Sunday Poster Session
Category: GI Bleeding
P0961 - Presumed Dieulafoy, Proven Hemangioma: A Rare Cause of Refractory Small Bowel Bleeding Requiring Surgical Resection
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Simran Agarwal, MS, MA (she/her/hers)
Ross University School of Medicine
Boynton Beach, FL
Presenting Author(s)
Award: ACG Presidential Poster Award
Simran Agarwal, MS, MA1, Rujul Patel, BS1, Neelam Khetpal, MD2, Asad Ur Rahman, MD2, David J. Restrepo, MD2, Fernando Castro, MD2
1Ross University School of Medicine, Miramar, FL; 2Cleveland Clinic Florida, Weston, FL
Introduction: Dieulafoy lesions are rare vascular malformations that account for 1 to 2 percent of gastrointestinal bleeds and up to 6.5 percent of non-variceal upper gastrointestinal hemorrhages. They are composed of large-caliber submucosal arteries that erode through the mucosa, resulting in acute and often massive bleeding. Endoscopic therapies such as clipping, band ligation, or thermal coagulation are typically effective, with surgery required in fewer than 6 percent of cases. In patients with recurrent bleeding despite appropriate endoscopic treatment, other vascular causes such as submucosal hemangiomas should be considered.
Case Description/
Methods: A 62-year-old male with metastatic bladder cancer, chronic kidney disease, and a right lower extremity deep vein thrombosis diagnosed on December 14, 2024 (started on apixaban), presented on December 19, 2024, with melena, fatigue, and transfusion-dependent anemia. He received seven units of packed red blood cells over multiple admissions. Anticoagulation was held and an inferior vena cava filter was placed. Esophagogastroduodenoscopy revealed no overt source of bleeding and colonoscopy showed hematin in the terminal ileum. Capsule endoscopy demonstrated active bleeding at approximately 50% of the small bowel transit time, suggesting a jejunal or proximal ileal source. Double balloon enteroscopy (DBE) identified a presumed Dieulafoy lesion in the proximal ileum, managed with epinephrine injection, hemostatic clips, and tattooing. The patient was readmitted with recurrent melena. Repeat DBE failed due to looping. CT angiography and formal angiography were non-diagnostic. Laparoscopic-assisted intraoperative enteroscopy revealed active bleeding five centimeters distal to the tattooed site. A 20 cm segment of proximal ileum was resected. Final pathology confirmed a cavernous submucosal hemangioma.
Discussion: Small bowel hemangiomas account for approximately ten percent of benign small bowel tumors and are most commonly found in the jejunum or ileum. They appear submucosally as soft, violaceous lesions and are often missed on capsule endoscopy or imaging. Surgical resection is typically required. This case highlights the importance of maintaining a broad differential in obscure gastrointestinal bleeding and emphasizes the value of tattooing in accurately localizing lesions for targeted surgical treatment.
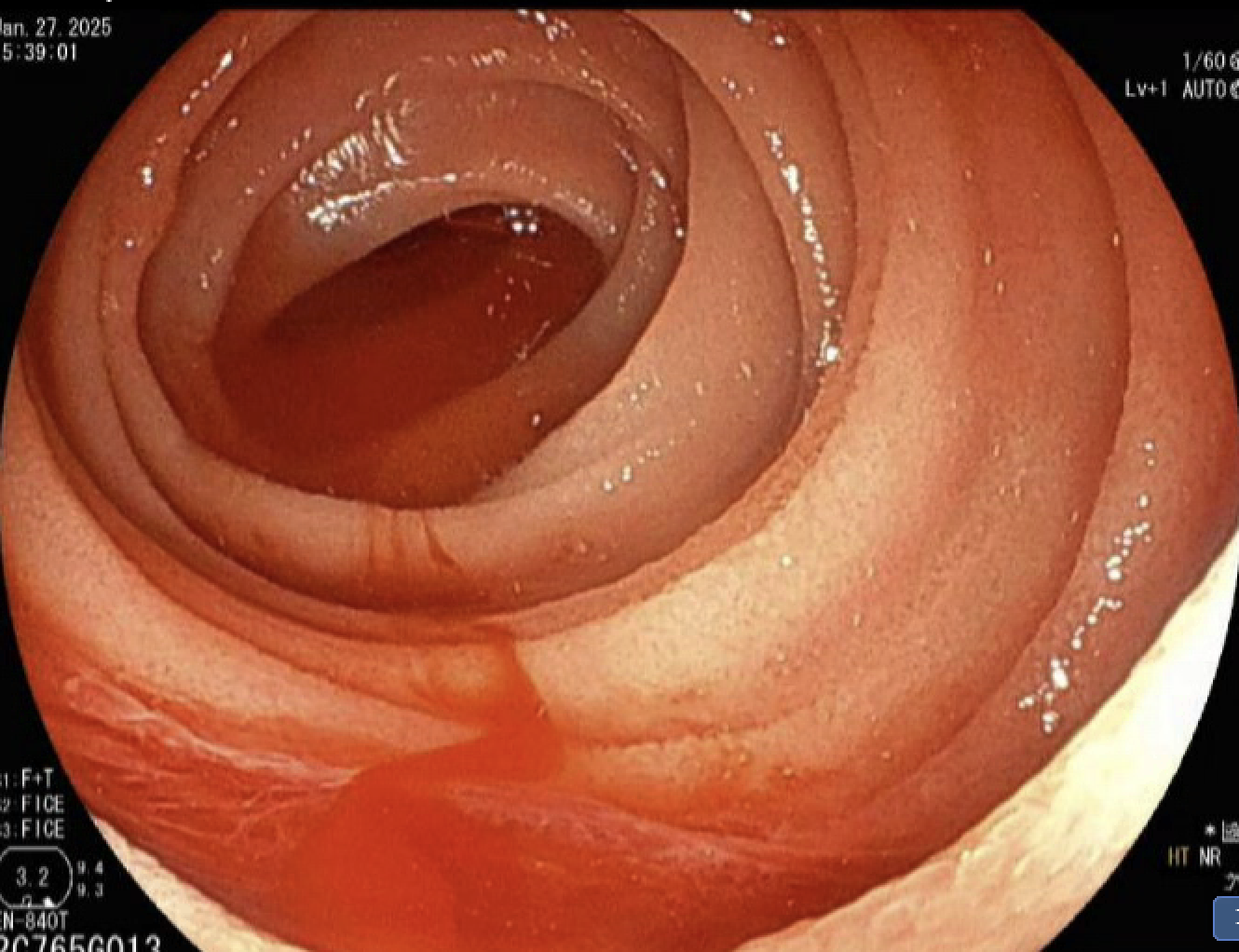
Figure: Double balloon enteroscopy image showing presumed Dieulafoy lesion in the proximal ileum, treated with hemostatic clip placement and tattoo marking.
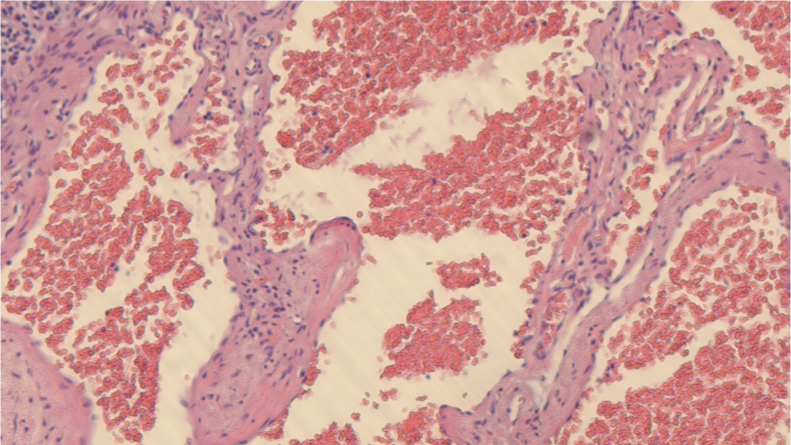
Figure: Histopathology image demonstrating cavernous submucosal hemangioma with dilated vascular spaces in the resected small bowel specimen (H&E stain).
Disclosures:
Simran Agarwal indicated no relevant financial relationships.
Rujul Patel indicated no relevant financial relationships.
Neelam Khetpal indicated no relevant financial relationships.
Asad Ur Rahman: Abbvie Inc – Speakers Bureau.
David Restrepo indicated no relevant financial relationships.
Fernando Castro indicated no relevant financial relationships.
Simran Agarwal, MS, MA1, Rujul Patel, BS1, Neelam Khetpal, MD2, Asad Ur Rahman, MD2, David J. Restrepo, MD2, Fernando Castro, MD2. P0961 - Presumed Dieulafoy, Proven Hemangioma: A Rare Cause of Refractory Small Bowel Bleeding Requiring Surgical Resection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Simran Agarwal, MS, MA1, Rujul Patel, BS1, Neelam Khetpal, MD2, Asad Ur Rahman, MD2, David J. Restrepo, MD2, Fernando Castro, MD2
1Ross University School of Medicine, Miramar, FL; 2Cleveland Clinic Florida, Weston, FL
Introduction: Dieulafoy lesions are rare vascular malformations that account for 1 to 2 percent of gastrointestinal bleeds and up to 6.5 percent of non-variceal upper gastrointestinal hemorrhages. They are composed of large-caliber submucosal arteries that erode through the mucosa, resulting in acute and often massive bleeding. Endoscopic therapies such as clipping, band ligation, or thermal coagulation are typically effective, with surgery required in fewer than 6 percent of cases. In patients with recurrent bleeding despite appropriate endoscopic treatment, other vascular causes such as submucosal hemangiomas should be considered.
Case Description/
Methods: A 62-year-old male with metastatic bladder cancer, chronic kidney disease, and a right lower extremity deep vein thrombosis diagnosed on December 14, 2024 (started on apixaban), presented on December 19, 2024, with melena, fatigue, and transfusion-dependent anemia. He received seven units of packed red blood cells over multiple admissions. Anticoagulation was held and an inferior vena cava filter was placed. Esophagogastroduodenoscopy revealed no overt source of bleeding and colonoscopy showed hematin in the terminal ileum. Capsule endoscopy demonstrated active bleeding at approximately 50% of the small bowel transit time, suggesting a jejunal or proximal ileal source. Double balloon enteroscopy (DBE) identified a presumed Dieulafoy lesion in the proximal ileum, managed with epinephrine injection, hemostatic clips, and tattooing. The patient was readmitted with recurrent melena. Repeat DBE failed due to looping. CT angiography and formal angiography were non-diagnostic. Laparoscopic-assisted intraoperative enteroscopy revealed active bleeding five centimeters distal to the tattooed site. A 20 cm segment of proximal ileum was resected. Final pathology confirmed a cavernous submucosal hemangioma.
Discussion: Small bowel hemangiomas account for approximately ten percent of benign small bowel tumors and are most commonly found in the jejunum or ileum. They appear submucosally as soft, violaceous lesions and are often missed on capsule endoscopy or imaging. Surgical resection is typically required. This case highlights the importance of maintaining a broad differential in obscure gastrointestinal bleeding and emphasizes the value of tattooing in accurately localizing lesions for targeted surgical treatment.
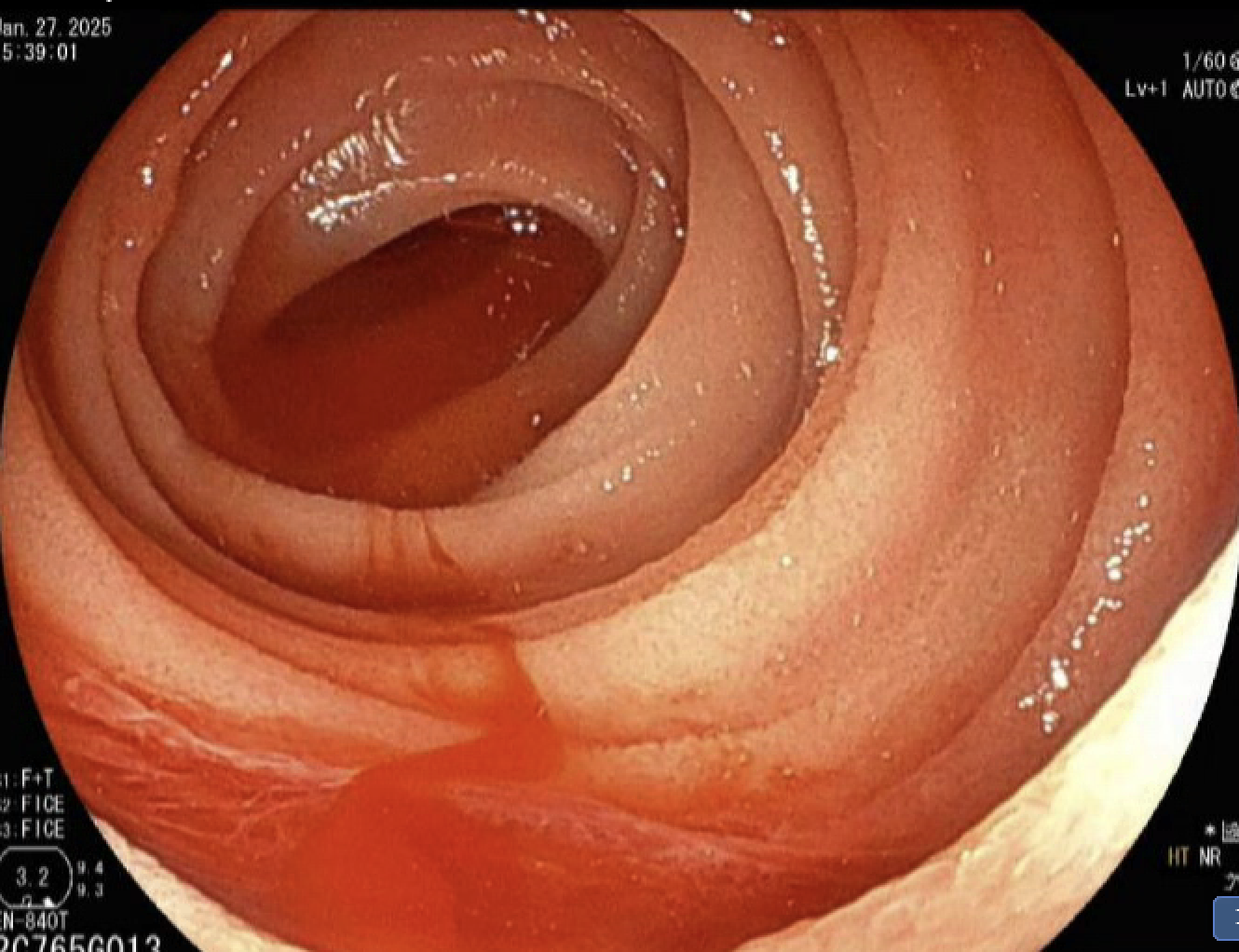
Figure: Double balloon enteroscopy image showing presumed Dieulafoy lesion in the proximal ileum, treated with hemostatic clip placement and tattoo marking.
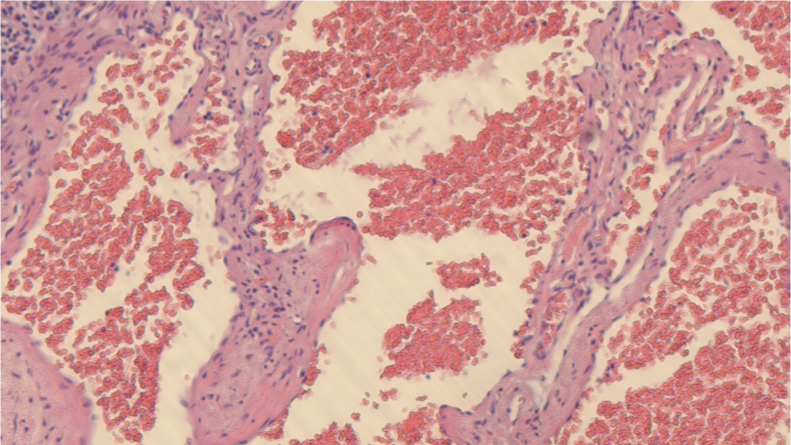
Figure: Histopathology image demonstrating cavernous submucosal hemangioma with dilated vascular spaces in the resected small bowel specimen (H&E stain).
Disclosures:
Simran Agarwal indicated no relevant financial relationships.
Rujul Patel indicated no relevant financial relationships.
Neelam Khetpal indicated no relevant financial relationships.
Asad Ur Rahman: Abbvie Inc – Speakers Bureau.
David Restrepo indicated no relevant financial relationships.
Fernando Castro indicated no relevant financial relationships.
Simran Agarwal, MS, MA1, Rujul Patel, BS1, Neelam Khetpal, MD2, Asad Ur Rahman, MD2, David J. Restrepo, MD2, Fernando Castro, MD2. P0961 - Presumed Dieulafoy, Proven Hemangioma: A Rare Cause of Refractory Small Bowel Bleeding Requiring Surgical Resection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

