Sunday Poster Session
Category: GI Bleeding
P0954 - A Rare Cause of Gastrointestinal Bleeding: Endoscopic Resection of a Large Brunner Gland Hamartoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Alexander F. Siegel, MD
Creighton University Medical Center
Omaha, NE
Presenting Author(s)
Alexander F. Siegel, MD1, Shalini S.. Jain, MD2
1Creighton University Medical Center, Omaha, NE; 2Creighton University, Omaha, NE
Introduction: Brunner gland hamartomas (BGH) are rare, mostly benign tumors that arise from Brunner's glands located in the submucosa of the duodenum (1). They are often discovered incidentally during upper endoscopy (EGD), as most lesions are relatively small (ranging from 0.2 - 2 cm) and asymptomatic (2). However, larger lesions can cause more complications such as gastrointestinal bleeding (GIB), partial bowel obstruction or anemia. If involvement of the Ampulla of Vater, patients can present with obstructive jaundice, pancreatitis and even biliary tract fistula.
Case Description/
Methods: A 44 year old male with past medical history of an asymptomatic hiatal hernia presented with one week of melena. He was otherwise asymptomatic with no prior GIB or NSAID use. Vitals stable on admission. Initial labs revealed BUN 32 and hemoglobin (Hb) of 12.8 g/dL, which subsequently dropped to 8.6 g/dL within 48 hours. He had a benign abdominal exam. CT angiogram of the abdomen was negative for active bleeding.
EGD revealed a 4.0 x 3.5 x 2.2 cm pedunculated, fibrovascular polyp with an ulcerated tip in the second part of the duodenum. The polyp was successfully removed by the advanced endoscopist using an ENDOLOOP snare mucosal resection, and three hemostatic clips were placed to ensure hemostasis. The polyp was retrieved intact via Roth net. The patient tolerated the procedure well with improvement of anemia prior to discharge. Histopathologic examination was consistent with Brunner gland hamartoma.
Discussion: Brunner glands play an important role in neutralizing stomach acid. They aid in digestion by producing a mucus-rich secretion containing bicarbonate, which helps activate pancreatic digestive enzymes. Disorganized growth of these glands can lead to hyperplasia eventually resulting in large hamartoma formation. Risk factors of BGH are not well defined. Case reports have identified associations between BGH and H. pylori infection (3) and more non-specific chronic duodenal mucosa inflammation leading to metaplasia (4). In a literature review, 2.1% of Brunner’s gland hyperplasia lesions evaluated had dysplasia and 0.3% with invasive carcinoma (2). Therefore, although rare, removal via polypectomy of these hamartomas is crucial, but can often be endoscopically challenging. Surgical resection has been utilized in difficult cases. Our case highlights the importance of keeping the differential diagnosis of GIB broad to include these rare findings like BGH, which can often lead to an endoscopically challenging case.

Figure: Resected BGH next to the specimen cup lid for size comparison.
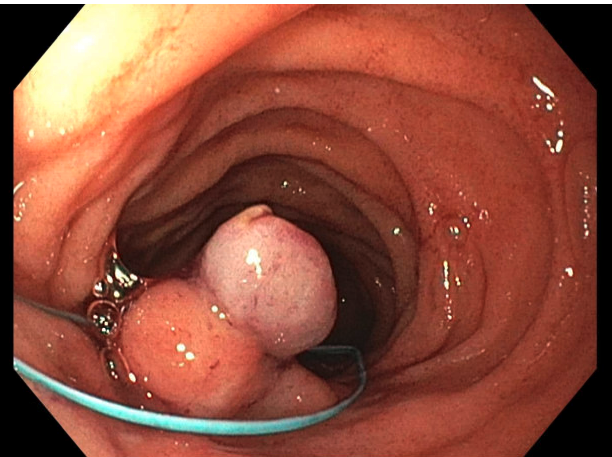
Figure: ENDOLOOP mucosal resection of the BGH.
Disclosures:
Alexander Siegel indicated no relevant financial relationships.
Shalini Jain indicated no relevant financial relationships.
Alexander F. Siegel, MD1, Shalini S.. Jain, MD2. P0954 - A Rare Cause of Gastrointestinal Bleeding: Endoscopic Resection of a Large Brunner Gland Hamartoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University Medical Center, Omaha, NE; 2Creighton University, Omaha, NE
Introduction: Brunner gland hamartomas (BGH) are rare, mostly benign tumors that arise from Brunner's glands located in the submucosa of the duodenum (1). They are often discovered incidentally during upper endoscopy (EGD), as most lesions are relatively small (ranging from 0.2 - 2 cm) and asymptomatic (2). However, larger lesions can cause more complications such as gastrointestinal bleeding (GIB), partial bowel obstruction or anemia. If involvement of the Ampulla of Vater, patients can present with obstructive jaundice, pancreatitis and even biliary tract fistula.
Case Description/
Methods: A 44 year old male with past medical history of an asymptomatic hiatal hernia presented with one week of melena. He was otherwise asymptomatic with no prior GIB or NSAID use. Vitals stable on admission. Initial labs revealed BUN 32 and hemoglobin (Hb) of 12.8 g/dL, which subsequently dropped to 8.6 g/dL within 48 hours. He had a benign abdominal exam. CT angiogram of the abdomen was negative for active bleeding.
EGD revealed a 4.0 x 3.5 x 2.2 cm pedunculated, fibrovascular polyp with an ulcerated tip in the second part of the duodenum. The polyp was successfully removed by the advanced endoscopist using an ENDOLOOP snare mucosal resection, and three hemostatic clips were placed to ensure hemostasis. The polyp was retrieved intact via Roth net. The patient tolerated the procedure well with improvement of anemia prior to discharge. Histopathologic examination was consistent with Brunner gland hamartoma.
Discussion: Brunner glands play an important role in neutralizing stomach acid. They aid in digestion by producing a mucus-rich secretion containing bicarbonate, which helps activate pancreatic digestive enzymes. Disorganized growth of these glands can lead to hyperplasia eventually resulting in large hamartoma formation. Risk factors of BGH are not well defined. Case reports have identified associations between BGH and H. pylori infection (3) and more non-specific chronic duodenal mucosa inflammation leading to metaplasia (4). In a literature review, 2.1% of Brunner’s gland hyperplasia lesions evaluated had dysplasia and 0.3% with invasive carcinoma (2). Therefore, although rare, removal via polypectomy of these hamartomas is crucial, but can often be endoscopically challenging. Surgical resection has been utilized in difficult cases. Our case highlights the importance of keeping the differential diagnosis of GIB broad to include these rare findings like BGH, which can often lead to an endoscopically challenging case.

Figure: Resected BGH next to the specimen cup lid for size comparison.
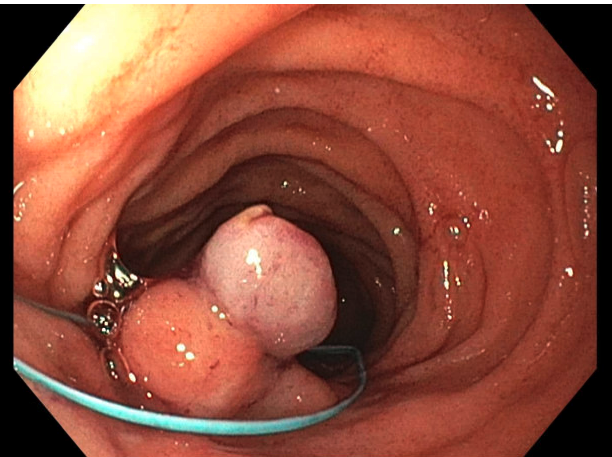
Figure: ENDOLOOP mucosal resection of the BGH.
Disclosures:
Alexander Siegel indicated no relevant financial relationships.
Shalini Jain indicated no relevant financial relationships.
Alexander F. Siegel, MD1, Shalini S.. Jain, MD2. P0954 - A Rare Cause of Gastrointestinal Bleeding: Endoscopic Resection of a Large Brunner Gland Hamartoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
