Sunday Poster Session
Category: GI Bleeding
P0940 - Clinical Outcomes in CAD Patients With Non-Variceal GI Bleed and In-Hospital ACS: Impact of Anticoagulation in a Propensity-Matched Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- FE
Fatima Elmustafa, MBBS
Henry Ford Warren
Warren, MI
Presenting Author(s)
Fatima Elmustafa, MBBS1, Ali Osman, MD2, Mohammad Adam, MD, MSc3, Tasneem Elmustafa, MBBS4, Nihal Babiker, MBBS5, Mohamed Abdallah, MD6
1Henry Ford Warren, Warren, MI; 2Washington University, Saint Louis, MO; 3University of Missouri-Kansas City, Kansas City, MO; 4Omdurman Islamic University, Al Rashidiya, Ajman, United Arab Emirates; 5Zafazig University, Zagazig, Ash Sharqiyah, Egypt; 6Corewell Health, Royal Oak, MI
Introduction: Management of acute coronary syndrome (ACS) in the setting of gastrointestinal (GI) bleeding is complex. While anticoagulation remains a cornerstone of ACS management, the potential contribution of demand ischemia may influence decisions about its use. This study evaluates clinical outcomes in patients with prior coronary artery disease (CAD) admitted for non-variceal GI bleeding who developed ACS, comparing those who received anticoagulation to those who did not.
Methods: We conducted a retrospective cohort study using TriNetX, a global federated health research network aggregating de-identified electronic health records. Adults (≥18 years) with a history of coronary artery disease (CAD) hospitalized for non-variceal upper or lower gastrointestinal bleeding were included. Patients who developed acute coronary syndrome (ACS) during hospitalization were divided into two groups: those who received anticoagulation with heparin and those who did not. Propensity score matching (1:1) was performed to balance baseline characteristics, including demographics, comorbidities (e.g., diabetes, chronic kidney disease), medication use (e.g., anticoagulants, statins), and race/ethnicity.
Results: Before matching, 10,469 patients with a history of CAD admitted for non-variceal GI bleeding who developed ACS received heparin, compared to 20,107 similar patients who did not. After 1:1 propensity score matching, each cohort included 9,266 patients. Post-matching, anticoagulation was associated with a non-significant trend toward lower in-hospital mortality (OR 0.844, 95% CI 0.692–1.030) and reduced rebleeding (OR 0.944, 95% CI 0.882–1.010). ICU admission rates were similar between groups (OR 1.00, 95% CI 0.416–2.404). However, patients receiving anticoagulation had significantly higher odds of requiring blood transfusion (OR 1.715, 95% CI 1.441–2.040).
Discussion: In patients with a history of CAD hospitalized for non-variceal GI bleeding who developed ACS, anticoagulation was not associated with a significant increase in mortality or rebleeding risk but was linked to higher transfusion requirements. Further prospective studies are needed to determine optimal management strategies in this complex clinical setting.
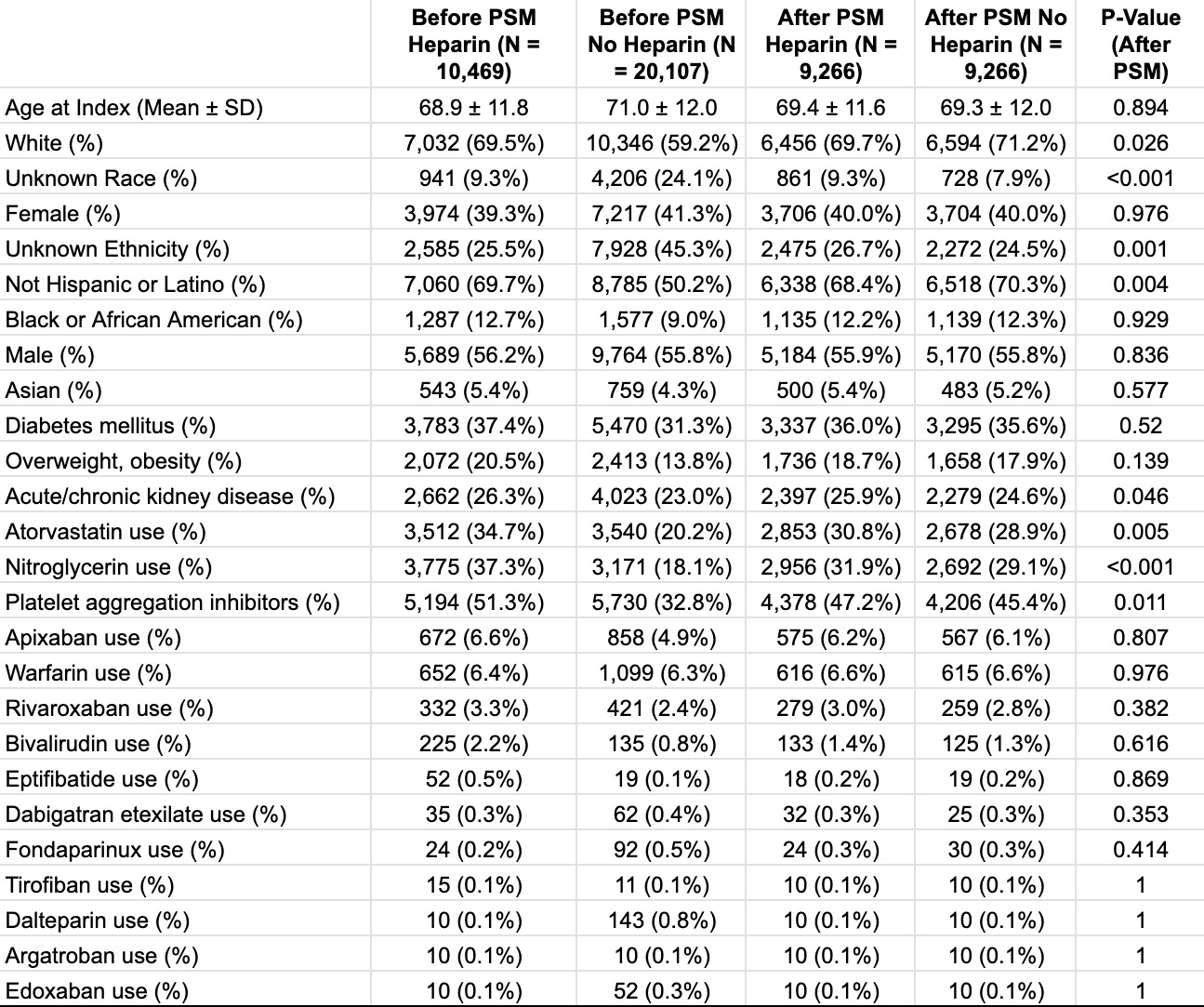
Figure: Table 1. Patient Characteristics Before and After Propensity Score Matching (PSM) in Heparin and No Heparin Cohorts
Disclosures:
Fatima Elmustafa indicated no relevant financial relationships.
Ali Osman indicated no relevant financial relationships.
Mohammad Adam indicated no relevant financial relationships.
Tasneem Elmustafa indicated no relevant financial relationships.
Nihal Babiker indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Fatima Elmustafa, MBBS1, Ali Osman, MD2, Mohammad Adam, MD, MSc3, Tasneem Elmustafa, MBBS4, Nihal Babiker, MBBS5, Mohamed Abdallah, MD6. P0940 - Clinical Outcomes in CAD Patients With Non-Variceal GI Bleed and In-Hospital ACS: Impact of Anticoagulation in a Propensity-Matched Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Warren, Warren, MI; 2Washington University, Saint Louis, MO; 3University of Missouri-Kansas City, Kansas City, MO; 4Omdurman Islamic University, Al Rashidiya, Ajman, United Arab Emirates; 5Zafazig University, Zagazig, Ash Sharqiyah, Egypt; 6Corewell Health, Royal Oak, MI
Introduction: Management of acute coronary syndrome (ACS) in the setting of gastrointestinal (GI) bleeding is complex. While anticoagulation remains a cornerstone of ACS management, the potential contribution of demand ischemia may influence decisions about its use. This study evaluates clinical outcomes in patients with prior coronary artery disease (CAD) admitted for non-variceal GI bleeding who developed ACS, comparing those who received anticoagulation to those who did not.
Methods: We conducted a retrospective cohort study using TriNetX, a global federated health research network aggregating de-identified electronic health records. Adults (≥18 years) with a history of coronary artery disease (CAD) hospitalized for non-variceal upper or lower gastrointestinal bleeding were included. Patients who developed acute coronary syndrome (ACS) during hospitalization were divided into two groups: those who received anticoagulation with heparin and those who did not. Propensity score matching (1:1) was performed to balance baseline characteristics, including demographics, comorbidities (e.g., diabetes, chronic kidney disease), medication use (e.g., anticoagulants, statins), and race/ethnicity.
Results: Before matching, 10,469 patients with a history of CAD admitted for non-variceal GI bleeding who developed ACS received heparin, compared to 20,107 similar patients who did not. After 1:1 propensity score matching, each cohort included 9,266 patients. Post-matching, anticoagulation was associated with a non-significant trend toward lower in-hospital mortality (OR 0.844, 95% CI 0.692–1.030) and reduced rebleeding (OR 0.944, 95% CI 0.882–1.010). ICU admission rates were similar between groups (OR 1.00, 95% CI 0.416–2.404). However, patients receiving anticoagulation had significantly higher odds of requiring blood transfusion (OR 1.715, 95% CI 1.441–2.040).
Discussion: In patients with a history of CAD hospitalized for non-variceal GI bleeding who developed ACS, anticoagulation was not associated with a significant increase in mortality or rebleeding risk but was linked to higher transfusion requirements. Further prospective studies are needed to determine optimal management strategies in this complex clinical setting.
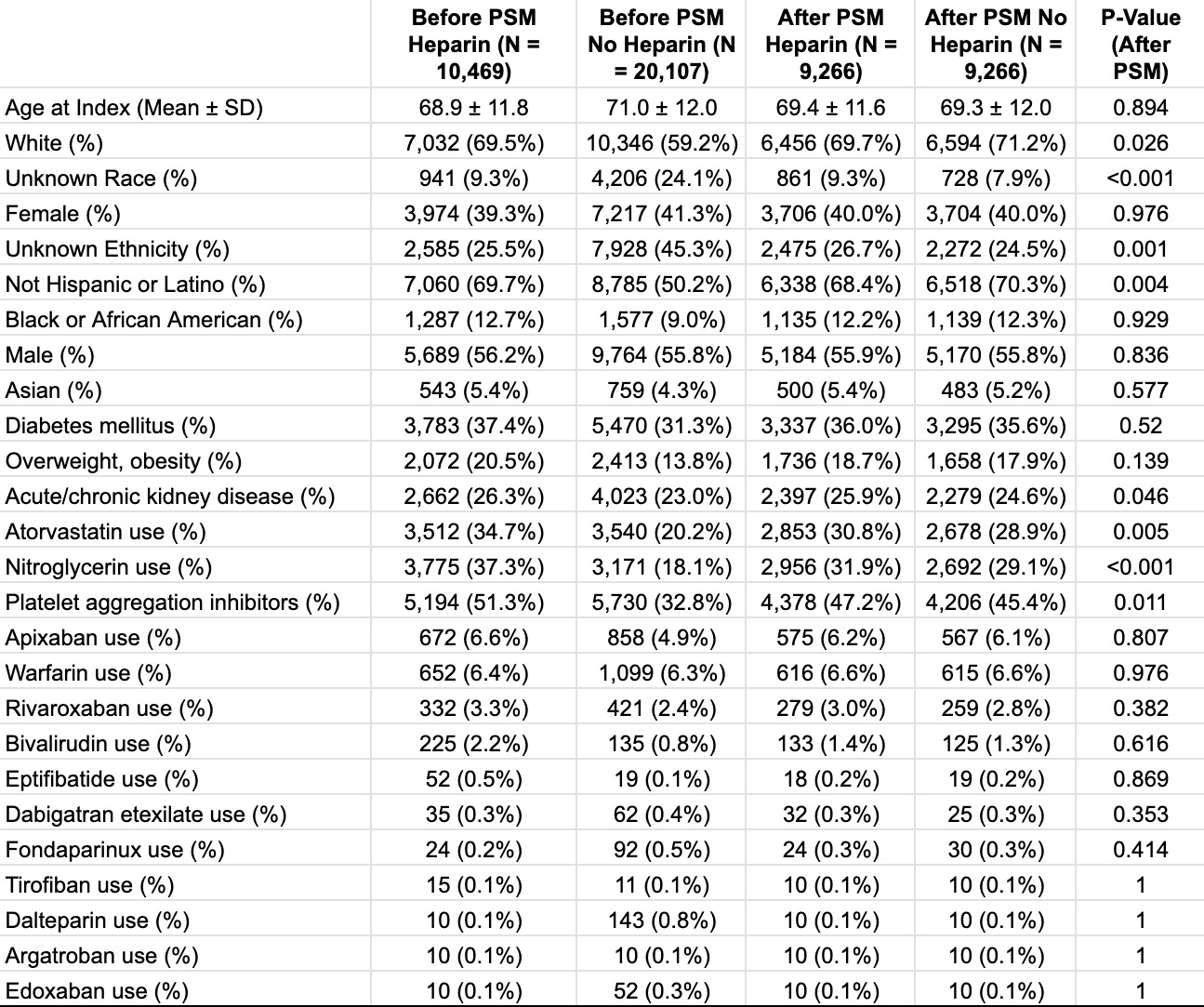
Figure: Table 1. Patient Characteristics Before and After Propensity Score Matching (PSM) in Heparin and No Heparin Cohorts
Disclosures:
Fatima Elmustafa indicated no relevant financial relationships.
Ali Osman indicated no relevant financial relationships.
Mohammad Adam indicated no relevant financial relationships.
Tasneem Elmustafa indicated no relevant financial relationships.
Nihal Babiker indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Fatima Elmustafa, MBBS1, Ali Osman, MD2, Mohammad Adam, MD, MSc3, Tasneem Elmustafa, MBBS4, Nihal Babiker, MBBS5, Mohamed Abdallah, MD6. P0940 - Clinical Outcomes in CAD Patients With Non-Variceal GI Bleed and In-Hospital ACS: Impact of Anticoagulation in a Propensity-Matched Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
