Sunday Poster Session
Category: GI Bleeding
P0926 - Carvedilol Use in Cirrhosis: A National Database Study Linking Beta-Blockade to Reduced Bleeding and Readmissions
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AP
Achal Patel, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Rajmohan Rammohan, MD, Dilman Natt, MD, Achal Patel, MD, Sai Reshma Magam, MD, Leeza E. Pannikodu, MD, Amilcar Guaschino, MD, Cesar Orlando Ortiz Bernard, MD, Sindhuja Giridharan, MD, Amina Zafar, MD, Venkata Panchagnula, MD, Wing Hang Lau, DO, Sri Harsha Boppana, MD, Paul Mustacchia, MD
Nassau University Medical Center, East Meadow, NY
Introduction: Carvedilol, a non-selective beta-blocker, is widely prescribed for hypertension and heart failure. Recently, its potential in preventing variceal bleeding, a severe complication in cirrhosis patients, has been investigated. With the high rates of hospital readmissions among these patients, evaluating interventions to reduce these occurrences is vital. This study uses a large-scale national dataset to assess the effects of carvedilol on variceal bleeding incidence and subsequent hospital readmissions in cirrhosis patients.
Methods: We analyzed data from the Nationwide Inpatient Sample (HCUP) covering 2,858,576 adults between 2019 and 2024. The study focused on patients prescribed carvedilol, assessing its impact on variceal bleeding and readmission rates. Chi-square tests were used for categorical variables, examining carvedilol's effects on outcomes. Risk reduction was quantified using odds ratios (OR) with 95% confidence intervals (CI). Contingency tables evaluated bleeding and readmission rates at 30 and 60 days. Statistical significance was set at p < 0.05.
Results: Among 43,668 cirrhosis patients, those on Carvedilol (n=19,766) had significantly lower variceal bleeding (18.3% vs. 61.6%) and 30-day readmissions (0.3% vs. 51.8%) compared to non-users (n=23,902). At 60 days, readmissions were also reduced (1.0% vs. 44.7%). Carvedilol use was associated with lower odds of bleeding (p < 0.001), 30-day readmission (OR=0.001, 95% CI: 0.0008–0.0013; p< 0.001), and 60-day readmission (OR=0.37, 95% CI: 0.32–0.44; p< 0.001).
Discussion: This study demonstrates that carvedilol significantly reduces variceal bleeding and hospital readmission rates in cirrhosis patients. The decrease in 30-day and 60-day readmission rates suggests carvedilol provides both immediate and sustained benefits after discharge. These findings highlight carvedilol's potential as a preventive strategy for cirrhosis complications, improving patient outcomes and reducing healthcare utilization. Further research is needed to explore the mechanisms behind these effects and assess the long-term benefits of carvedilol therapy in diverse populations.
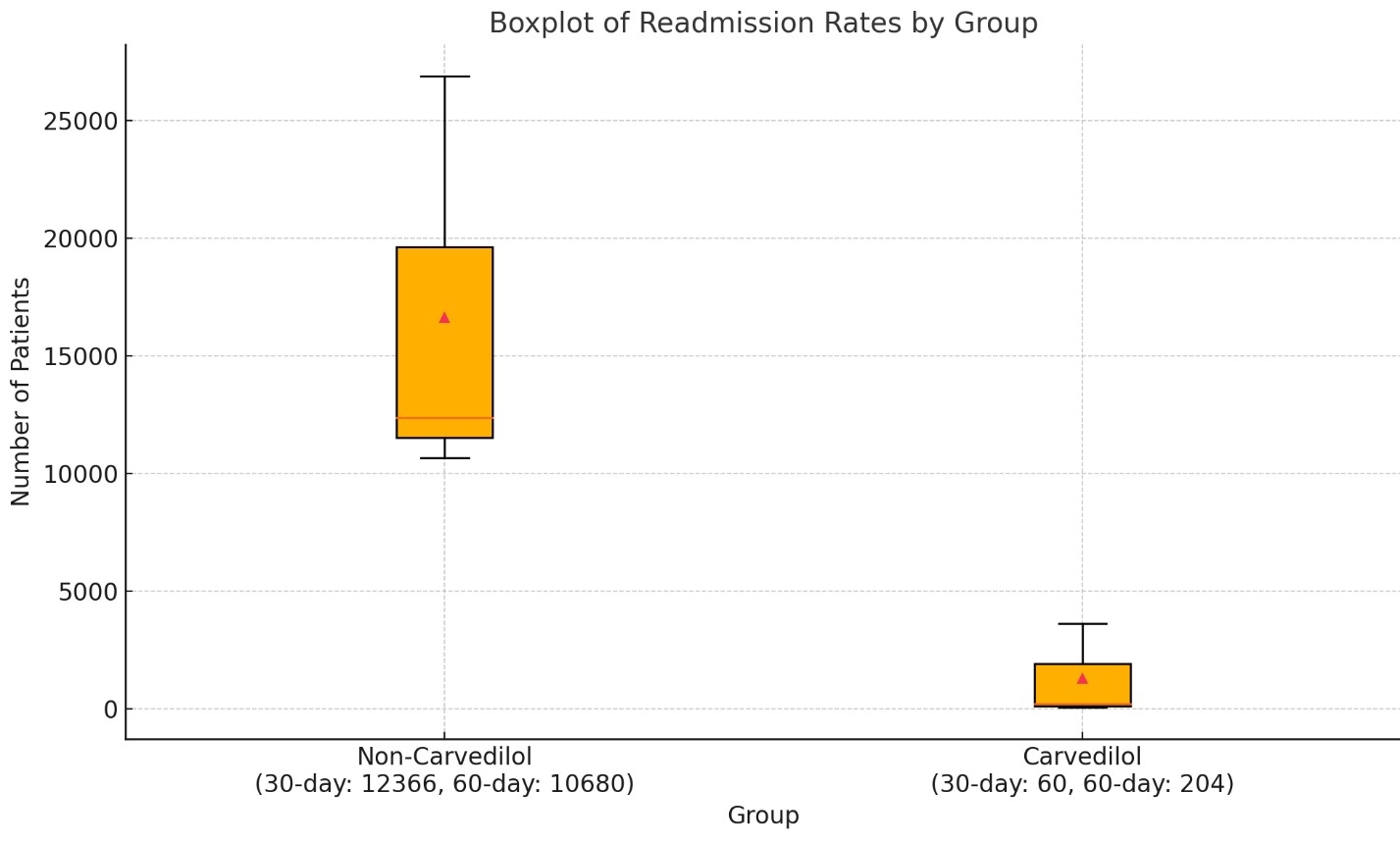
Figure: CARVEDILOL USE IN CIRRHOSIS
Disclosures:
Rajmohan Rammohan indicated no relevant financial relationships.
Dilman Natt indicated no relevant financial relationships.
Achal Patel indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Amilcar Guaschino indicated no relevant financial relationships.
Cesar Orlando Ortiz Bernard indicated no relevant financial relationships.
Sindhuja Giridharan indicated no relevant financial relationships.
Amina Zafar indicated no relevant financial relationships.
Venkata Panchagnula indicated no relevant financial relationships.
Wing Hang Lau indicated no relevant financial relationships.
Sri Harsha Boppana indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Rajmohan Rammohan, MD, Dilman Natt, MD, Achal Patel, MD, Sai Reshma Magam, MD, Leeza E. Pannikodu, MD, Amilcar Guaschino, MD, Cesar Orlando Ortiz Bernard, MD, Sindhuja Giridharan, MD, Amina Zafar, MD, Venkata Panchagnula, MD, Wing Hang Lau, DO, Sri Harsha Boppana, MD, Paul Mustacchia, MD. P0926 - Carvedilol Use in Cirrhosis: A National Database Study Linking Beta-Blockade to Reduced Bleeding and Readmissions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Carvedilol, a non-selective beta-blocker, is widely prescribed for hypertension and heart failure. Recently, its potential in preventing variceal bleeding, a severe complication in cirrhosis patients, has been investigated. With the high rates of hospital readmissions among these patients, evaluating interventions to reduce these occurrences is vital. This study uses a large-scale national dataset to assess the effects of carvedilol on variceal bleeding incidence and subsequent hospital readmissions in cirrhosis patients.
Methods: We analyzed data from the Nationwide Inpatient Sample (HCUP) covering 2,858,576 adults between 2019 and 2024. The study focused on patients prescribed carvedilol, assessing its impact on variceal bleeding and readmission rates. Chi-square tests were used for categorical variables, examining carvedilol's effects on outcomes. Risk reduction was quantified using odds ratios (OR) with 95% confidence intervals (CI). Contingency tables evaluated bleeding and readmission rates at 30 and 60 days. Statistical significance was set at p < 0.05.
Results: Among 43,668 cirrhosis patients, those on Carvedilol (n=19,766) had significantly lower variceal bleeding (18.3% vs. 61.6%) and 30-day readmissions (0.3% vs. 51.8%) compared to non-users (n=23,902). At 60 days, readmissions were also reduced (1.0% vs. 44.7%). Carvedilol use was associated with lower odds of bleeding (p < 0.001), 30-day readmission (OR=0.001, 95% CI: 0.0008–0.0013; p< 0.001), and 60-day readmission (OR=0.37, 95% CI: 0.32–0.44; p< 0.001).
Discussion: This study demonstrates that carvedilol significantly reduces variceal bleeding and hospital readmission rates in cirrhosis patients. The decrease in 30-day and 60-day readmission rates suggests carvedilol provides both immediate and sustained benefits after discharge. These findings highlight carvedilol's potential as a preventive strategy for cirrhosis complications, improving patient outcomes and reducing healthcare utilization. Further research is needed to explore the mechanisms behind these effects and assess the long-term benefits of carvedilol therapy in diverse populations.
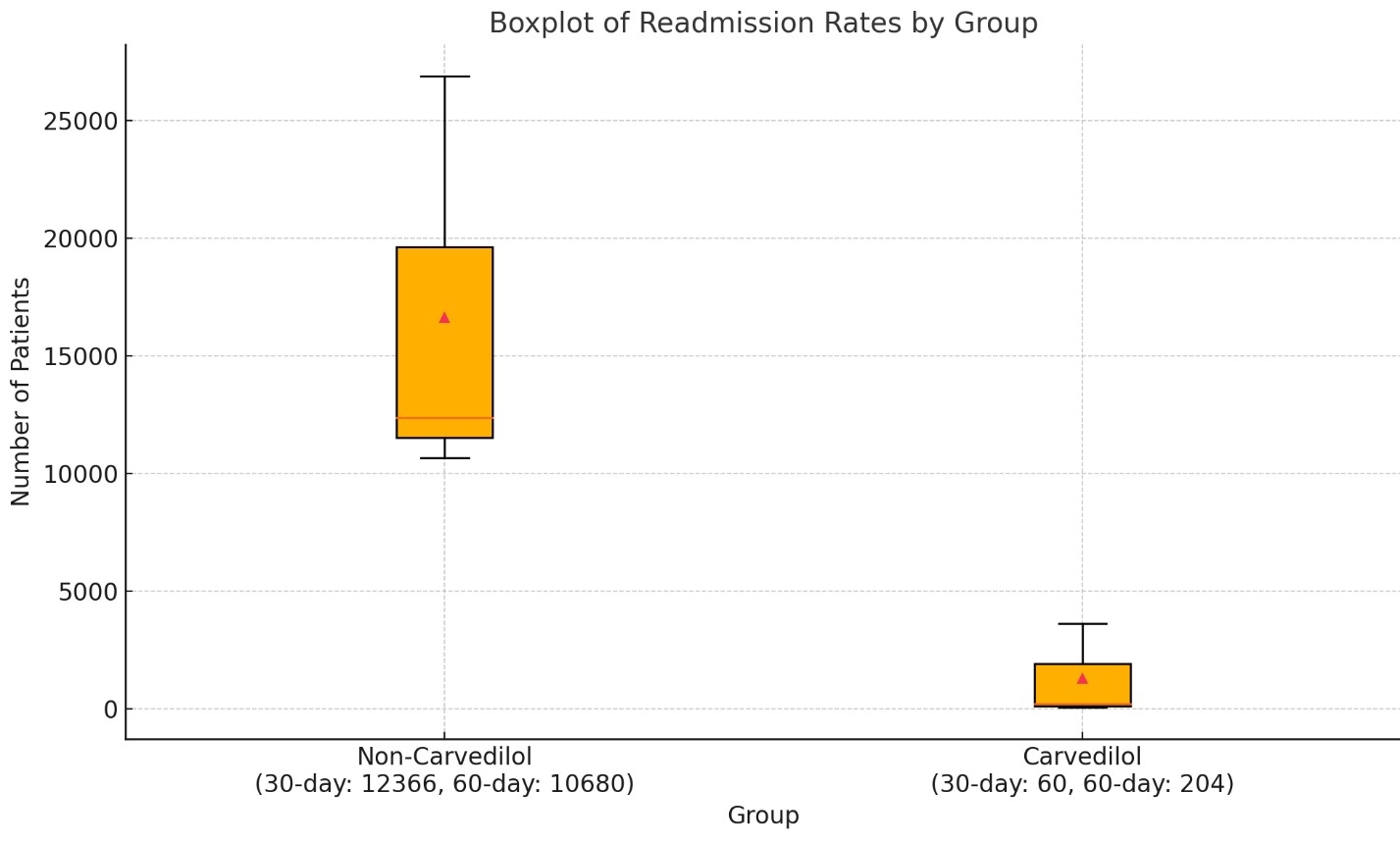
Figure: CARVEDILOL USE IN CIRRHOSIS
Disclosures:
Rajmohan Rammohan indicated no relevant financial relationships.
Dilman Natt indicated no relevant financial relationships.
Achal Patel indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Amilcar Guaschino indicated no relevant financial relationships.
Cesar Orlando Ortiz Bernard indicated no relevant financial relationships.
Sindhuja Giridharan indicated no relevant financial relationships.
Amina Zafar indicated no relevant financial relationships.
Venkata Panchagnula indicated no relevant financial relationships.
Wing Hang Lau indicated no relevant financial relationships.
Sri Harsha Boppana indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Rajmohan Rammohan, MD, Dilman Natt, MD, Achal Patel, MD, Sai Reshma Magam, MD, Leeza E. Pannikodu, MD, Amilcar Guaschino, MD, Cesar Orlando Ortiz Bernard, MD, Sindhuja Giridharan, MD, Amina Zafar, MD, Venkata Panchagnula, MD, Wing Hang Lau, DO, Sri Harsha Boppana, MD, Paul Mustacchia, MD. P0926 - Carvedilol Use in Cirrhosis: A National Database Study Linking Beta-Blockade to Reduced Bleeding and Readmissions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
