Sunday Poster Session
Category: GI Bleeding
P0962 - A Gastroenteric Fistulation Preventing Peptic Ulcer Perforation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jerry Kong, BS (he/him/his)
NYU Grossman School of Medicine
New York, NY
Presenting Author(s)
Jerry Kong, BS1, Lindsey Sattler, MD2, Courtney Balgobin, MD1
1NYU Grossman School of Medicine, New York, NY; 2NYU Langone Health, New York, NY
Introduction: Gastrointestinal (GI) fistulas are abnormal connections between the GI tract and an epithelialized surface, such as skin, bladder, or another section of GI tract. Common causes of GI fistulas include surgery, radiation, malignancy, inflammatory bowel disease (IBD), and diverticular disease. We present a case of an elderly woman with a fortuitous fistulation between the stomach and small bowel as a suspected complication from methotrexate toxicity causing a gastric ulcer.
Case Description/
Methods: A 73-year-old woman with a history of rheumatoid arthritis treated with methotrexate and gastroesophageal reflux disease presented as a transfer from an outside hospital (OSH) after presenting with 1 week of hematemesis and weakness. She had no known history of surgery, radiation, IBD, or cancer. Notably, the patient had been taking 25mg of methotrexate daily rather than weekly as prescribed. She presented with a hemoglobin of 4.5g/dL and underwent an esophagogastroduodenoscopy (EGD) that reportedly revealed concern for a large mass with underlying ulceration, which was biopsied.
Biopsies were consistent with chronic inactive gastritis, negative for H. pylori from the ulcer base, and showed predominantly fragments of small bowel mucosa. She was found to have bilateral pulmonary embolisms after staging computed tomography (CT) scans and was started on anticoagulation but subsequently developed massive hematemesis. She was stabilized and transferred for inferior vena cava filter placement.
Given concern for gastric malignancy from OSH, a repeat EGD showed a large non-malignant-appearing ulcer at the incisura with small bowel mucosa protruding through a fistula. The fistula was traversed with findings consistent with small bowel lumen and villous mucosa on the other side. Review of CT abdomen suggested that the stomach fistulized to the proximal jejunum. In consultation with general surgery, the etiology of the fistula was thought to be secondary to methotrexate toxicity with possibility of spontaneous closure after cessation of methotrexate. The patient was discharged with plans for close follow-up and repeat EGD.
Discussion: We report a rare case of a gastroenteric fistula secondary to gastric ulceration likely caused by methotrexate toxicity. The serendipitous location of the patient’s proximal jejunum may have saved the patient from an ulcer perforation in the abdominal cavity. This case emphasizes the need for doctors to regularly assess patients' understanding of treatment regimens.

Figure: Figure 1. Images from the patient’s first EGD at OSH show protruding small bowel mucosa initially reported as a large mass in the center of an underlying ulcer bed near the incisura of the stomach. This was thought to be suspicious for malignancy. Biopsies were taken of both the protruding mucosa and the underlying ulcer bed.
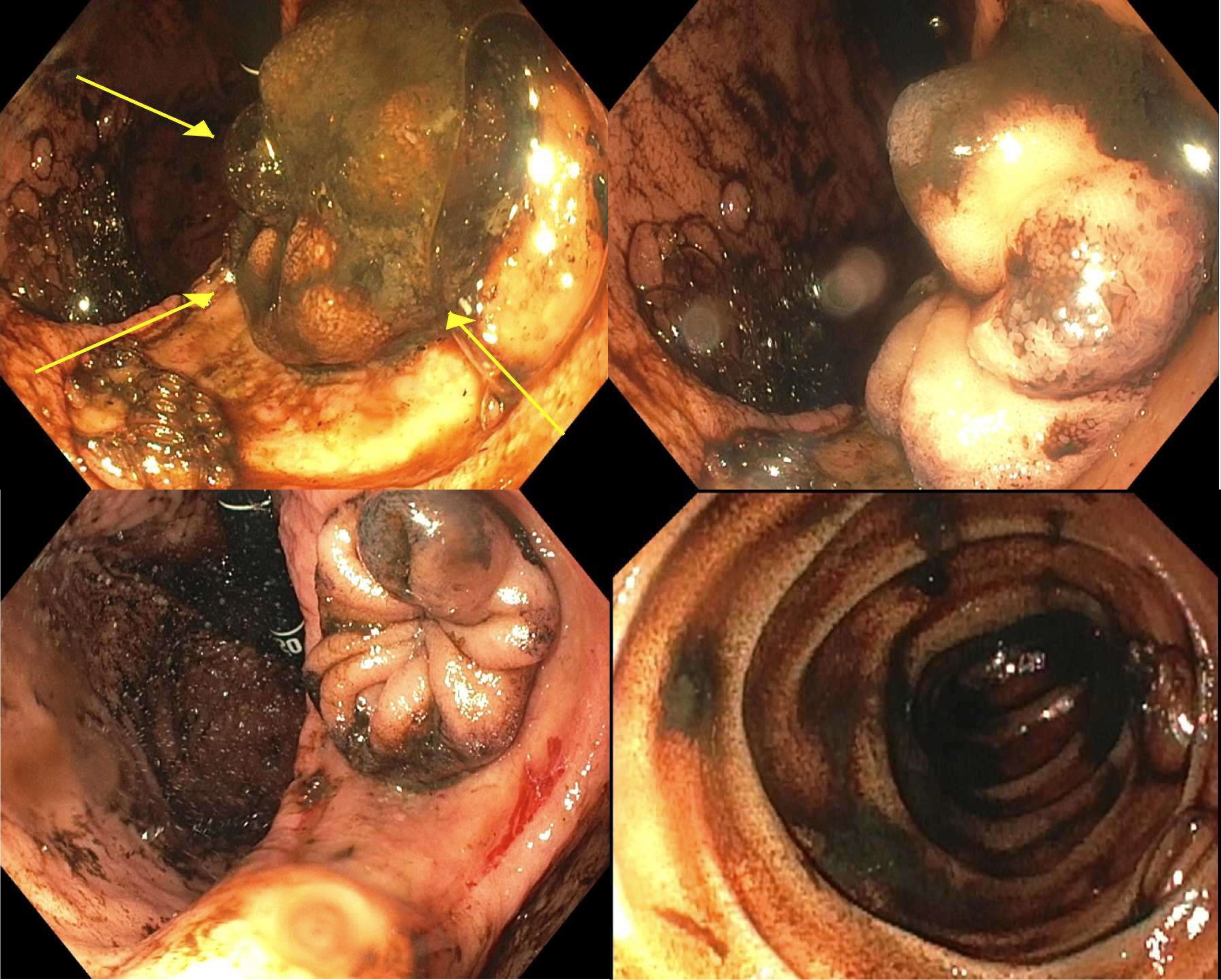
Figure: Figure 2. Images from the patient’s repeat inpatient EGD show an 8 cm clean-based ulcer bed with small bowel mucosa protruding through a fistula. Note the abundance of hematin in the setting of bleeding after starting anticoagulation. The image on the bottom right shows small bowel which was visualized upon traversing through the protruding small bowel mucosa and fistula tract.
Disclosures:
Jerry Kong indicated no relevant financial relationships.
Lindsey Sattler indicated no relevant financial relationships.
Courtney Balgobin indicated no relevant financial relationships.
Jerry Kong, BS1, Lindsey Sattler, MD2, Courtney Balgobin, MD1. P0962 - A Gastroenteric Fistulation Preventing Peptic Ulcer Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYU Grossman School of Medicine, New York, NY; 2NYU Langone Health, New York, NY
Introduction: Gastrointestinal (GI) fistulas are abnormal connections between the GI tract and an epithelialized surface, such as skin, bladder, or another section of GI tract. Common causes of GI fistulas include surgery, radiation, malignancy, inflammatory bowel disease (IBD), and diverticular disease. We present a case of an elderly woman with a fortuitous fistulation between the stomach and small bowel as a suspected complication from methotrexate toxicity causing a gastric ulcer.
Case Description/
Methods: A 73-year-old woman with a history of rheumatoid arthritis treated with methotrexate and gastroesophageal reflux disease presented as a transfer from an outside hospital (OSH) after presenting with 1 week of hematemesis and weakness. She had no known history of surgery, radiation, IBD, or cancer. Notably, the patient had been taking 25mg of methotrexate daily rather than weekly as prescribed. She presented with a hemoglobin of 4.5g/dL and underwent an esophagogastroduodenoscopy (EGD) that reportedly revealed concern for a large mass with underlying ulceration, which was biopsied.
Biopsies were consistent with chronic inactive gastritis, negative for H. pylori from the ulcer base, and showed predominantly fragments of small bowel mucosa. She was found to have bilateral pulmonary embolisms after staging computed tomography (CT) scans and was started on anticoagulation but subsequently developed massive hematemesis. She was stabilized and transferred for inferior vena cava filter placement.
Given concern for gastric malignancy from OSH, a repeat EGD showed a large non-malignant-appearing ulcer at the incisura with small bowel mucosa protruding through a fistula. The fistula was traversed with findings consistent with small bowel lumen and villous mucosa on the other side. Review of CT abdomen suggested that the stomach fistulized to the proximal jejunum. In consultation with general surgery, the etiology of the fistula was thought to be secondary to methotrexate toxicity with possibility of spontaneous closure after cessation of methotrexate. The patient was discharged with plans for close follow-up and repeat EGD.
Discussion: We report a rare case of a gastroenteric fistula secondary to gastric ulceration likely caused by methotrexate toxicity. The serendipitous location of the patient’s proximal jejunum may have saved the patient from an ulcer perforation in the abdominal cavity. This case emphasizes the need for doctors to regularly assess patients' understanding of treatment regimens.

Figure: Figure 1. Images from the patient’s first EGD at OSH show protruding small bowel mucosa initially reported as a large mass in the center of an underlying ulcer bed near the incisura of the stomach. This was thought to be suspicious for malignancy. Biopsies were taken of both the protruding mucosa and the underlying ulcer bed.
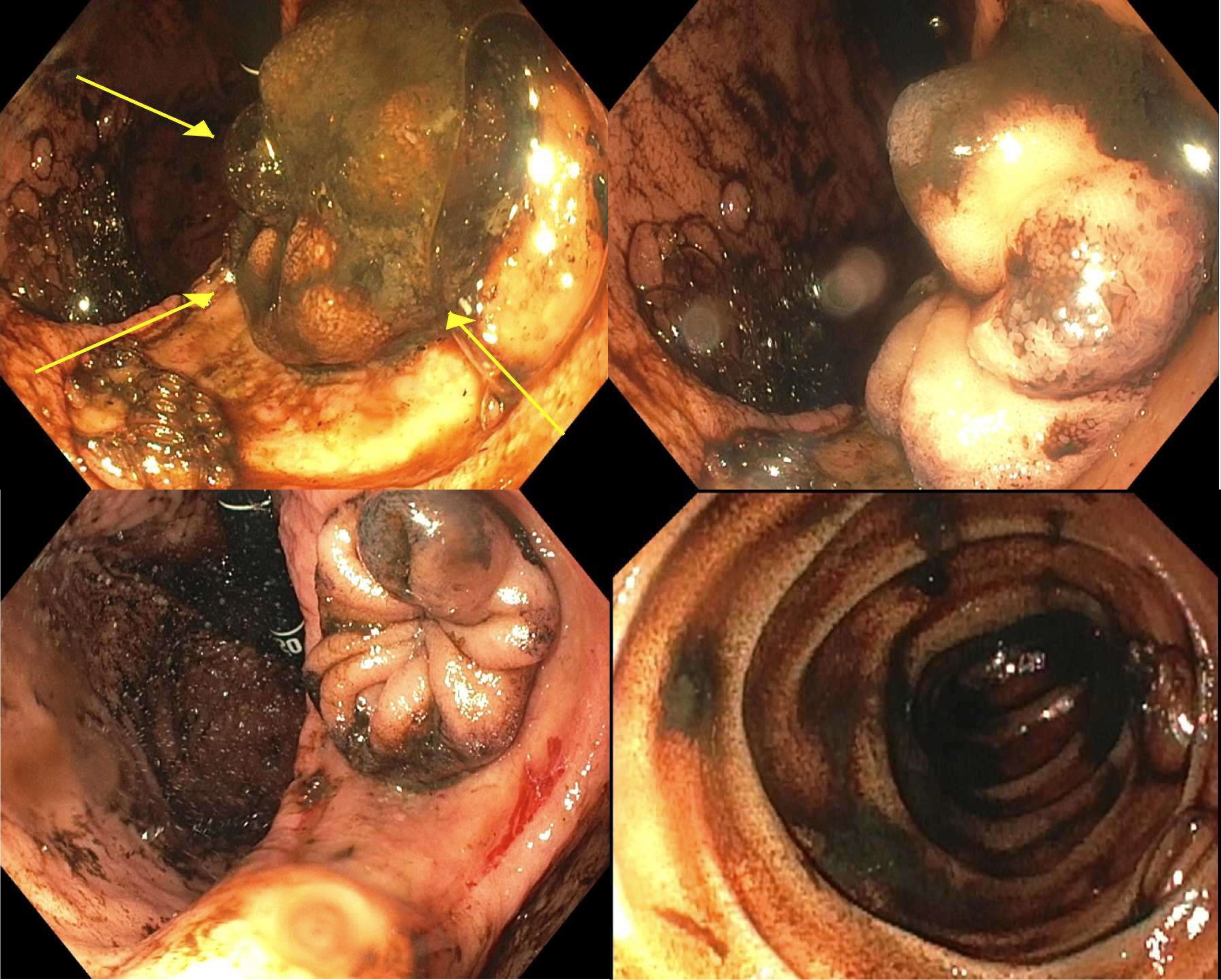
Figure: Figure 2. Images from the patient’s repeat inpatient EGD show an 8 cm clean-based ulcer bed with small bowel mucosa protruding through a fistula. Note the abundance of hematin in the setting of bleeding after starting anticoagulation. The image on the bottom right shows small bowel which was visualized upon traversing through the protruding small bowel mucosa and fistula tract.
Disclosures:
Jerry Kong indicated no relevant financial relationships.
Lindsey Sattler indicated no relevant financial relationships.
Courtney Balgobin indicated no relevant financial relationships.
Jerry Kong, BS1, Lindsey Sattler, MD2, Courtney Balgobin, MD1. P0962 - A Gastroenteric Fistulation Preventing Peptic Ulcer Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
