Sunday Poster Session
Category: GI Bleeding
P0948 - Multifactorial Duodenal Hemorrhage in a Patient With Diffuse Large B-Cell Lymphoma: Navigating Steroid-Induced Ulceration and Anticoagulation in the Setting of Sepsis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Deepak Kumar, MBBS, MD (he/him/his)
Northwell Health
Port Jefferson, NY
Presenting Author(s)
Deepak Kumar, MBBS, MD1, Toby Bradford, DO2, Sunny Kumar, MD3, Janta Devi Ukrani, MBBS, MD1, Ramona Rajapakse, MD, FACG4
1Northwell Health, Port Jefferson, NY; 2Northwell at MATHER Hospital, Port Jefferson, NY; 3Wright Center for Graduate Medical Education, Scranton, PA; 4Mather Hospital, Northwell Health, Port Jefferson, NY
Introduction: Upper gastrointestinal bleeding (UGIB) is a potentially life-threatening emergency, especially in patients with complex comorbidities such as malignancy and venous thromboembolism. Although 80% of UGIB cases resolve with supportive care, patients with metastatic cancer, hemodynamic instability, or inpatient onset carry significantly higher mortality. We present a challenging case of UGIB in a patient with diffuse large B-cell lymphoma (DLBCL) and concurrent pulmonary embolism (PE), highlighting the complexities of management in the setting of competing risks.
Case Description/
Methods: A 74-year-old man with newly diagnosed DLBCL presented following a syncopal episode. He had recently initiated POLA-R-CHP chemotherapy. Imaging revealed a segmental pulmonary embolism and left soleal DVT. He was started on intravenous heparin. Within 72 hours, he developed melena and acute anemia (hemoglobin dropped from 9.0 to 5.6 g/dL). Heparin was discontinued, and a pantoprazole infusion was initiated. CT angiography revealed duodenal bleeding. The patient progressed to hemorrhagic shock requiring vasopressors and was concurrently septic, likely due to pneumonia. After stabilization with multiple transfusions (4 PRBCs, 1 FFP, 1 platelet unit), an esophagogastroduodenoscopy (EGD) on hospital day five revealed seven Forrest class III duodenal ulcers with nodularity, but no active bleeding. Given prior hemorrhagic shock, poor prognostic factors, and anticipated need for anticoagulation, PuraStat® topical hemostatic gel was applied generously. Biopsies were deferred to avoid provoking further bleeding. CT imaging confirmed duodenal ulceration without mass or obstruction. H. pylori infection and gastrinoma were considered but deemed unlikely based on clinical context. Anticoagulation with apixaban 5 mg BID was resumed cautiously. Hemoglobin remained stable with no recurrent bleeding. An IVC filter was considered given rebleeding risk.
Discussion: This case underscores the clinical tension between thrombotic risk and gastrointestinal bleeding in patients with hematologic malignancies. Steroid use, chemotherapy, sepsis, and anticoagulation likely contributed to multifactorial ulcer formation. Conservative endoscopic therapy with PuraStat®, PPI infusion, transfusion support, and delayed reintroduction of anticoagulation enabled clinical stability. Multidisciplinary coordination among gastroenterology, hematology, and critical care was crucial for optimal outcome in this high-risk, medically complex patient.
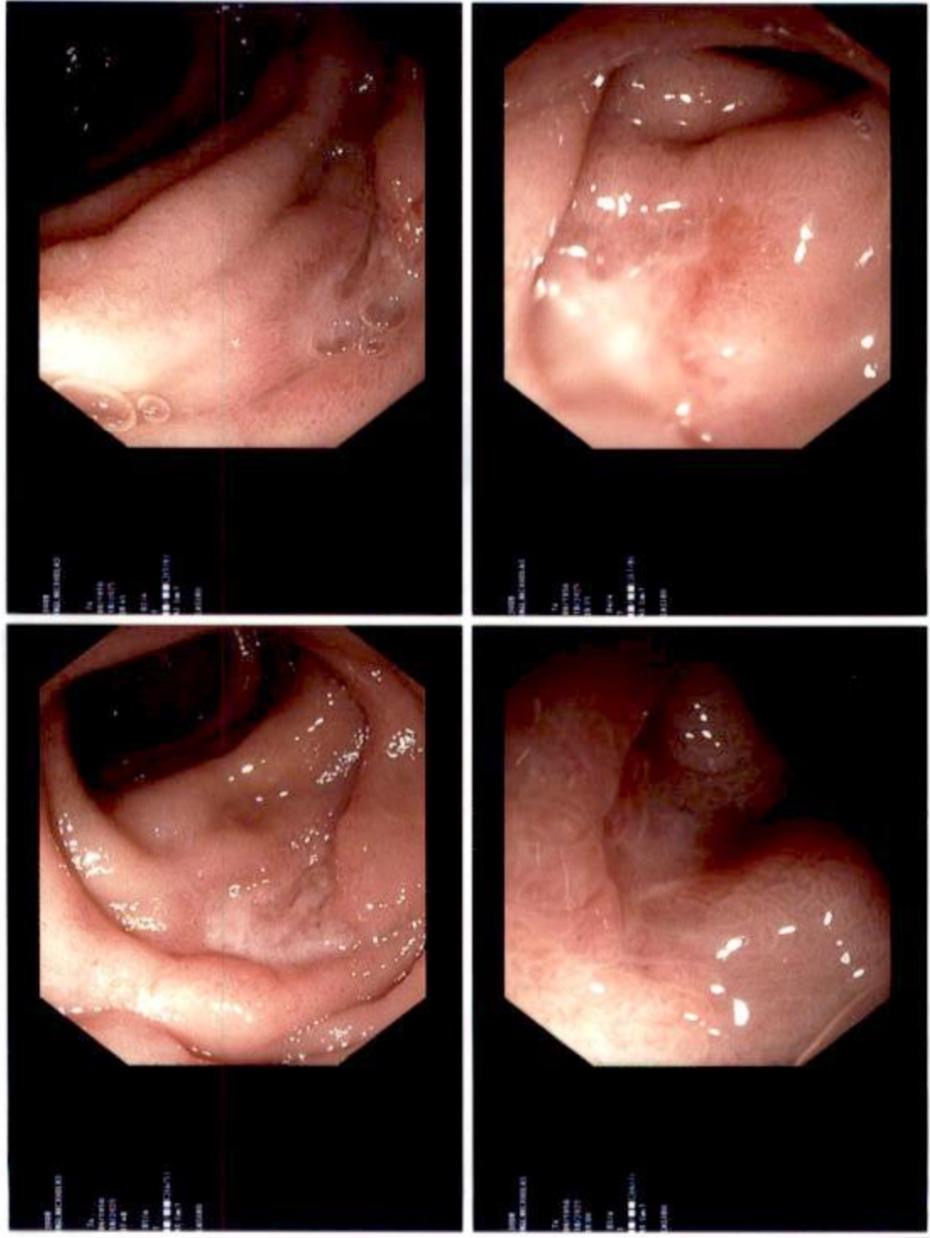
Figure: Forrest class III duodenal ulcers with nodularity, but no active bleeding
Disclosures:
Deepak Kumar indicated no relevant financial relationships.
Toby Bradford indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Janta Devi Ukrani indicated no relevant financial relationships.
Ramona Rajapakse indicated no relevant financial relationships.
Deepak Kumar, MBBS, MD1, Toby Bradford, DO2, Sunny Kumar, MD3, Janta Devi Ukrani, MBBS, MD1, Ramona Rajapakse, MD, FACG4. P0948 - Multifactorial Duodenal Hemorrhage in a Patient With Diffuse Large B-Cell Lymphoma: Navigating Steroid-Induced Ulceration and Anticoagulation in the Setting of Sepsis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northwell Health, Port Jefferson, NY; 2Northwell at MATHER Hospital, Port Jefferson, NY; 3Wright Center for Graduate Medical Education, Scranton, PA; 4Mather Hospital, Northwell Health, Port Jefferson, NY
Introduction: Upper gastrointestinal bleeding (UGIB) is a potentially life-threatening emergency, especially in patients with complex comorbidities such as malignancy and venous thromboembolism. Although 80% of UGIB cases resolve with supportive care, patients with metastatic cancer, hemodynamic instability, or inpatient onset carry significantly higher mortality. We present a challenging case of UGIB in a patient with diffuse large B-cell lymphoma (DLBCL) and concurrent pulmonary embolism (PE), highlighting the complexities of management in the setting of competing risks.
Case Description/
Methods: A 74-year-old man with newly diagnosed DLBCL presented following a syncopal episode. He had recently initiated POLA-R-CHP chemotherapy. Imaging revealed a segmental pulmonary embolism and left soleal DVT. He was started on intravenous heparin. Within 72 hours, he developed melena and acute anemia (hemoglobin dropped from 9.0 to 5.6 g/dL). Heparin was discontinued, and a pantoprazole infusion was initiated. CT angiography revealed duodenal bleeding. The patient progressed to hemorrhagic shock requiring vasopressors and was concurrently septic, likely due to pneumonia. After stabilization with multiple transfusions (4 PRBCs, 1 FFP, 1 platelet unit), an esophagogastroduodenoscopy (EGD) on hospital day five revealed seven Forrest class III duodenal ulcers with nodularity, but no active bleeding. Given prior hemorrhagic shock, poor prognostic factors, and anticipated need for anticoagulation, PuraStat® topical hemostatic gel was applied generously. Biopsies were deferred to avoid provoking further bleeding. CT imaging confirmed duodenal ulceration without mass or obstruction. H. pylori infection and gastrinoma were considered but deemed unlikely based on clinical context. Anticoagulation with apixaban 5 mg BID was resumed cautiously. Hemoglobin remained stable with no recurrent bleeding. An IVC filter was considered given rebleeding risk.
Discussion: This case underscores the clinical tension between thrombotic risk and gastrointestinal bleeding in patients with hematologic malignancies. Steroid use, chemotherapy, sepsis, and anticoagulation likely contributed to multifactorial ulcer formation. Conservative endoscopic therapy with PuraStat®, PPI infusion, transfusion support, and delayed reintroduction of anticoagulation enabled clinical stability. Multidisciplinary coordination among gastroenterology, hematology, and critical care was crucial for optimal outcome in this high-risk, medically complex patient.
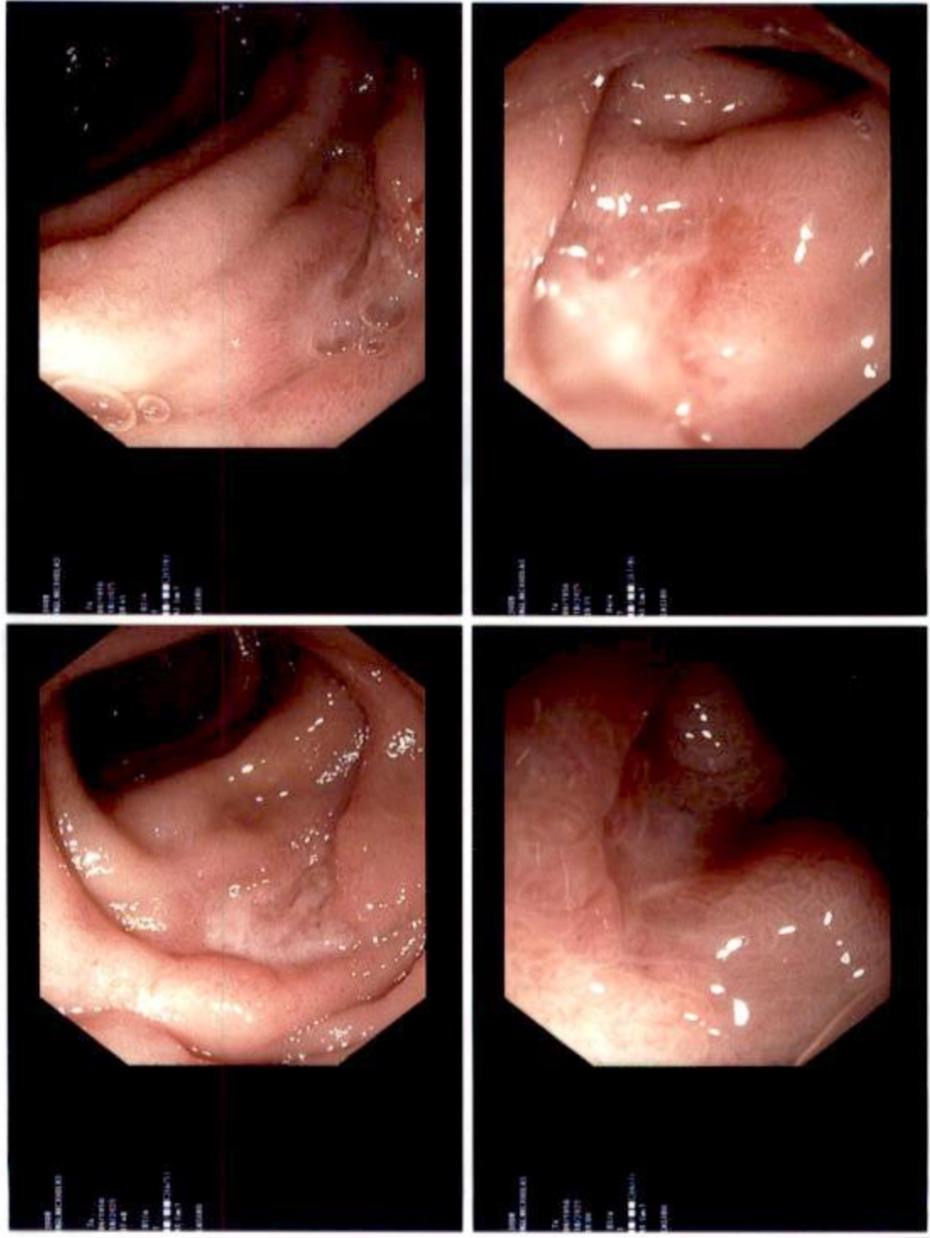
Figure: Forrest class III duodenal ulcers with nodularity, but no active bleeding
Disclosures:
Deepak Kumar indicated no relevant financial relationships.
Toby Bradford indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Janta Devi Ukrani indicated no relevant financial relationships.
Ramona Rajapakse indicated no relevant financial relationships.
Deepak Kumar, MBBS, MD1, Toby Bradford, DO2, Sunny Kumar, MD3, Janta Devi Ukrani, MBBS, MD1, Ramona Rajapakse, MD, FACG4. P0948 - Multifactorial Duodenal Hemorrhage in a Patient With Diffuse Large B-Cell Lymphoma: Navigating Steroid-Induced Ulceration and Anticoagulation in the Setting of Sepsis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
