Sunday Poster Session
Category: General Endoscopy
P0896 - Cutting Through Challenges: Endoscopic Submucosal Dissection for Esophageal Adenocarcinoma Amidst Variceal Vulnerability
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Fred Ahmadi, DO
Ascension Providence Hospital
Southfield, MI
Presenting Author(s)
Award: ACG Presidential Poster Award
Fred Ahmadi, DO, Saif Affas, MD, Roberto Gamarra, MD, FACG
Ascension Providence Hospital, Southfield, MI
Introduction: Endoscopic submucosal dissection (ESD) offers a curative, organ-preserving approach for early esophageal adenocarcinoma (EAC), particularly in patients who are poor surgical candidates. However, the presence of esophageal varices, commonly due to portal hypertension, poses significant hemorrhagic risk, often limiting the use of standard endoscopic therapies. Also, current surveillance guidelines typically reserve intervention for Barrett’s esophagus (BE) segments ≥1 cm unless additional risk factors are present. We present a rare case of EAC arising in nodular short-segment BE in a cirrhotic patient with esophageal varices, successfully managed with ESD.
Case Description/
Methods: A 67-year-old man with a history of cirrhosis underwent EGD for surveillance. A nodular lesion at the GE junction was noted within a 1 cm segment of BE, along with grade 2 esophageal varices. Biopsies revealed villous architecture with high-grade dysplasia and intramucosal adenocarcinoma. PET imaging showed no metastasis. Due to cirrhosis and varices, he was deemed high-risk for surgery and referred for endoscopy. ESD was performed with thermal marking and submucosal lifting using methylene blue solution. A 3 × 5 cm en bloc resection was achieved, encompassing the lower esophagus and gastric cardia. Visible vessels were coagulated prophylactically. There were no immediate or delayed bleeding complications. Pathology confirmed moderately differentiated adenocarcinoma with submucosal invasion (5 mm), arising in BE with high-grade dysplasia. All margins were negative. At six-month follow-up, EGD showed residual varices but no recurrent neoplasia. Biopsies revealed only mild chronic inflammation.
Discussion: This case supports the feasibility of ESD in patients with early EAC and concurrent varices when surgical resection is contraindicated. While varices are generally considered a relative contraindication due to bleeding risk, careful planning and hemostatic technique can mitigate complications. Watanabe et al. (Endosc Int Open, 2020) demonstrated the technical safety of ESD in similar contexts and our case adds to this emerging evidence.
Additionally, while short-segment BE is typically considered low risk, nodularity or dysplasia warrants close surveillance. Barrie et al. (Surg Endosc, 2021) reported that EAC can arise in very short segments of BE, challenging traditional models. This case shows the need for individualized assessment and highlights ESD as a viable option in complex clinical settings.
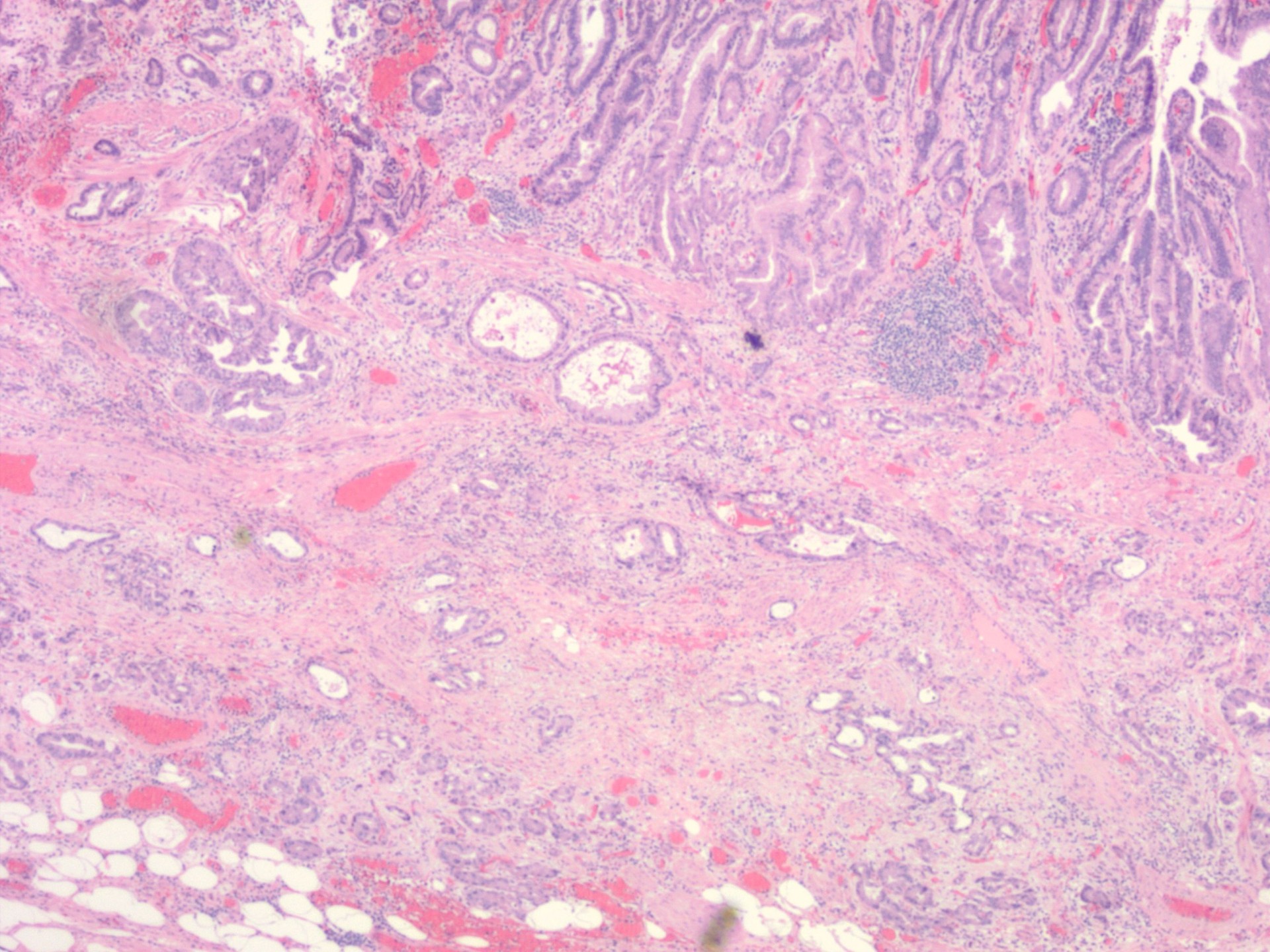
Figure: Esophageal adenocarcinoma, this is the base of the lesion with invasive glands extending into the submucosa.

Figure: Endoscopic view of the lesion, later identified as adenocarcinoma, seen at the GE junction.
Disclosures:
Fred Ahmadi indicated no relevant financial relationships.
Saif Affas indicated no relevant financial relationships.
Roberto Gamarra indicated no relevant financial relationships.
Fred Ahmadi, DO, Saif Affas, MD, Roberto Gamarra, MD, FACG. P0896 - Cutting Through Challenges: Endoscopic Submucosal Dissection for Esophageal Adenocarcinoma Amidst Variceal Vulnerability, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Fred Ahmadi, DO, Saif Affas, MD, Roberto Gamarra, MD, FACG
Ascension Providence Hospital, Southfield, MI
Introduction: Endoscopic submucosal dissection (ESD) offers a curative, organ-preserving approach for early esophageal adenocarcinoma (EAC), particularly in patients who are poor surgical candidates. However, the presence of esophageal varices, commonly due to portal hypertension, poses significant hemorrhagic risk, often limiting the use of standard endoscopic therapies. Also, current surveillance guidelines typically reserve intervention for Barrett’s esophagus (BE) segments ≥1 cm unless additional risk factors are present. We present a rare case of EAC arising in nodular short-segment BE in a cirrhotic patient with esophageal varices, successfully managed with ESD.
Case Description/
Methods: A 67-year-old man with a history of cirrhosis underwent EGD for surveillance. A nodular lesion at the GE junction was noted within a 1 cm segment of BE, along with grade 2 esophageal varices. Biopsies revealed villous architecture with high-grade dysplasia and intramucosal adenocarcinoma. PET imaging showed no metastasis. Due to cirrhosis and varices, he was deemed high-risk for surgery and referred for endoscopy. ESD was performed with thermal marking and submucosal lifting using methylene blue solution. A 3 × 5 cm en bloc resection was achieved, encompassing the lower esophagus and gastric cardia. Visible vessels were coagulated prophylactically. There were no immediate or delayed bleeding complications. Pathology confirmed moderately differentiated adenocarcinoma with submucosal invasion (5 mm), arising in BE with high-grade dysplasia. All margins were negative. At six-month follow-up, EGD showed residual varices but no recurrent neoplasia. Biopsies revealed only mild chronic inflammation.
Discussion: This case supports the feasibility of ESD in patients with early EAC and concurrent varices when surgical resection is contraindicated. While varices are generally considered a relative contraindication due to bleeding risk, careful planning and hemostatic technique can mitigate complications. Watanabe et al. (Endosc Int Open, 2020) demonstrated the technical safety of ESD in similar contexts and our case adds to this emerging evidence.
Additionally, while short-segment BE is typically considered low risk, nodularity or dysplasia warrants close surveillance. Barrie et al. (Surg Endosc, 2021) reported that EAC can arise in very short segments of BE, challenging traditional models. This case shows the need for individualized assessment and highlights ESD as a viable option in complex clinical settings.
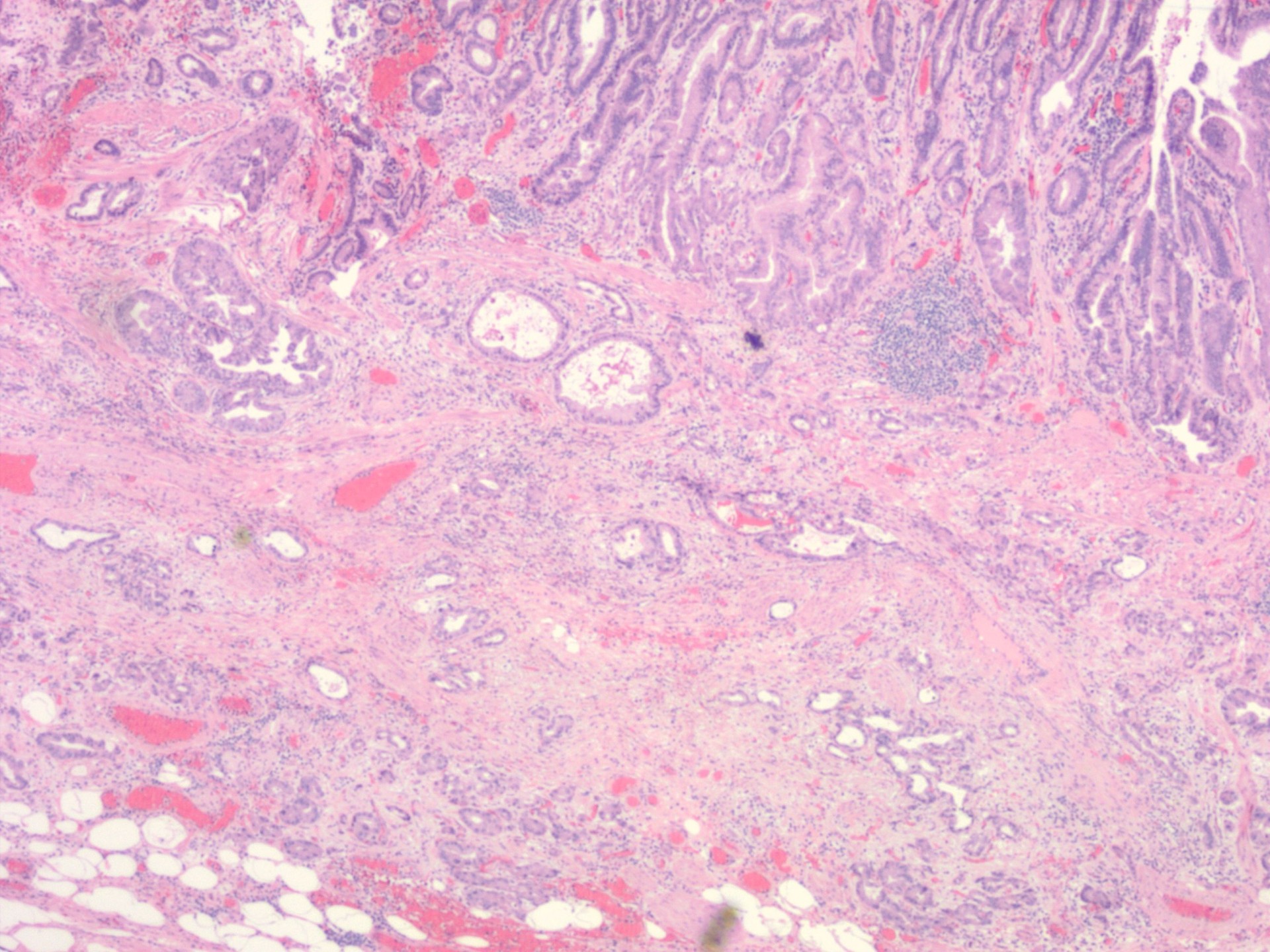
Figure: Esophageal adenocarcinoma, this is the base of the lesion with invasive glands extending into the submucosa.

Figure: Endoscopic view of the lesion, later identified as adenocarcinoma, seen at the GE junction.
Disclosures:
Fred Ahmadi indicated no relevant financial relationships.
Saif Affas indicated no relevant financial relationships.
Roberto Gamarra indicated no relevant financial relationships.
Fred Ahmadi, DO, Saif Affas, MD, Roberto Gamarra, MD, FACG. P0896 - Cutting Through Challenges: Endoscopic Submucosal Dissection for Esophageal Adenocarcinoma Amidst Variceal Vulnerability, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

