Sunday Poster Session
Category: GI Bleeding
P0945 - Caught Red-Handed: Congo Red Unmasks Culprit in Gastrointestinal Bleed
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Claire C. Russell, DO (she/her/hers)
McLaren Greater Lansing Hospital
Lansing, MI
Presenting Author(s)
Claire C. Russell, DO1, Ali Rida, MD1, Caleb Glover, DO1, Edward Cay, DO2, Eric Nguyen, MD1, John Walling, DO1
1McLaren Greater Lansing Hospital, Lansing, MI; 2McLaren Greater Lansing, Lansing, MI
Introduction: Immunoglobulin light chain (AL) amyloidosis is characterized by plasma cell dyscrasia causing misfolded protein deposition. AL is the most common subtype of amyloid. Gastrointestinal (GI) involvement is less common in AL amyloidosis, affecting 8 percent of patients. Nonspecific presenting factors may lead to difficulty of diagnosis. Common symptoms include diarrhea, malabsorption, and obstruction. Bleeding presents in 25-45 percent of patients and can be secondary to ischemia or vascular friability. This case highlights the need for a broad differential for GI bleed evaluation.
Case Description/
Methods: A 65 year old female with past medical history pertinent for stage IV AL lambda type cardiac, renal amyloidosis, and immunoglobulin A (IgA) lambda multiple myeloma stage II, who presented for hematochezia for several hours. Patient hemoglobin 9.6g/dL on presentation. CT angiography evidenced moderate wall thickening in the lower rectum and increased fluid content in the left colon. Colonoscopy on hospital day two demonstrated an adherent clot without active bleeding 22-45 cm from anal verge. Remainder of procedure completed without complication. The patient was hemodynamically stable, tolerated diet, and denied further hematochezia after the procedure; four days after colonoscopy, the patient experienced large volume hematochezia, with hemoglobin downtrend to 7.9g/dL. Repeat colonoscopy completed successfully and demonstrated sigmoid ulceration where clot was seen on prior colonoscopy, biopsies were taken. Initial pathologic evaluation demonstrated ulcerated granulation tissue, suggestive of mucosal injury without evidence of chronicity or granulomas. Tissue examined under Congo Red stain was positive for amyloid deposition. Patient was discharged the following day with no further episodes of hematochezia.
Discussion: AL amyloid can cause structural and vascular fragility. Identifying amyloid as the cause of GI bleed can be difficult as patients may present without confirmed AL diagnosis. Histologic confirmation with Congo red staining and apple-green birefringence under polarized light is diagnostic gold standard, but not routinely performed. It is imperative to maintain a high index of suspicion for amyloidosis in patients presenting with unexplained GI bleeding, with known or suspected plasma cell disorders. Early recognition is crucial, due to high morbidity and mortality of GI bleeds in patients with systemic AL amyloid.
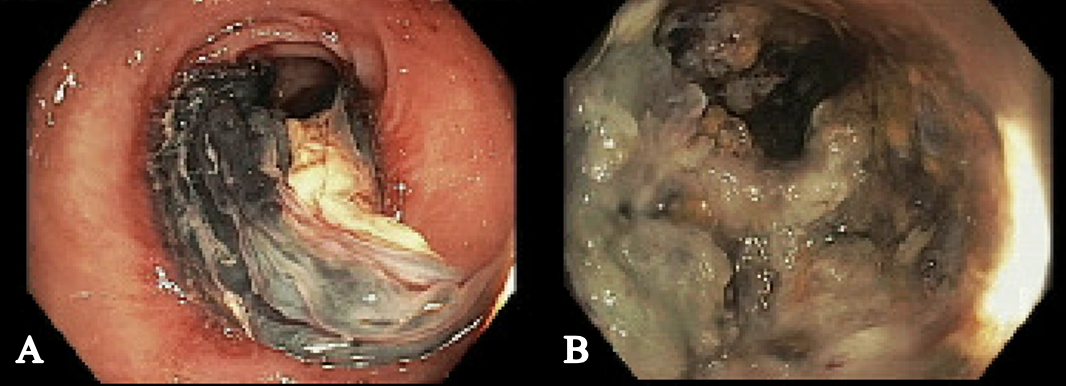
Figure: Figure 1: Pathology Slide of Colon Biopsy with Congo Red Staining
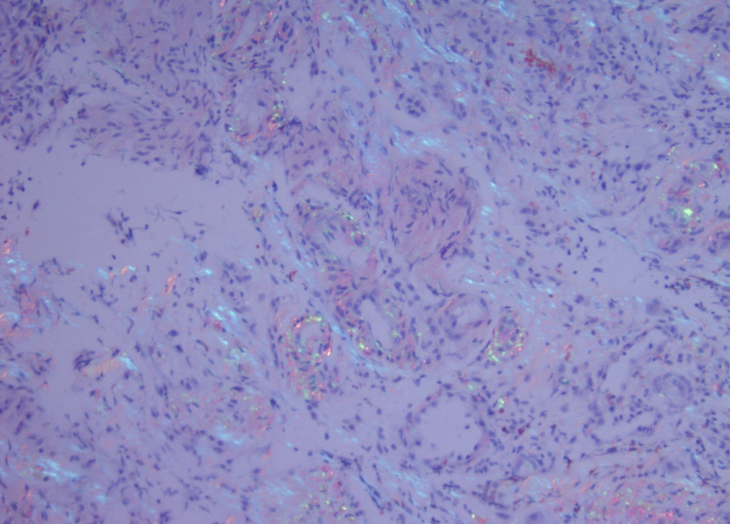
Figure: Figure 2: A: First Colonoscopy with Sigmoid Clot; B: Second Colonoscopy with Sigmoid Ulceration
Disclosures:
Claire Russell indicated no relevant financial relationships.
Ali Rida indicated no relevant financial relationships.
Caleb Glover indicated no relevant financial relationships.
Edward Cay indicated no relevant financial relationships.
Eric Nguyen indicated no relevant financial relationships.
John Walling indicated no relevant financial relationships.
Claire C. Russell, DO1, Ali Rida, MD1, Caleb Glover, DO1, Edward Cay, DO2, Eric Nguyen, MD1, John Walling, DO1. P0945 - Caught Red-Handed: Congo Red Unmasks Culprit in Gastrointestinal Bleed, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1McLaren Greater Lansing Hospital, Lansing, MI; 2McLaren Greater Lansing, Lansing, MI
Introduction: Immunoglobulin light chain (AL) amyloidosis is characterized by plasma cell dyscrasia causing misfolded protein deposition. AL is the most common subtype of amyloid. Gastrointestinal (GI) involvement is less common in AL amyloidosis, affecting 8 percent of patients. Nonspecific presenting factors may lead to difficulty of diagnosis. Common symptoms include diarrhea, malabsorption, and obstruction. Bleeding presents in 25-45 percent of patients and can be secondary to ischemia or vascular friability. This case highlights the need for a broad differential for GI bleed evaluation.
Case Description/
Methods: A 65 year old female with past medical history pertinent for stage IV AL lambda type cardiac, renal amyloidosis, and immunoglobulin A (IgA) lambda multiple myeloma stage II, who presented for hematochezia for several hours. Patient hemoglobin 9.6g/dL on presentation. CT angiography evidenced moderate wall thickening in the lower rectum and increased fluid content in the left colon. Colonoscopy on hospital day two demonstrated an adherent clot without active bleeding 22-45 cm from anal verge. Remainder of procedure completed without complication. The patient was hemodynamically stable, tolerated diet, and denied further hematochezia after the procedure; four days after colonoscopy, the patient experienced large volume hematochezia, with hemoglobin downtrend to 7.9g/dL. Repeat colonoscopy completed successfully and demonstrated sigmoid ulceration where clot was seen on prior colonoscopy, biopsies were taken. Initial pathologic evaluation demonstrated ulcerated granulation tissue, suggestive of mucosal injury without evidence of chronicity or granulomas. Tissue examined under Congo Red stain was positive for amyloid deposition. Patient was discharged the following day with no further episodes of hematochezia.
Discussion: AL amyloid can cause structural and vascular fragility. Identifying amyloid as the cause of GI bleed can be difficult as patients may present without confirmed AL diagnosis. Histologic confirmation with Congo red staining and apple-green birefringence under polarized light is diagnostic gold standard, but not routinely performed. It is imperative to maintain a high index of suspicion for amyloidosis in patients presenting with unexplained GI bleeding, with known or suspected plasma cell disorders. Early recognition is crucial, due to high morbidity and mortality of GI bleeds in patients with systemic AL amyloid.
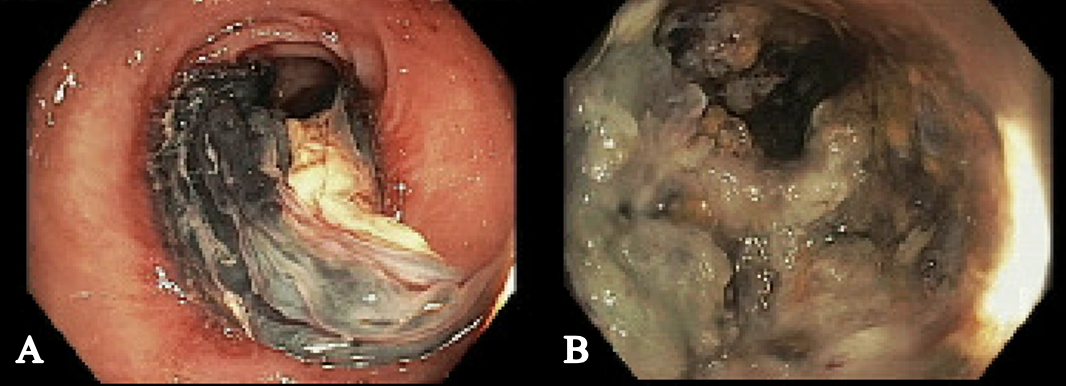
Figure: Figure 1: Pathology Slide of Colon Biopsy with Congo Red Staining
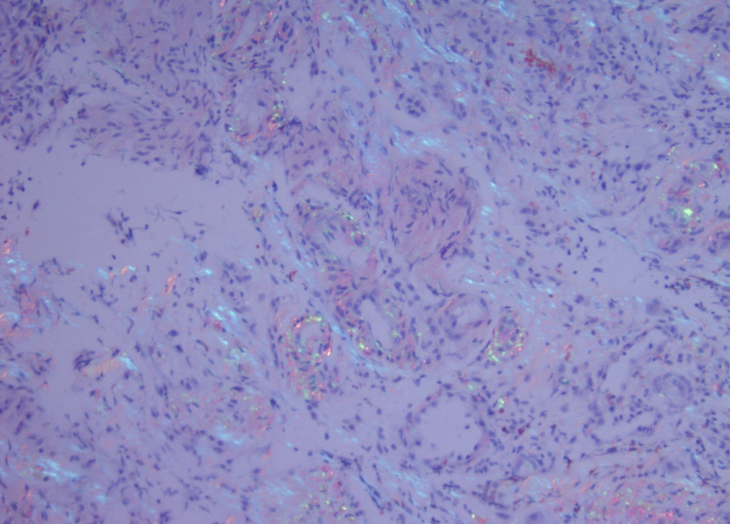
Figure: Figure 2: A: First Colonoscopy with Sigmoid Clot; B: Second Colonoscopy with Sigmoid Ulceration
Disclosures:
Claire Russell indicated no relevant financial relationships.
Ali Rida indicated no relevant financial relationships.
Caleb Glover indicated no relevant financial relationships.
Edward Cay indicated no relevant financial relationships.
Eric Nguyen indicated no relevant financial relationships.
John Walling indicated no relevant financial relationships.
Claire C. Russell, DO1, Ali Rida, MD1, Caleb Glover, DO1, Edward Cay, DO2, Eric Nguyen, MD1, John Walling, DO1. P0945 - Caught Red-Handed: Congo Red Unmasks Culprit in Gastrointestinal Bleed, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
