Sunday Poster Session
Category: GI Bleeding
P0986 - Bleeding Small Bowel Arteriovenous Malformation in Cowden Syndrome: A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Samantha Woller, MD, MS
Creighton University Medical Center
Omaha, NE
Presenting Author(s)
Samantha Woller, MD, MS1, Kyaw Min Tun, DO2, Nurlan Aliyev, MD3, Erin Jenkins, MD2
1Creighton University Medical Center, Omaha, NE; 2Creighton University School of Medicine, Omaha, NE; 3University of Nebraska Medical Center, Elkhorn, NE
Introduction: Cowden syndrome is a rare disease caused by a PTEN gene mutation, resulting in multiple hamartomas with an increased malignancy risk. Few cases of arteriovenous malformations (AVMs) have been reported in patients with Cowden syndrome. This case presents a 48-year-old female with Cowden syndrome and recurrent gastrointestinal (GI) bleed secondary to small bowel AVM.
Case Description/
Methods: A 48-year-old female with Cowden syndrome presented with melena and hypotension. Workup revealed a hemoglobin (hgb) of 5.3 g/dl. CT angiogram (CTA) and esophagogastroduodenoscopy (EGD) did not reveal a source of bleeding. Despite stabilization efforts, she continued to have melena, prompting colonoscopy, tagged red blood cell scan, and video capsule endoscopy (VCE). These revealed small polypoid lesions, likely hamartomas consistent with Cowden syndrome, and hematin throughout the colon, but no source of bleeding. She stabilized after multiple transfusions and was discharged.
Two weeks later, she returned with hgb of 4.6 g/dl and now requiring vasopressor support. Repeat CTA and EGD were again inconclusive. A second VCE localized bleeding to the proximal jejunum. Push enteroscopy found a visible vessel with adherent clot which was treated with epinephrine and clipping. She was discharged without further signs of bleeding.
She presented again the following day with melena and hypotension. Repeat enteroscopy revealed blood within the proximal jejunum, prompting urgent embolization. Imaging during embolization noted findings consistent with a large AVM near prior clips. Unfortunately, symptoms returned yet again.
Final EGD revealed a 5 cm oozing circumferential ulcer with mucosal congestion in the proximal tissue. She underwent resection of the affected segment and has not had recurrence of symptoms.
Discussion: This case illustrates a rare but serious complication of Cowden syndrome – bleeding from small bowel AVMs. While hamartomas are well documented in Cowden syndrome, AVMs are exceedingly rare, with only a few reports, and just one previous case of upper GI bleed requiring surgical resection. Our case highlights the diagnostic and therapeutic challenges in identifying and managing small bowel AVMs in this population. Despite imaging, endoscopy, and embolization, only surgery achieved definitive hemostasis. This report emphasizes the need to consider vascular anomalies in patients with Cowden syndrome and unexplained GI bleeding and the value of multidisciplinary intervention when conservative measures fail.
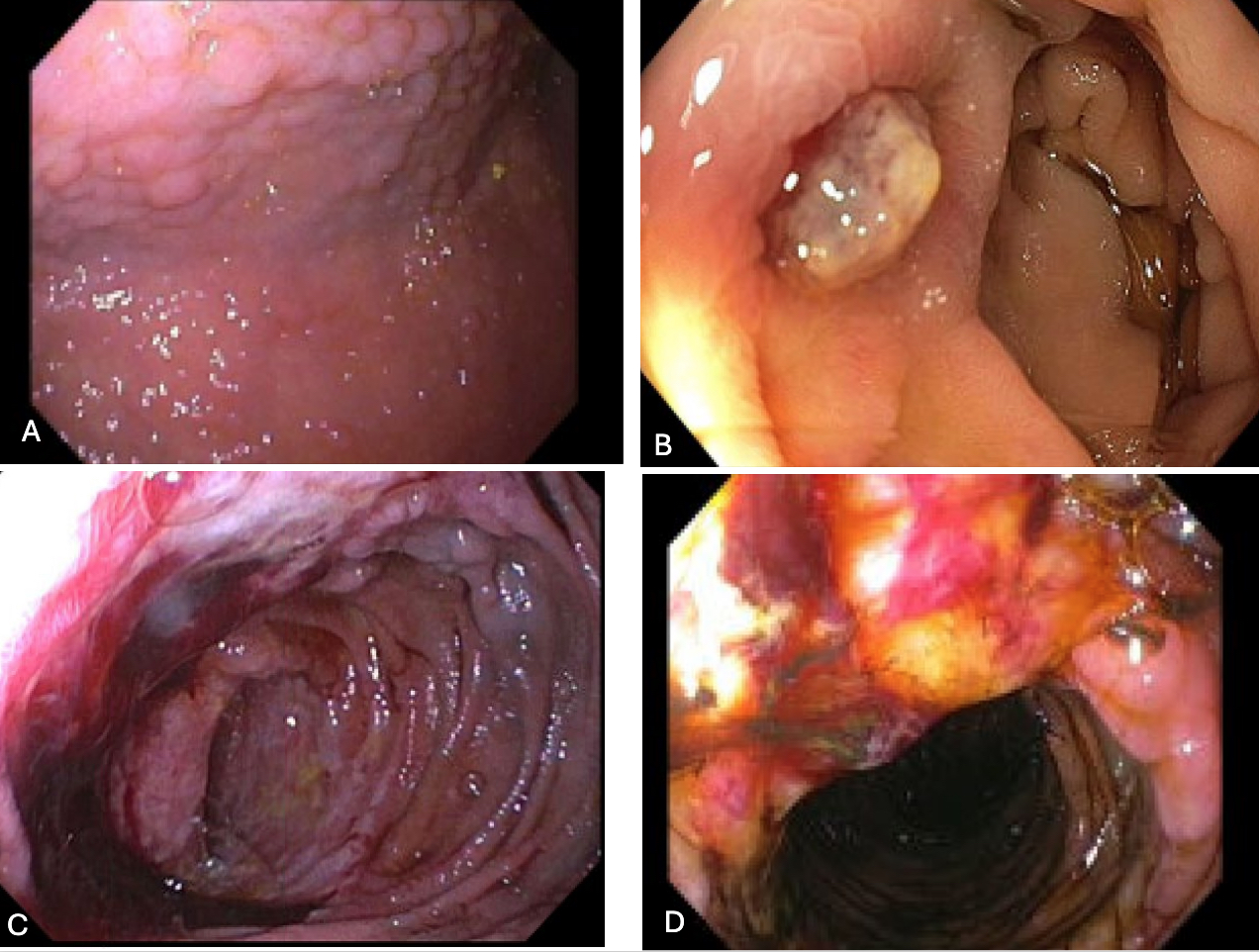
Figure: Figure 1.
A. Hamartomas within the gastric body, consistent with Cowden Syndrome
B. Ulcer with adherent clot in the proximal jejunum, 8/13/24
C and D. Bleeding circumferential ulcer in the proximal jejunum, 9/9/24
Disclosures:
Samantha Woller indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Nurlan Aliyev indicated no relevant financial relationships.
Erin Jenkins indicated no relevant financial relationships.
Samantha Woller, MD, MS1, Kyaw Min Tun, DO2, Nurlan Aliyev, MD3, Erin Jenkins, MD2. P0986 - Bleeding Small Bowel Arteriovenous Malformation in Cowden Syndrome: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University Medical Center, Omaha, NE; 2Creighton University School of Medicine, Omaha, NE; 3University of Nebraska Medical Center, Elkhorn, NE
Introduction: Cowden syndrome is a rare disease caused by a PTEN gene mutation, resulting in multiple hamartomas with an increased malignancy risk. Few cases of arteriovenous malformations (AVMs) have been reported in patients with Cowden syndrome. This case presents a 48-year-old female with Cowden syndrome and recurrent gastrointestinal (GI) bleed secondary to small bowel AVM.
Case Description/
Methods: A 48-year-old female with Cowden syndrome presented with melena and hypotension. Workup revealed a hemoglobin (hgb) of 5.3 g/dl. CT angiogram (CTA) and esophagogastroduodenoscopy (EGD) did not reveal a source of bleeding. Despite stabilization efforts, she continued to have melena, prompting colonoscopy, tagged red blood cell scan, and video capsule endoscopy (VCE). These revealed small polypoid lesions, likely hamartomas consistent with Cowden syndrome, and hematin throughout the colon, but no source of bleeding. She stabilized after multiple transfusions and was discharged.
Two weeks later, she returned with hgb of 4.6 g/dl and now requiring vasopressor support. Repeat CTA and EGD were again inconclusive. A second VCE localized bleeding to the proximal jejunum. Push enteroscopy found a visible vessel with adherent clot which was treated with epinephrine and clipping. She was discharged without further signs of bleeding.
She presented again the following day with melena and hypotension. Repeat enteroscopy revealed blood within the proximal jejunum, prompting urgent embolization. Imaging during embolization noted findings consistent with a large AVM near prior clips. Unfortunately, symptoms returned yet again.
Final EGD revealed a 5 cm oozing circumferential ulcer with mucosal congestion in the proximal tissue. She underwent resection of the affected segment and has not had recurrence of symptoms.
Discussion: This case illustrates a rare but serious complication of Cowden syndrome – bleeding from small bowel AVMs. While hamartomas are well documented in Cowden syndrome, AVMs are exceedingly rare, with only a few reports, and just one previous case of upper GI bleed requiring surgical resection. Our case highlights the diagnostic and therapeutic challenges in identifying and managing small bowel AVMs in this population. Despite imaging, endoscopy, and embolization, only surgery achieved definitive hemostasis. This report emphasizes the need to consider vascular anomalies in patients with Cowden syndrome and unexplained GI bleeding and the value of multidisciplinary intervention when conservative measures fail.
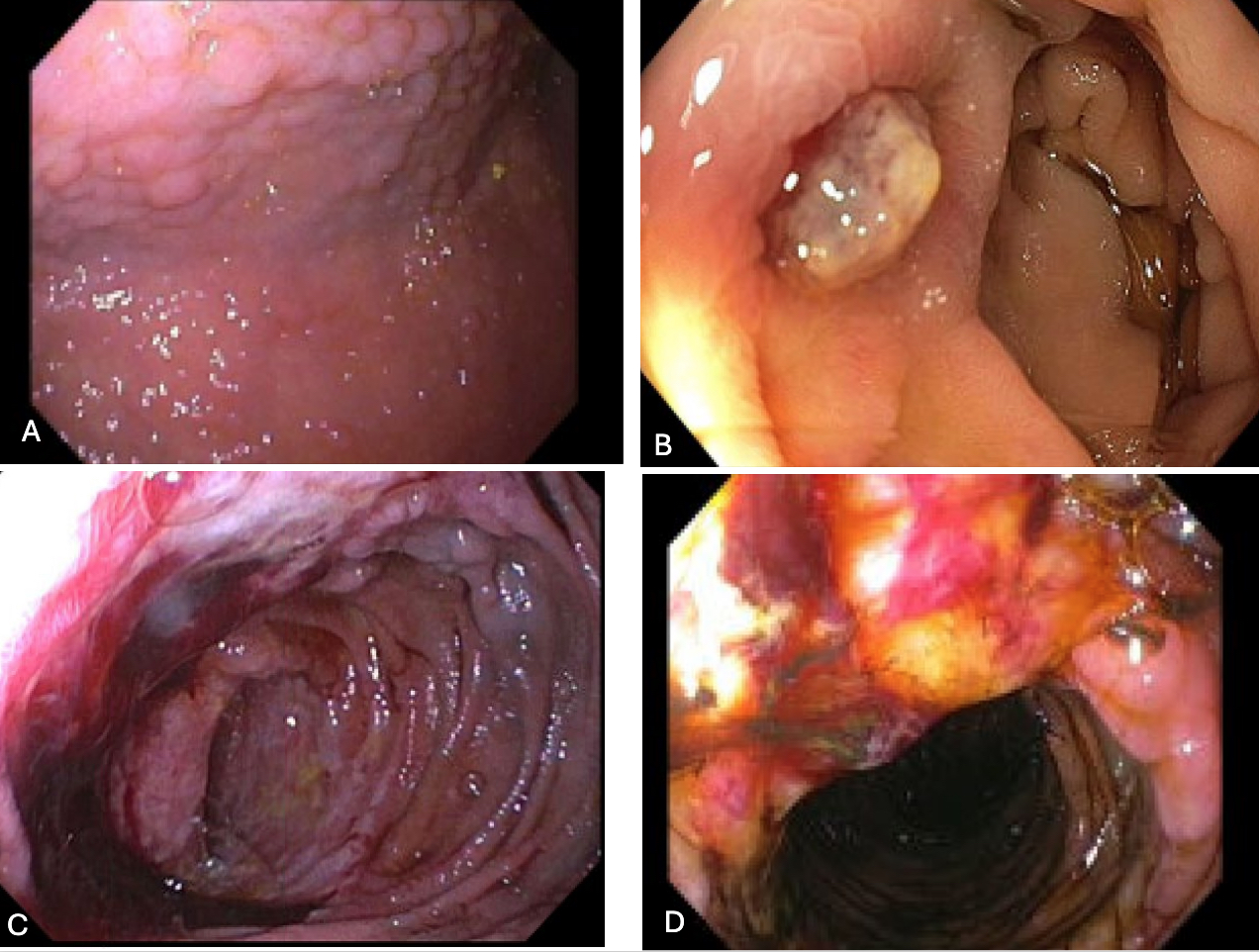
Figure: Figure 1.
A. Hamartomas within the gastric body, consistent with Cowden Syndrome
B. Ulcer with adherent clot in the proximal jejunum, 8/13/24
C and D. Bleeding circumferential ulcer in the proximal jejunum, 9/9/24
Disclosures:
Samantha Woller indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Nurlan Aliyev indicated no relevant financial relationships.
Erin Jenkins indicated no relevant financial relationships.
Samantha Woller, MD, MS1, Kyaw Min Tun, DO2, Nurlan Aliyev, MD3, Erin Jenkins, MD2. P0986 - Bleeding Small Bowel Arteriovenous Malformation in Cowden Syndrome: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
