Sunday Poster Session
Category: GI Bleeding
P0938 - It Is Not Who You Are but Where You Are: Understanding the Urban-Rural Divide in Lower Gastrointestinal Bleeding Treatment Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Reem Al Shabeeb, MD (she/her/hers)
Carilion Clinic
Roanoke, VA
Presenting Author(s)
Reem Al Shabeeb, MD1, Varun Kesar, MD1, Hiral Patel, MD1, Bara El Kurdi, MD1, Marwan Abougergi, MD2
1Carilion Clinic, Roanoke, VA; 2Inova Health System, Falls Church, VA
Introduction: Lower gastrointestinal bleed (LGIB) is a common gastrointestinal emergency. LGIB treatment depends on timely access to healthcare resources including colonoscopy, interventional radiology (IR), surgery and intensive care. Those resources are geographically unequally distributed in the United States. Thus, the aim of our study is to compare LGIB treatment outcomes between rural and urban areas.
Methods: This retrospective cohort study used the National Inpatient Sample 2021. Admissions with a principal diagnosis of LGIB were included. The primary outcome was in-hospital mortality. Secondary outcomes were 1-treatment modalities: endoscopic, radiologic and surgical therapy, 2-morbidity: hypovolemic shock and mechanical ventilation for >96 hours (PMV), 3- resource utilization: length of stay (LOS), total hospitalization costs and charges. Multivariate regression models were used to adjust for the confounders.
Results: There were 480,724 admissions for LGIB in 2021. Of those, 13% were for patients in rural areas. Patients in rural areas were more likely to be Caucasian, have lower income and receive treatment at large rural hospitals in the Midwest and south. Both rural and urban patient groups had similar mean ages (72 years) and comparable rates of anticoagulant, and antiplatelet therapy.
The overall in-hospital mortality rate was 2.0 %. The rates of endoscopic interventions, radiologic and surgical therapy were 1.0 %, 1.2%, and 0.03%, respectively. Hypovolemic shock and PMV occurred in 1.0% and 2.0 % of admissions respectively. The mean LOS was 5.4 days, with mean total hospitalization costs of $16,170 and charges of $1,645.
Adjusted results are presented in Table 1. Patients in rural areas had 21% higher odds of in-hospital mortality compared with those in urban areas. Both groups had similar odds of receiving endoscopic therapy, as well as IR and surgical therapy. However, patients in rural areas were less likely to receive care at urban (52 % vs. 99%, p< 0.01) or teaching hospitals (42% vs. 78%, p< 0.01) and more frequently transferred from another hospital (23% vs 8%, P< 0.01). The adjusted odds of shock were similar between the two groups but that of PMV were higher in the rural group.
Discussion: Patients with LGIB in rural areas experience higher in-hospital mortality and lower resource utilization compared to their urban counterparts. This disparity in treatment outcome could be explained at least in part by the unequal availability of local resources.
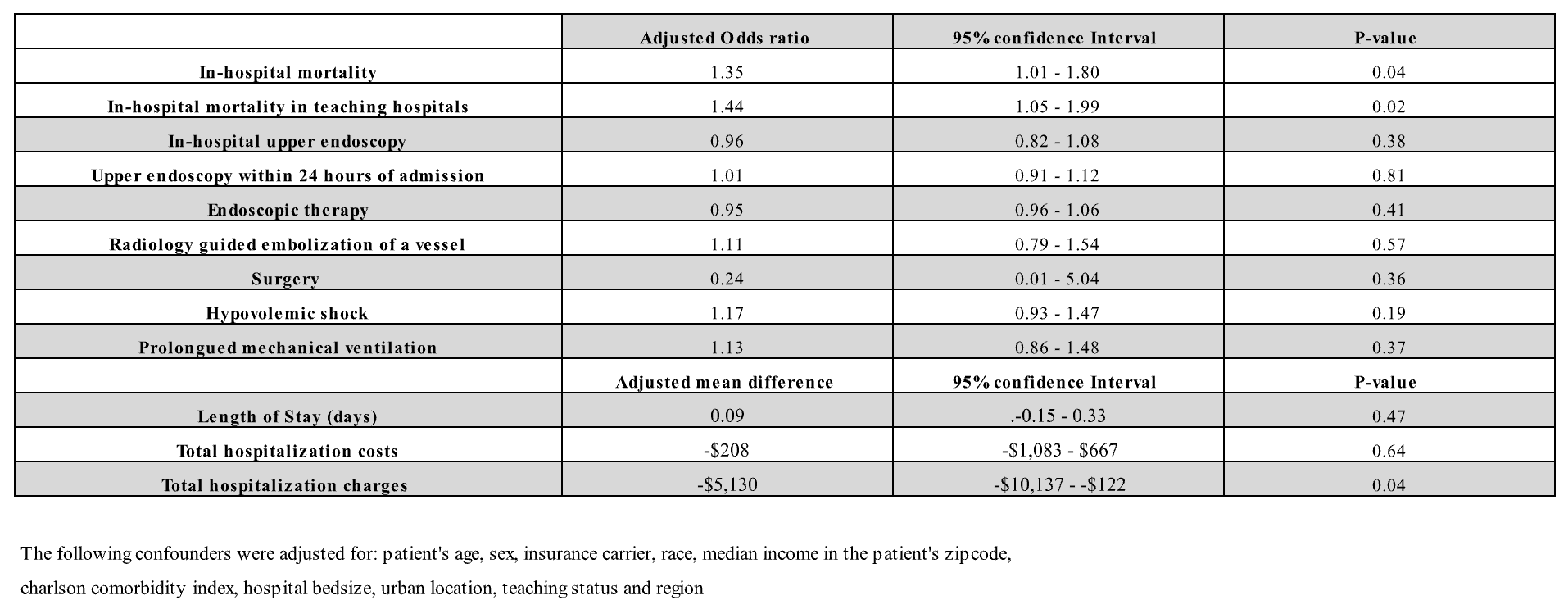
Figure: Table 1: Adjusted Results
Disclosures:
Reem Al Shabeeb indicated no relevant financial relationships.
Varun Kesar indicated no relevant financial relationships.
Hiral Patel indicated no relevant financial relationships.
Bara El Kurdi indicated no relevant financial relationships.
Marwan Abougergi indicated no relevant financial relationships.
Reem Al Shabeeb, MD1, Varun Kesar, MD1, Hiral Patel, MD1, Bara El Kurdi, MD1, Marwan Abougergi, MD2. P0938 - It Is Not Who You Are but Where You Are: Understanding the Urban-Rural Divide in Lower Gastrointestinal Bleeding Treatment Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Carilion Clinic, Roanoke, VA; 2Inova Health System, Falls Church, VA
Introduction: Lower gastrointestinal bleed (LGIB) is a common gastrointestinal emergency. LGIB treatment depends on timely access to healthcare resources including colonoscopy, interventional radiology (IR), surgery and intensive care. Those resources are geographically unequally distributed in the United States. Thus, the aim of our study is to compare LGIB treatment outcomes between rural and urban areas.
Methods: This retrospective cohort study used the National Inpatient Sample 2021. Admissions with a principal diagnosis of LGIB were included. The primary outcome was in-hospital mortality. Secondary outcomes were 1-treatment modalities: endoscopic, radiologic and surgical therapy, 2-morbidity: hypovolemic shock and mechanical ventilation for >96 hours (PMV), 3- resource utilization: length of stay (LOS), total hospitalization costs and charges. Multivariate regression models were used to adjust for the confounders.
Results: There were 480,724 admissions for LGIB in 2021. Of those, 13% were for patients in rural areas. Patients in rural areas were more likely to be Caucasian, have lower income and receive treatment at large rural hospitals in the Midwest and south. Both rural and urban patient groups had similar mean ages (72 years) and comparable rates of anticoagulant, and antiplatelet therapy.
The overall in-hospital mortality rate was 2.0 %. The rates of endoscopic interventions, radiologic and surgical therapy were 1.0 %, 1.2%, and 0.03%, respectively. Hypovolemic shock and PMV occurred in 1.0% and 2.0 % of admissions respectively. The mean LOS was 5.4 days, with mean total hospitalization costs of $16,170 and charges of $1,645.
Adjusted results are presented in Table 1. Patients in rural areas had 21% higher odds of in-hospital mortality compared with those in urban areas. Both groups had similar odds of receiving endoscopic therapy, as well as IR and surgical therapy. However, patients in rural areas were less likely to receive care at urban (52 % vs. 99%, p< 0.01) or teaching hospitals (42% vs. 78%, p< 0.01) and more frequently transferred from another hospital (23% vs 8%, P< 0.01). The adjusted odds of shock were similar between the two groups but that of PMV were higher in the rural group.
Discussion: Patients with LGIB in rural areas experience higher in-hospital mortality and lower resource utilization compared to their urban counterparts. This disparity in treatment outcome could be explained at least in part by the unequal availability of local resources.
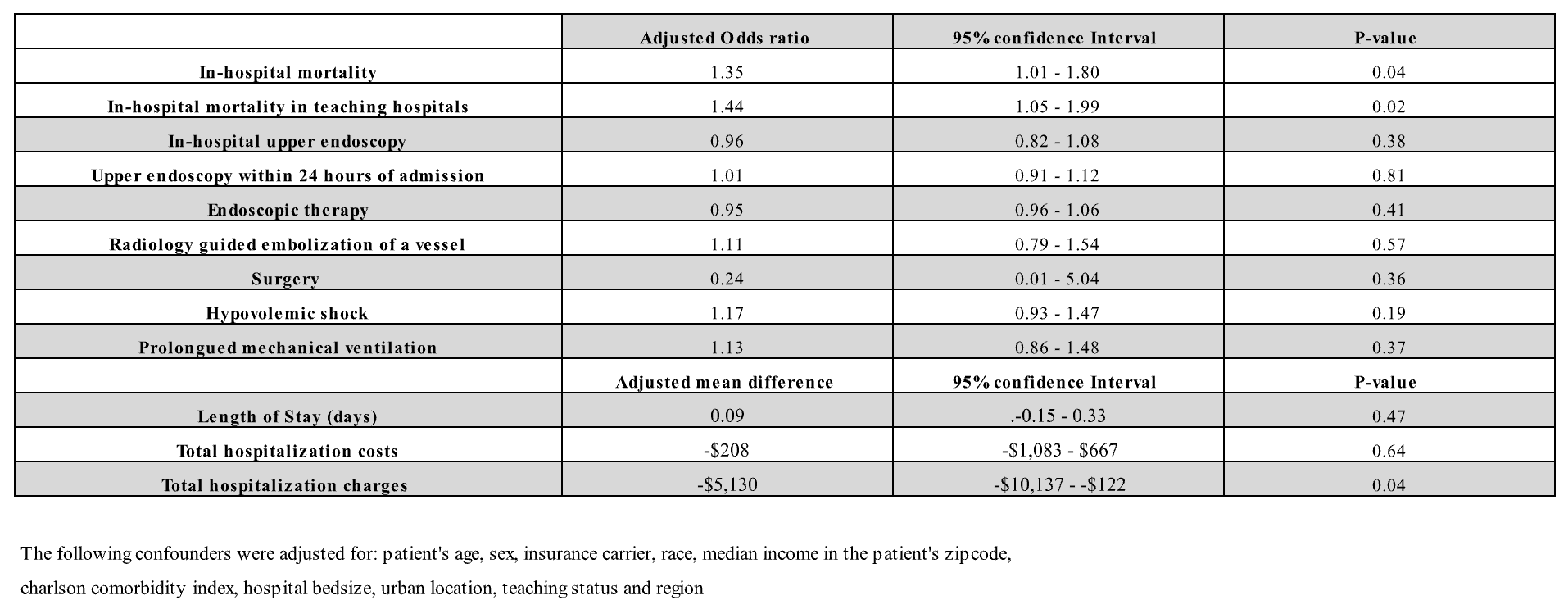
Figure: Table 1: Adjusted Results
Disclosures:
Reem Al Shabeeb indicated no relevant financial relationships.
Varun Kesar indicated no relevant financial relationships.
Hiral Patel indicated no relevant financial relationships.
Bara El Kurdi indicated no relevant financial relationships.
Marwan Abougergi indicated no relevant financial relationships.
Reem Al Shabeeb, MD1, Varun Kesar, MD1, Hiral Patel, MD1, Bara El Kurdi, MD1, Marwan Abougergi, MD2. P0938 - It Is Not Who You Are but Where You Are: Understanding the Urban-Rural Divide in Lower Gastrointestinal Bleeding Treatment Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
