Sunday Poster Session
Category: General Endoscopy
P0891 - Not Every Perioral Pigmentation Is Suggestive of Peutz-Jeghers Syndrome: Have You Thought of Laugier-Hunziker Syndrome?
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Hadassah Polydore
Penn State University
Hershey, PA
Presenting Author(s)
Hadassah Polydore, 1, Smriti Kochhar, DO2, John Levenick, MD2, Thomas McGarrity, MD2, Hadie Razjouyan, MD3
1Penn State University, Hershey, PA; 2Penn State College of Medicine, Hershey, PA; 3Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Peutz-Jeghers Syndrome (PJS) is a rare autosomal dominant disorder most often caused by mutations in the STK11 (LKB1) gene. It is associated with an increased risk of gastrointestinal and endocrine malignancies. Diagnosis is based on at least two of the following criteria: (1) family history of PJS, (2) characteristic mucocutaneous pigmentation, and (3) presence of hamartomatous gastrointestinal polyps.
Perioral pigmentation, a hallmark of PJS, may also occur in conditions.
We present a patient with gastrointestinal symptoms and perioral pigmentation, who sought multiple specialist opinions following a preliminary diagnosis of PJS based solely on mucocutaneous findings.
Case Description/
Methods: A 47 year-old female with a history of chronic constipation, Gastroesophageal reflux disease, uterine fibroids, Tobacco and opioid use disorder presented to her primary care doctor for inability to tolerate oral intake and abdominal pain. Physical exam revealed multiple dark confluent macules on the oral and left vermillion border. Patient reports that lip pigmentation has developed gradually since age 14. Her lip lesions were biopsied due to concerns for melanoma. Histological examination was non-specific but suggestive of lentigo. Considering patient’s symptoms and reported bile duct dilation seen on her prior CT scan, an upper endoscopic examination was conducted. Upper endoscopy and echoendoscopy exam were essentially unremarkable except for mild common bile duct dilation likely due to chronic opioid use. Furthermore, her screening colonoscopy at the age of 45 revealed no evidence of polyps. With a normal endoscopic and colonoscopy examination, and family history of liver and pancreatic cancer, genetic testing was ordered which was negative for the STK11 (LKB1) mutation. She also had CT enterography to look for small bowel lesions which came back negative. With negative genetic testing and no evidence of hamartomatous polyps on endoscopic and colonoscopy testing, as well as imaging, it was determined that the patient is unlikely to have PJS but rather Laugier-Hunziker syndrome considering not having other medical condition.
Discussion: Laugier-Hunziker syndrome presents with adult onset benign basal hyperpigmentation of nail beds, and perioral and acral regions of the body. There is no known evidence of genetic transmission and no known malignant associations or systemic abnormalities.
With its similarities to Peutz-Jegher and Addison’s disease, it is often a diagnosis of exclusion.
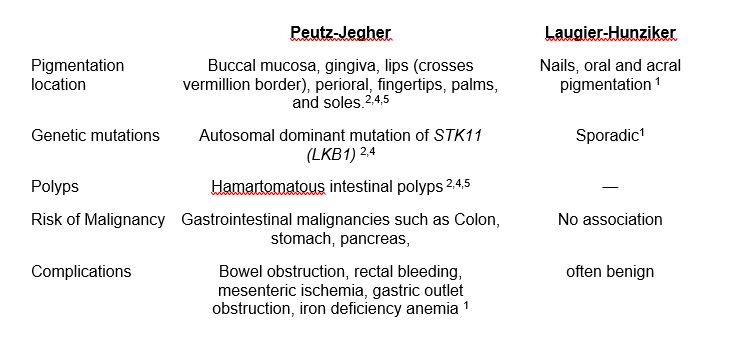
Figure: Key differences between Peutz-Jegher Syndrome and Laugier-Hunziker syndrome
Disclosures:
Hadassah Polydore indicated no relevant financial relationships.
Smriti Kochhar indicated no relevant financial relationships.
John Levenick indicated no relevant financial relationships.
Thomas McGarrity indicated no relevant financial relationships.
Hadie Razjouyan indicated no relevant financial relationships.
Hadassah Polydore, 1, Smriti Kochhar, DO2, John Levenick, MD2, Thomas McGarrity, MD2, Hadie Razjouyan, MD3. P0891 - Not Every Perioral Pigmentation Is Suggestive of Peutz-Jeghers Syndrome: Have You Thought of Laugier-Hunziker Syndrome?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Penn State University, Hershey, PA; 2Penn State College of Medicine, Hershey, PA; 3Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Peutz-Jeghers Syndrome (PJS) is a rare autosomal dominant disorder most often caused by mutations in the STK11 (LKB1) gene. It is associated with an increased risk of gastrointestinal and endocrine malignancies. Diagnosis is based on at least two of the following criteria: (1) family history of PJS, (2) characteristic mucocutaneous pigmentation, and (3) presence of hamartomatous gastrointestinal polyps.
Perioral pigmentation, a hallmark of PJS, may also occur in conditions.
We present a patient with gastrointestinal symptoms and perioral pigmentation, who sought multiple specialist opinions following a preliminary diagnosis of PJS based solely on mucocutaneous findings.
Case Description/
Methods: A 47 year-old female with a history of chronic constipation, Gastroesophageal reflux disease, uterine fibroids, Tobacco and opioid use disorder presented to her primary care doctor for inability to tolerate oral intake and abdominal pain. Physical exam revealed multiple dark confluent macules on the oral and left vermillion border. Patient reports that lip pigmentation has developed gradually since age 14. Her lip lesions were biopsied due to concerns for melanoma. Histological examination was non-specific but suggestive of lentigo. Considering patient’s symptoms and reported bile duct dilation seen on her prior CT scan, an upper endoscopic examination was conducted. Upper endoscopy and echoendoscopy exam were essentially unremarkable except for mild common bile duct dilation likely due to chronic opioid use. Furthermore, her screening colonoscopy at the age of 45 revealed no evidence of polyps. With a normal endoscopic and colonoscopy examination, and family history of liver and pancreatic cancer, genetic testing was ordered which was negative for the STK11 (LKB1) mutation. She also had CT enterography to look for small bowel lesions which came back negative. With negative genetic testing and no evidence of hamartomatous polyps on endoscopic and colonoscopy testing, as well as imaging, it was determined that the patient is unlikely to have PJS but rather Laugier-Hunziker syndrome considering not having other medical condition.
Discussion: Laugier-Hunziker syndrome presents with adult onset benign basal hyperpigmentation of nail beds, and perioral and acral regions of the body. There is no known evidence of genetic transmission and no known malignant associations or systemic abnormalities.
With its similarities to Peutz-Jegher and Addison’s disease, it is often a diagnosis of exclusion.
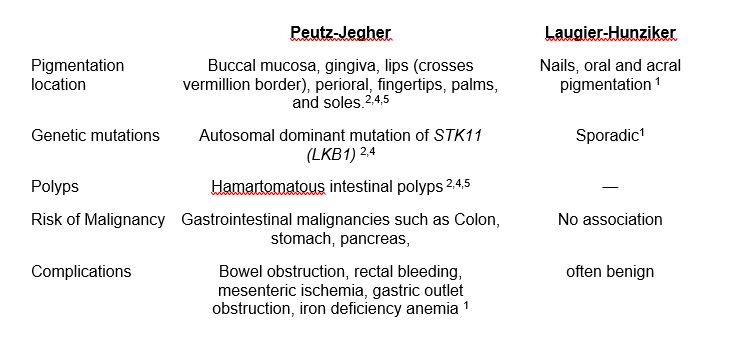
Figure: Key differences between Peutz-Jegher Syndrome and Laugier-Hunziker syndrome
Disclosures:
Hadassah Polydore indicated no relevant financial relationships.
Smriti Kochhar indicated no relevant financial relationships.
John Levenick indicated no relevant financial relationships.
Thomas McGarrity indicated no relevant financial relationships.
Hadie Razjouyan indicated no relevant financial relationships.
Hadassah Polydore, 1, Smriti Kochhar, DO2, John Levenick, MD2, Thomas McGarrity, MD2, Hadie Razjouyan, MD3. P0891 - Not Every Perioral Pigmentation Is Suggestive of Peutz-Jeghers Syndrome: Have You Thought of Laugier-Hunziker Syndrome?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
