracture, he developed a gastrointestinal bleed, which led to the discovery of further metastatic lesions in the stomach.
Case Description/
Methods: A 70-year-old male with a history of metastatic clear cell RCC (ccRCC) who underwent nephrectomy 10 years prior presented with agitation after an elective preoperative embolization of a known right humeral metastatic lesion. His initial labs were remarkable for a hemoglobin of 6.1 g/dL and BUN of 23 mg/dL. Throughout his hospitalization, the patient required 10 units of pRBCs and 1 unit of FFP. Gastroenterology was consulted after the patient had melena for 2 days. He underwent EGD which showed multiple 2 to 25 mm pedunculated and sessile bleeding polyps (Figure 1). Three polyps were resected with pathology showing fragments of metastatic carcinoma with clear cytoplasm, consistent with his known ccRCC (Figure 2).
Discussion: Although gastric metastases of RCC are rare, occurring in only 0.2-0.7% of patients with metastatic RCC, our patient had several risk factors for developing gastric metastases. Most notably, that he already had bone metastases at the time of presentation. Additionally, he was 10 years out from his nephrectomy, with a longer interval from surgery conferring an increased risk. Unexplained anemia and gastrointestinal bleeding are the most common presentations of gastric metastases. Though the patient did not initially present to the hospital with a GI bleed, his degree of anemia indicates that he had been bleeding for some time prior to admission. Currently, there are no formal guidelines for endoscopic surveillance in this patient population, however based on cohort studies and expert opinion there should be a low threshold to pursue EGD if there is an unexplained anemia among metastatic RCC patients with the aforementioned risk factors. A more stringent surveillance guideline would allow for more expeditious initiation of systemic therapy or escalation of therapy.

Figure: Figure 1. Pedunculated and sessile bleeding gastric polyps ranging in size from 2 to 25 mm.
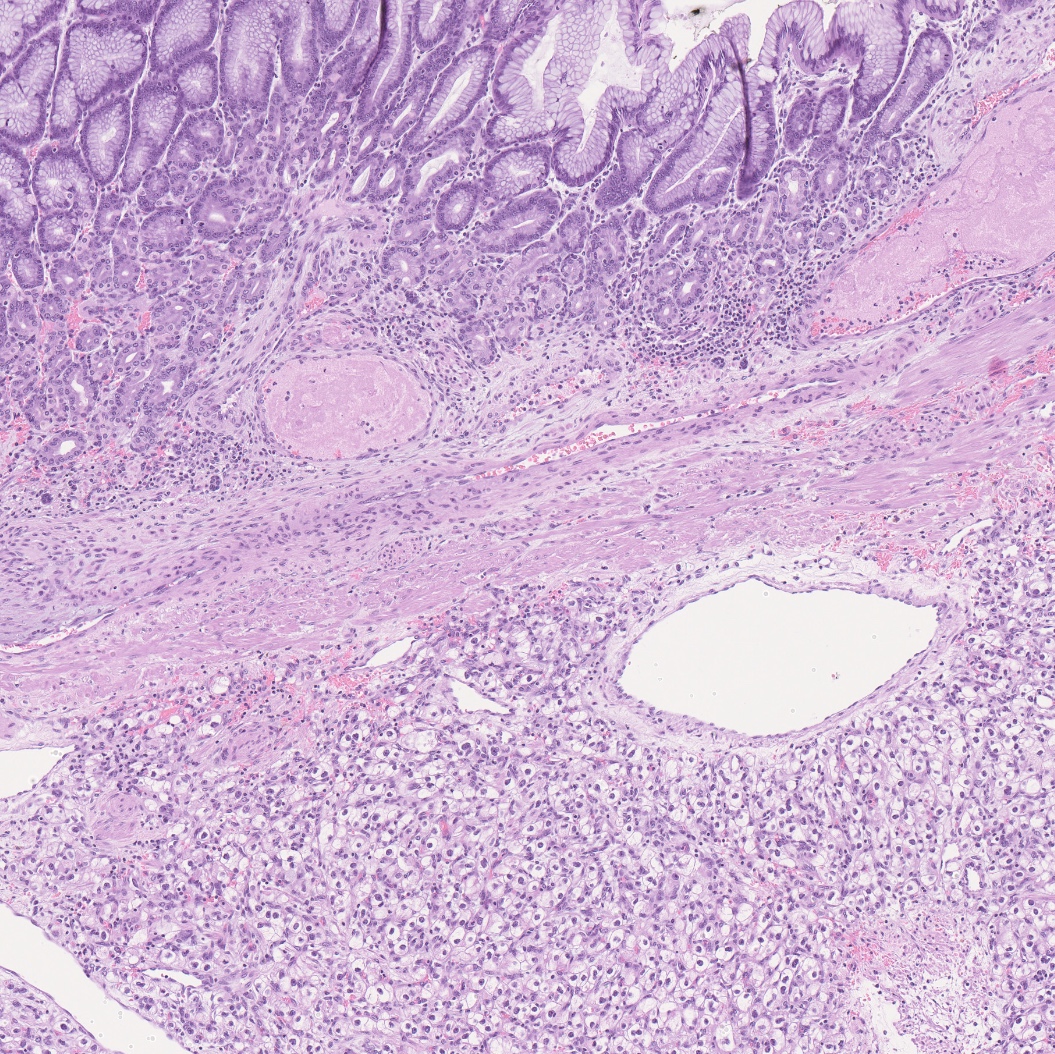
Figure: Metastatic clear cell renal cell carcinoma underlying gastric mucosa
Disclosures:
Brandon Stahl indicated no relevant financial relationships.
Anika Paradkar indicated no relevant financial relationships.
Lynn Guo indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Brandon Stahl, MD, Anika Paradkar, MD, Lynn Guo, MD, Seth Richter, MD, FACG. P0992 - Melena Uncovering Gastric Polyps as an Unusual Site of Renal Cell Carcinoma Metastases, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Brandon Stahl, MD, Anika Paradkar, MD, Lynn Guo, MD, Seth Richter, MD, FACG
Albany Medical Center, Albany, NY
Introduction: Renal cell carcinoma (RCC) is the ninth most common cancer diagnosis in the US. Metastases most commonly occur to lungs, bones, lymph nodes, and liver, and metastases to the GI tract occur in less than 1% of patients. Our patient has a longstanding history of RCC and underwent left nephrectomy at the time of his initial diagnosis. Ten years later he was found to have metastatic disease after a pathologic fracture of the right humerus. During admission to address the fracture, he developed a gastrointestinal bleed, which led to the discovery of further metastatic lesions in the stomach.
Case Description/
Methods: A 70-year-old male with a history of metastatic clear cell RCC (ccRCC) who underwent nephrectomy 10 years prior presented with agitation after an elective preoperative embolization of a known right humeral metastatic lesion. His initial labs were remarkable for a hemoglobin of 6.1 g/dL and BUN of 23 mg/dL. Throughout his hospitalization, the patient required 10 units of pRBCs and 1 unit of FFP. Gastroenterology was consulted after the patient had melena for 2 days. He underwent EGD which showed multiple 2 to 25 mm pedunculated and sessile bleeding polyps (Figure 1). Three polyps were resected with pathology showing fragments of metastatic carcinoma with clear cytoplasm, consistent with his known ccRCC (Figure 2).
Discussion: Although gastric metastases of RCC are rare, occurring in only 0.2-0.7% of patients with metastatic RCC, our patient had several risk factors for developing gastric metastases. Most notably, that he already had bone metastases at the time of presentation. Additionally, he was 10 years out from his nephrectomy, with a longer interval from surgery conferring an increased risk. Unexplained anemia and gastrointestinal bleeding are the most common presentations of gastric metastases. Though the patient did not initially present to the hospital with a GI bleed, his degree of anemia indicates that he had been bleeding for some time prior to admission. Currently, there are no formal guidelines for endoscopic surveillance in this patient population, however based on cohort studies and expert opinion there should be a low threshold to pursue EGD if there is an unexplained anemia among metastatic RCC patients with the aforementioned risk factors. A more stringent surveillance guideline would allow for more expeditious initiation of systemic therapy or escalation of therapy.

Figure: Figure 1. Pedunculated and sessile bleeding gastric polyps ranging in size from 2 to 25 mm.
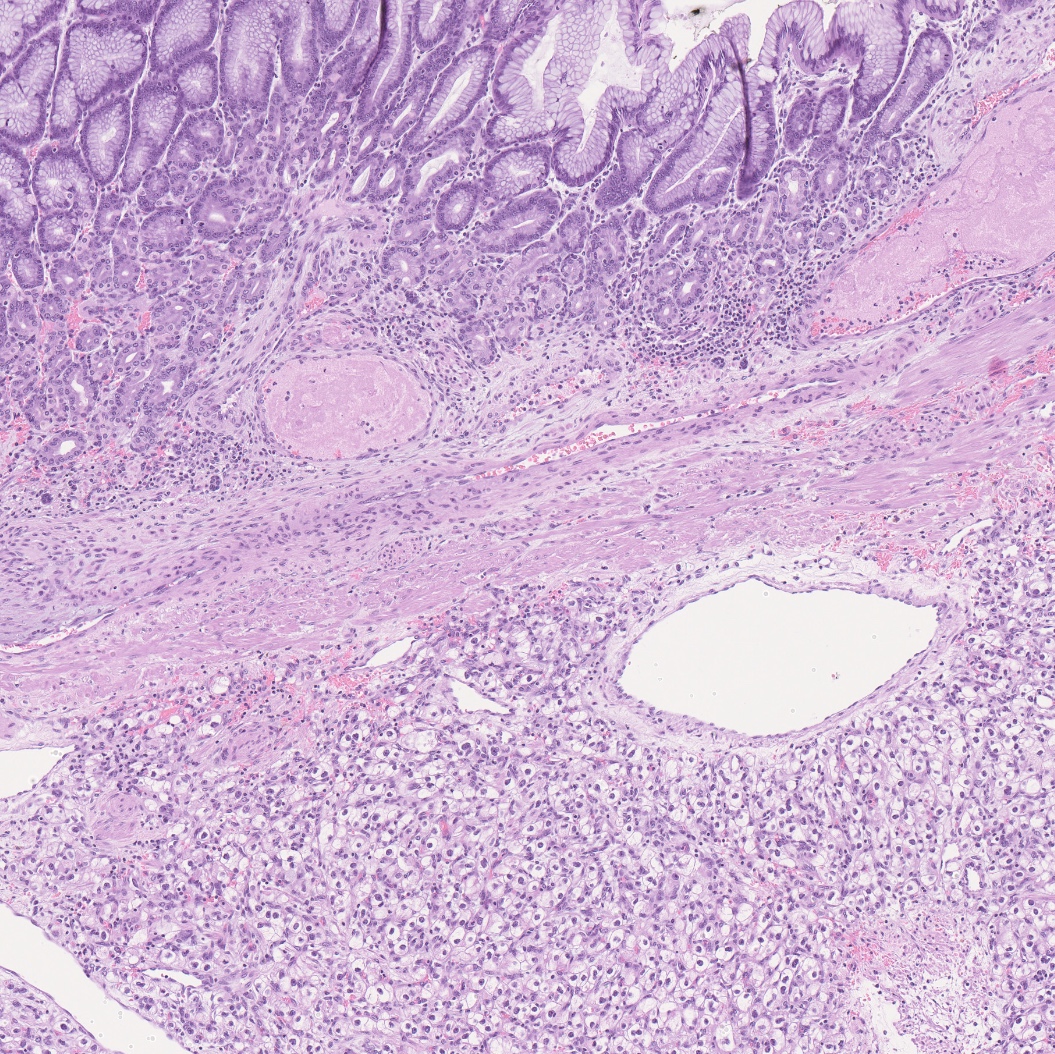
Figure: Metastatic clear cell renal cell carcinoma underlying gastric mucosa
Disclosures:
Brandon Stahl indicated no relevant financial relationships.
Anika Paradkar indicated no relevant financial relationships.
Lynn Guo indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Brandon Stahl, MD, Anika Paradkar, MD, Lynn Guo, MD, Seth Richter, MD, FACG. P0992 - Melena Uncovering Gastric Polyps as an Unusual Site of Renal Cell Carcinoma Metastases, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

