Sunday Poster Session
Category: GI Bleeding
P0939 - Comparative Outcomes of Endoscopic Hemostasis vs Angiographic Embolization in the Management of Severe Lower Gastrointestinal Bleeding
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Onoja-Frederick Okwori, MD, MPH
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Onoja-Frederick Okwori, MD, MPH1, Maurice Facey, MD2, Sedina Asafu-Adjaye, MD2, Nawaf Alhazmi, MD1, Andrew Catanzaro, MD3, Gregory S. Cooper, MD3, Omar Sims, PhD4
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 4Cleveland Clinic Foundation, Hoover, AL
Introduction: Lower GI bleeding (LGIB), which occurs distal to the ligament of Treitz, makes up about 20% of GI bleeds (1). Severe cases marked by hemodynamic instability or significant blood loss can lead to increased morbidity and mortality (2). Endoscopic and angiographic treatments are key options, but comparative data on their effectiveness are limited (1). Endoscopy enables direct visualization and treatment, while angiography is less invasive and helpful when endoscopy fails or not indicated. This study compares outcomes of both procedures to guide clinical decisions.
Methods: TriNetX, a large federated de-identified health network, provided data from 98 U.S. healthcare systems. Adults aged 18-85 with severe LGIB were identified using ICD-10 codes and grouped by treatment: angiographic embolization or endoscopy hemostasis. Data included demographics, procedure type, and outcomes. Inclusion and exclusion criteria were applied. Propensity Score Matching was used to balance groups, and outcomes were compared using risk ratios and 95% confidence intervals.
Results: A total of 479,163 patients with LGIB from 98 U.S. healthcare organizations were analyzed. After matching, 3,757 patients in each group (endoscopy vs. angiography) were compared. Both groups had a mean age of 65.3 years (Table 1a). As shown in Table 1b, rebleeding was significantly higher with angiography (57.7% vs. 25.4%; p < 0.001), though surgical risk was lower (2.3% vs. 8.9%; p < 0.001). Mortality (23.7% vs. 10.5%) and perforation risk (12.5% vs. 8.6%) were also greater with angiography, while anesthesia related complications were fewer (0.3% vs. 0.6%; p = 0.023). Cardiopulmonary arrest occurred equally (1.4%; p = 1.000). Bowel ischemia was slightly more frequent with endoscopy (1.0% vs. 0.6%; p = 0.041). Embolization rates were similar (0.3%; p = 0.669). Forest plot showing risk ratio for outcomes presented in Figure 1.
Discussion: This nationwide analysis showed that endoscopy was linked to lower rates of rebleeding, mortality and perforation compared to angiography. However, angiographic embolization had lower surgical and anesthesia-related risks. Cardiopulmonary arrest rates were similar. While endoscopy had better outcomes overall, angiography remains useful when endoscopy is delayed, contraindicated, or unsuccessful (4,5,6). Future randomized trials are needed to compare these procedures in diverse clinical settings and their impact on specific patient outcomes.
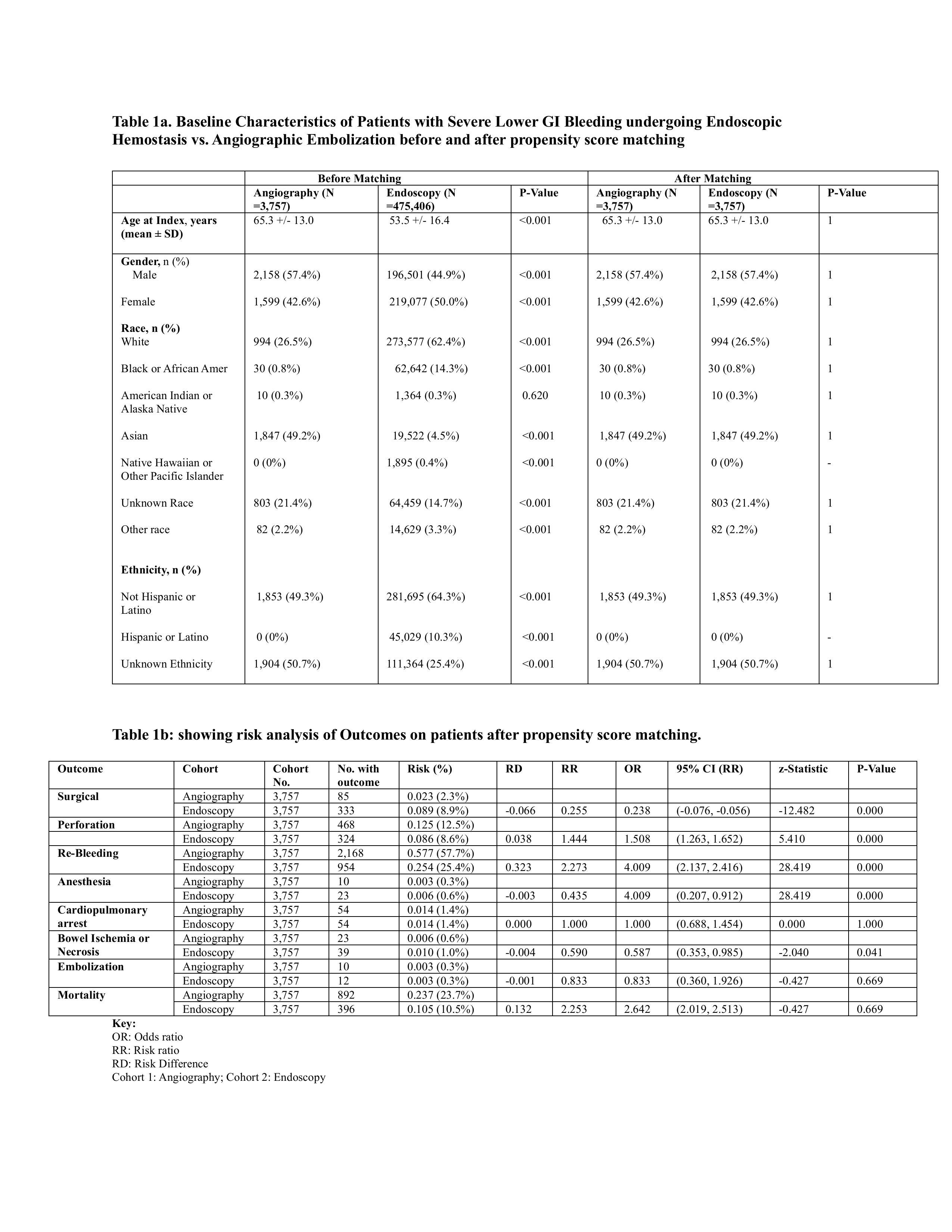
Figure: Table 1a. Baseline Characteristics of Patients with Severe Lower GI Bleeding undergoing Endoscopic Hemostasis vs. Angiographic Embolization before and after propensity score matching.
Table 1b: Risk analysis of Outcomes on patients after propensity score matching.

Figure: Figure 1. Forest Plot showing Risk Ratio for Outcomes
Disclosures:
Onoja-Frederick Okwori indicated no relevant financial relationships.
Maurice Facey indicated no relevant financial relationships.
Sedina Asafu-Adjaye indicated no relevant financial relationships.
Nawaf Alhazmi indicated no relevant financial relationships.
Andrew Catanzaro indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
Onoja-Frederick Okwori, MD, MPH1, Maurice Facey, MD2, Sedina Asafu-Adjaye, MD2, Nawaf Alhazmi, MD1, Andrew Catanzaro, MD3, Gregory S. Cooper, MD3, Omar Sims, PhD4. P0939 - Comparative Outcomes of Endoscopic Hemostasis vs Angiographic Embolization in the Management of Severe Lower Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 4Cleveland Clinic Foundation, Hoover, AL
Introduction: Lower GI bleeding (LGIB), which occurs distal to the ligament of Treitz, makes up about 20% of GI bleeds (1). Severe cases marked by hemodynamic instability or significant blood loss can lead to increased morbidity and mortality (2). Endoscopic and angiographic treatments are key options, but comparative data on their effectiveness are limited (1). Endoscopy enables direct visualization and treatment, while angiography is less invasive and helpful when endoscopy fails or not indicated. This study compares outcomes of both procedures to guide clinical decisions.
Methods: TriNetX, a large federated de-identified health network, provided data from 98 U.S. healthcare systems. Adults aged 18-85 with severe LGIB were identified using ICD-10 codes and grouped by treatment: angiographic embolization or endoscopy hemostasis. Data included demographics, procedure type, and outcomes. Inclusion and exclusion criteria were applied. Propensity Score Matching was used to balance groups, and outcomes were compared using risk ratios and 95% confidence intervals.
Results: A total of 479,163 patients with LGIB from 98 U.S. healthcare organizations were analyzed. After matching, 3,757 patients in each group (endoscopy vs. angiography) were compared. Both groups had a mean age of 65.3 years (Table 1a). As shown in Table 1b, rebleeding was significantly higher with angiography (57.7% vs. 25.4%; p < 0.001), though surgical risk was lower (2.3% vs. 8.9%; p < 0.001). Mortality (23.7% vs. 10.5%) and perforation risk (12.5% vs. 8.6%) were also greater with angiography, while anesthesia related complications were fewer (0.3% vs. 0.6%; p = 0.023). Cardiopulmonary arrest occurred equally (1.4%; p = 1.000). Bowel ischemia was slightly more frequent with endoscopy (1.0% vs. 0.6%; p = 0.041). Embolization rates were similar (0.3%; p = 0.669). Forest plot showing risk ratio for outcomes presented in Figure 1.
Discussion: This nationwide analysis showed that endoscopy was linked to lower rates of rebleeding, mortality and perforation compared to angiography. However, angiographic embolization had lower surgical and anesthesia-related risks. Cardiopulmonary arrest rates were similar. While endoscopy had better outcomes overall, angiography remains useful when endoscopy is delayed, contraindicated, or unsuccessful (4,5,6). Future randomized trials are needed to compare these procedures in diverse clinical settings and their impact on specific patient outcomes.
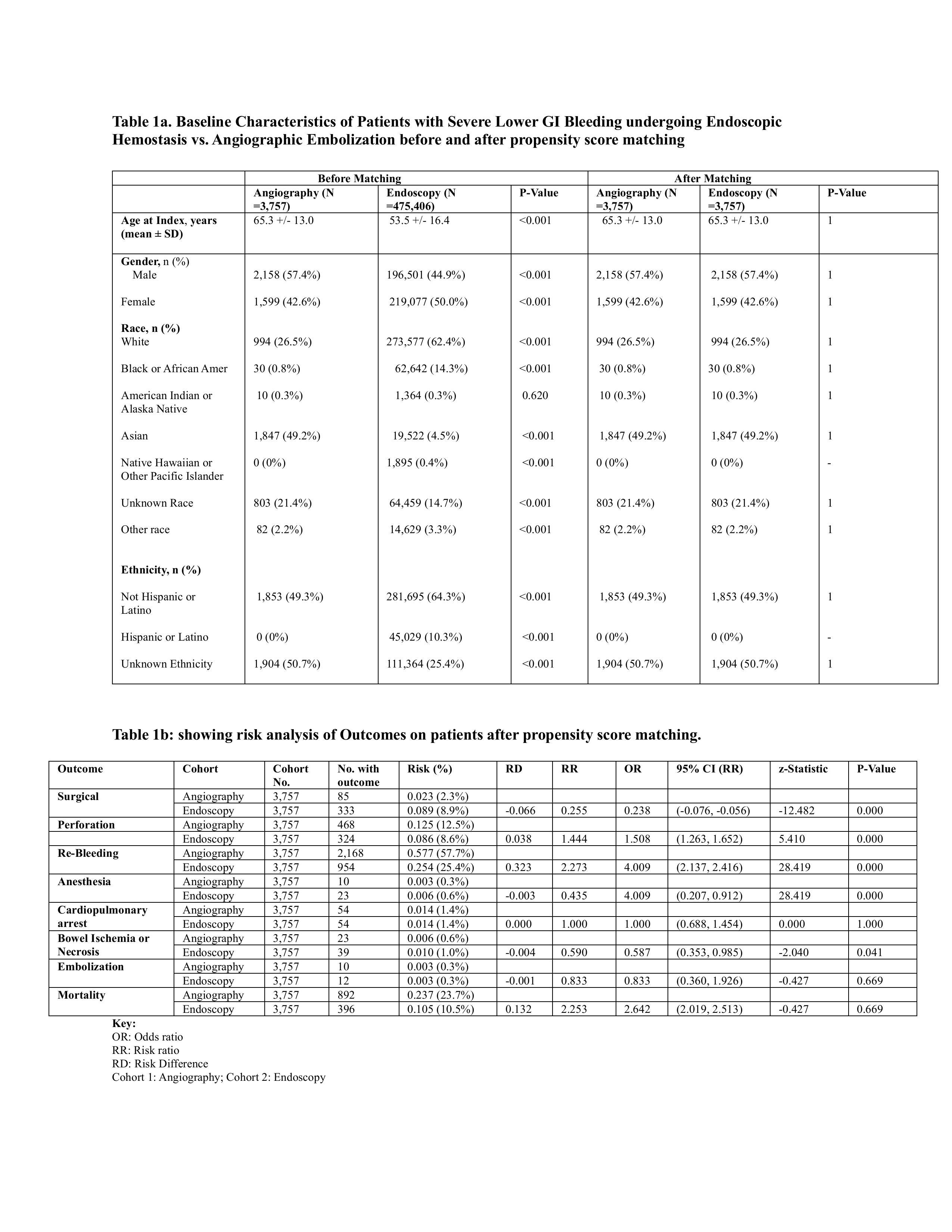
Figure: Table 1a. Baseline Characteristics of Patients with Severe Lower GI Bleeding undergoing Endoscopic Hemostasis vs. Angiographic Embolization before and after propensity score matching.
Table 1b: Risk analysis of Outcomes on patients after propensity score matching.

Figure: Figure 1. Forest Plot showing Risk Ratio for Outcomes
Disclosures:
Onoja-Frederick Okwori indicated no relevant financial relationships.
Maurice Facey indicated no relevant financial relationships.
Sedina Asafu-Adjaye indicated no relevant financial relationships.
Nawaf Alhazmi indicated no relevant financial relationships.
Andrew Catanzaro indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
Onoja-Frederick Okwori, MD, MPH1, Maurice Facey, MD2, Sedina Asafu-Adjaye, MD2, Nawaf Alhazmi, MD1, Andrew Catanzaro, MD3, Gregory S. Cooper, MD3, Omar Sims, PhD4. P0939 - Comparative Outcomes of Endoscopic Hemostasis vs Angiographic Embolization in the Management of Severe Lower Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
