Sunday Poster Session
Category: GI Bleeding
P0955 - A Pulsating Ulcer Unmasks an Atrio-Gastric Conduit Fistula: A Remote and Rare Complication of Esophagectomy and Chemoradiation for Esophageal Adenocarcinoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Garvita Singhal, MD (she/her/hers)
Tucson Medical Center (TMC)
Tucson, AZ
Presenting Author(s)
Award: ACG Presidential Poster Award
Garvita Singhal, MD1, Rizwan Safdar, MD2
1Tucson Medical Center (TMC), Tucson, AZ; 2Carondelet Health Network, Tucson, Arizona, Tucson, AZ
Introduction: Atrio-gastric conduit fistula (AGCF) is an exceedingly rare and often fatal complication following esophagectomy with gastric pull-up, particularly in patients with prior chemoradiation or tumor recurrence. We present a striking case emphasizing the importance of recognizing atypical endoscopic findings and initiating timely, life-saving intervention.
Case Description/
Methods: An 84-year-old man with a history of mechanical aortic valve replacement, atrial fibrillation, and stage IV esophageal adenocarcinoma (status post transhiatal esophagectomy with gastric pull-up and adjuvant chemoradiation two years earlier) presented with recurrent hematochezia and syncope. A prior colonoscopy was unrevealing. On admission, he was hypotensive and subsequently required ICU care. Upper endoscopy revealed a large gastric ulcer with a visible vessel that changed in depth and appearance with respiration and pulsation, located in the intrathoracic gastric conduit. Concern for an atypical vascular lesion prompted emergent CTA, which demonstrated a nipple-like outpouching of the left atrium projecting into the gastric lumen, consistent with AGCF. Given the near-certain lethality without intervention and a perioperative mortality risk >30%, the patient consented to surgery. He underwent left thoracotomy with cardiopulmonary bypass-assisted repair of the atrium and gastric conduit, along with interposition of serratus anterior and latissimus dorsi muscle flaps. A direct fistula was identified and repaired on both sides, and a pedicled muscle flap was placed to prevent recurrence. Despite a complicated postoperative course, the patient recovered successfully.
Discussion: AGCF is a rare, delayed complication of esophagectomy, particularly in patients with prior chemoradiation or malignancy recurrence. The posterior mediastinal placement of the gastric conduit in transhiatal reconstructions makes fistulization to the heart exceptionally uncommon. In this case, the fistula developed distal to the anastomosis, likely due to radiation-induced tissue injury. Clinically, AGCF may present with hematemesis, hematochezia, or sentinel bleeding followed by hemodynamic collapse. The finding of a pulsating ulcer synchronous with the heartbeat was subtle but critical. Endoscopic cautery would likely have been fatal and judicious decision making is important in such cases. Early recognition and surgical repair are essential, as mortality exceeds 95% without treatment.
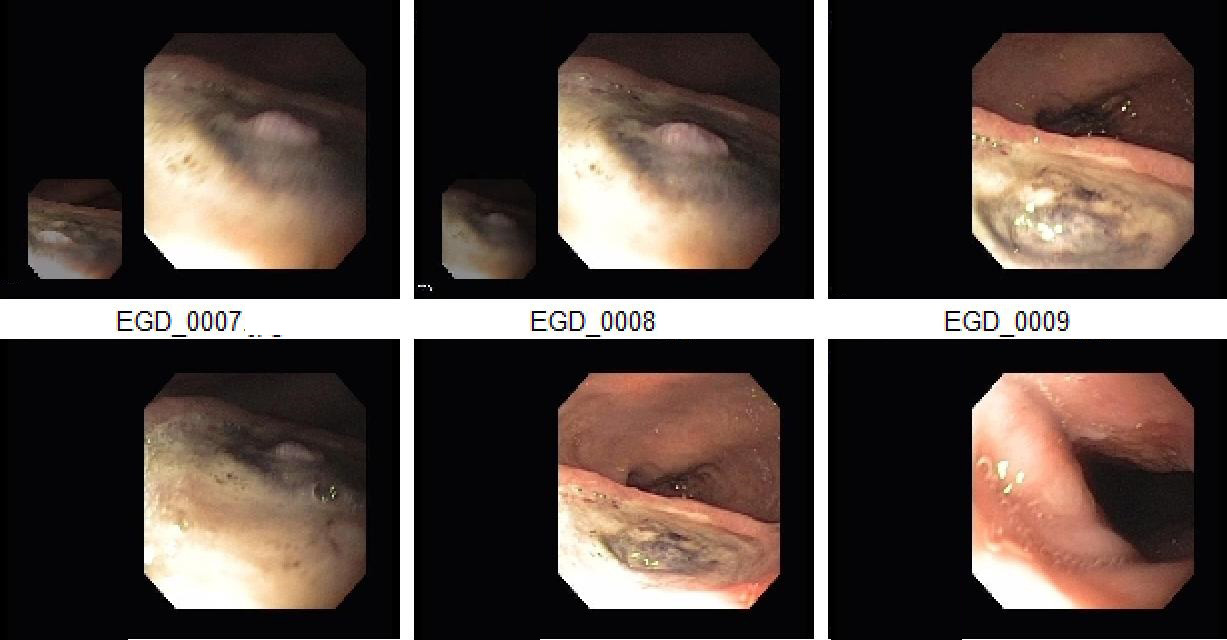
Figure: Image 1: Endoscopic view of the gastric ulcer base revealing a nipple-like protrusion (arrow). The protrusion exhibited dynamic movement—with respiration and pulsating synchronously with the cardiac cycle—raising concern for underlying vascular communication.
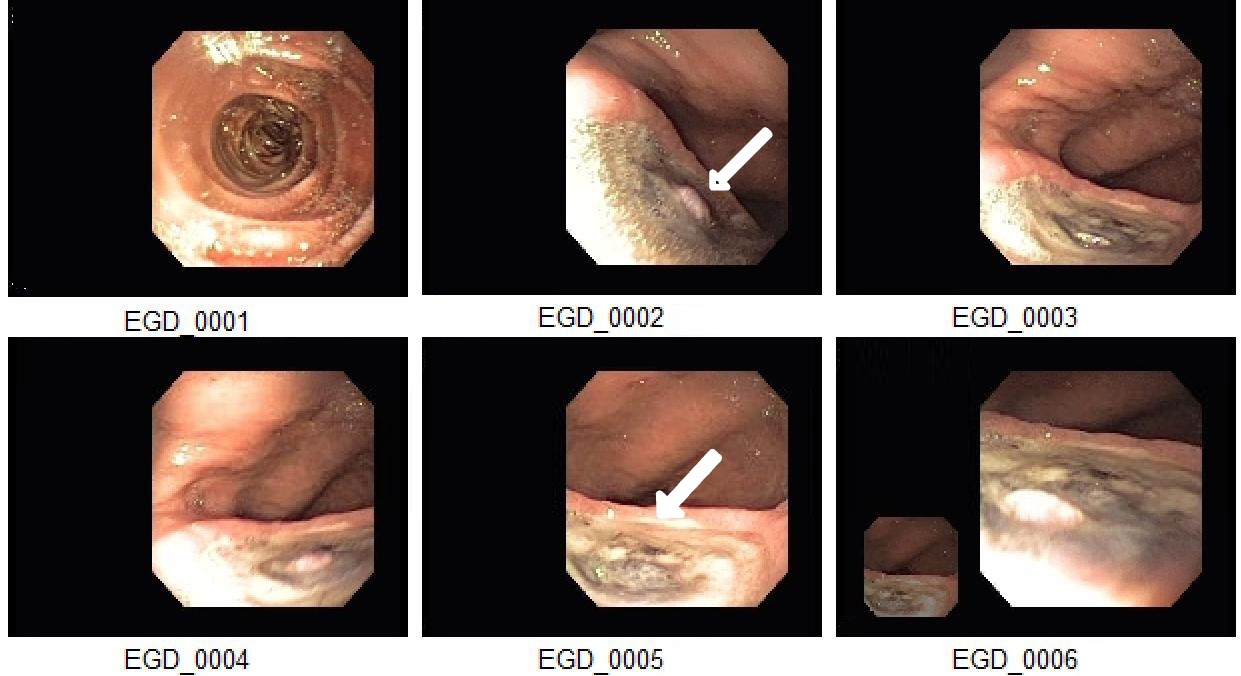
Figure: Image 2: Additional endoscopic images demonstrating the same findings as previously shown.
Disclosures:
Garvita Singhal indicated no relevant financial relationships.
Rizwan Safdar indicated no relevant financial relationships.
Garvita Singhal, MD1, Rizwan Safdar, MD2. P0955 - A Pulsating Ulcer Unmasks an Atrio-Gastric Conduit Fistula: A Remote and Rare Complication of Esophagectomy and Chemoradiation for Esophageal Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Garvita Singhal, MD1, Rizwan Safdar, MD2
1Tucson Medical Center (TMC), Tucson, AZ; 2Carondelet Health Network, Tucson, Arizona, Tucson, AZ
Introduction: Atrio-gastric conduit fistula (AGCF) is an exceedingly rare and often fatal complication following esophagectomy with gastric pull-up, particularly in patients with prior chemoradiation or tumor recurrence. We present a striking case emphasizing the importance of recognizing atypical endoscopic findings and initiating timely, life-saving intervention.
Case Description/
Methods: An 84-year-old man with a history of mechanical aortic valve replacement, atrial fibrillation, and stage IV esophageal adenocarcinoma (status post transhiatal esophagectomy with gastric pull-up and adjuvant chemoradiation two years earlier) presented with recurrent hematochezia and syncope. A prior colonoscopy was unrevealing. On admission, he was hypotensive and subsequently required ICU care. Upper endoscopy revealed a large gastric ulcer with a visible vessel that changed in depth and appearance with respiration and pulsation, located in the intrathoracic gastric conduit. Concern for an atypical vascular lesion prompted emergent CTA, which demonstrated a nipple-like outpouching of the left atrium projecting into the gastric lumen, consistent with AGCF. Given the near-certain lethality without intervention and a perioperative mortality risk >30%, the patient consented to surgery. He underwent left thoracotomy with cardiopulmonary bypass-assisted repair of the atrium and gastric conduit, along with interposition of serratus anterior and latissimus dorsi muscle flaps. A direct fistula was identified and repaired on both sides, and a pedicled muscle flap was placed to prevent recurrence. Despite a complicated postoperative course, the patient recovered successfully.
Discussion: AGCF is a rare, delayed complication of esophagectomy, particularly in patients with prior chemoradiation or malignancy recurrence. The posterior mediastinal placement of the gastric conduit in transhiatal reconstructions makes fistulization to the heart exceptionally uncommon. In this case, the fistula developed distal to the anastomosis, likely due to radiation-induced tissue injury. Clinically, AGCF may present with hematemesis, hematochezia, or sentinel bleeding followed by hemodynamic collapse. The finding of a pulsating ulcer synchronous with the heartbeat was subtle but critical. Endoscopic cautery would likely have been fatal and judicious decision making is important in such cases. Early recognition and surgical repair are essential, as mortality exceeds 95% without treatment.
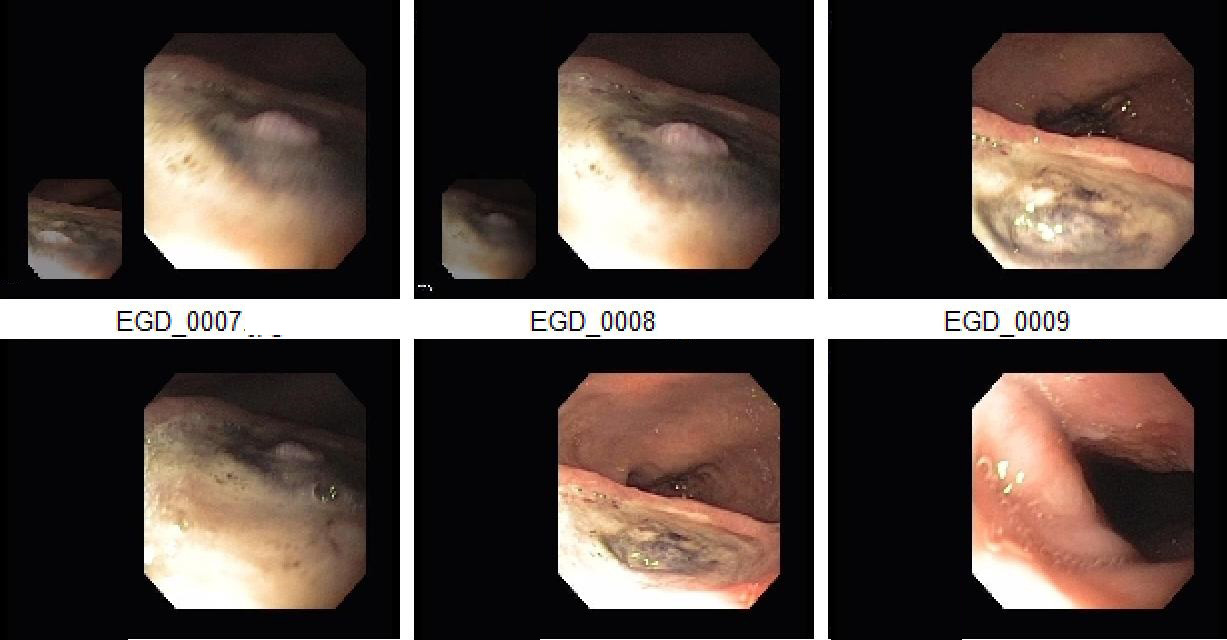
Figure: Image 1: Endoscopic view of the gastric ulcer base revealing a nipple-like protrusion (arrow). The protrusion exhibited dynamic movement—with respiration and pulsating synchronously with the cardiac cycle—raising concern for underlying vascular communication.
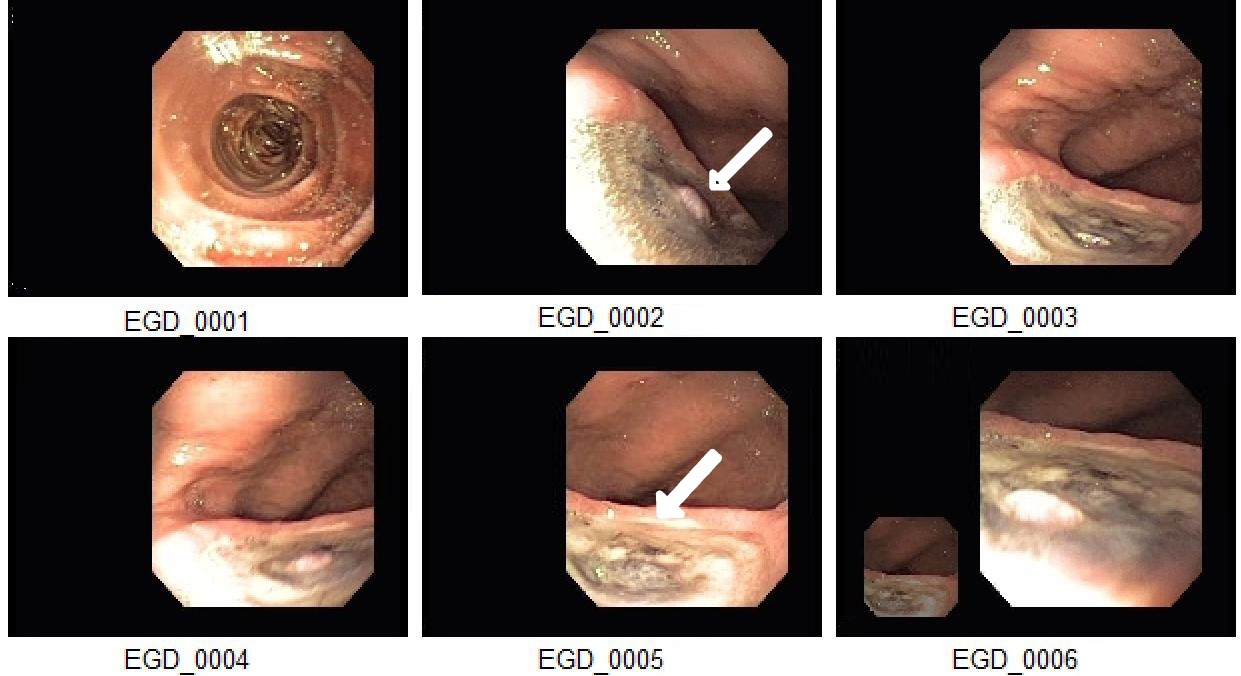
Figure: Image 2: Additional endoscopic images demonstrating the same findings as previously shown.
Disclosures:
Garvita Singhal indicated no relevant financial relationships.
Rizwan Safdar indicated no relevant financial relationships.
Garvita Singhal, MD1, Rizwan Safdar, MD2. P0955 - A Pulsating Ulcer Unmasks an Atrio-Gastric Conduit Fistula: A Remote and Rare Complication of Esophagectomy and Chemoradiation for Esophageal Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


