Sunday Poster Session
Category: General Endoscopy
P0889 - An Unintended Consequence: Dysphagia Following Bronchial Artery Embolization for Recurrent Hemoptysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Tsola Efejuku, MD
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Tsola Efejuku, MD1, Manavi Bhagwat, MD1, Himesh Zaver, MD2, Nicola Litchfield, DO1, Jeanetta Frye, MD1
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia Health, Charlottesville, VA
Introduction: Bronchial artery embolization (BAE) is a treatment for recurrent hemoptysis. Although adverse events are rare, we present a case of dysphagia caused by ischemic esophageal ulceration following BAE.
Case Description/
Methods: A 61-year-old female patient presented to a tertiary care center with hemoptysis. Past medical history was significant for paroxysmal atrial fibrillation and end-stage heart failure requiring a left ventricular assist device and warfarin anticoagulation. The patient had recurrent admissions for hemoptysis not amenable to standard hemostatic therapies via bronchoscopy. Following multidisciplinary discussion, the patient underwent catheter-directed BAE of her left bronchial artery for recurrent hemoptysis. One week after BAE procedure, the patient developed odynophagia and dysphagia to both solids and liquids, prompting gastrointestinal consultation. Initial evaluation included a barium esophagram, which was unremarkable except for a small hiatal hernia (Figure 1). The patient subsequently underwent esophagogastroduodenoscopy (EGD), which revealed a large esophageal ulcer (Figure 2A–B) surrounded by focal ischemic-appearing mucosa and food debris (Figure 2C), located approximately 25 cm from the incisors. The mucosa proximal and distal to the ulcer appeared normal and healthy. The ulcer and ischemic appearing mucosa were biopsied. Pathology was supportive of acute and chronic inflammation with reactive changes consistent with ischemia-related injury. Stains for fungal and viral pathogens were negative. The patient was started on a proton pump inhibitor and a low-residue dysphagia diet and was discharged home in stable condition.
Discussion: The major arteries supplying the esophagus include the inferior thyroid, bronchial, left gastric, and left phrenic arteries. In this case, BAE involving the left bronchial artery resulted in esophageal ischemia, leading to ulceration and esophageal symptoms. Although food debris was noted on EGD, the overall findings were not consistent with a stasis ulcer, underscoring the importance of avoiding anchoring bias in clinical interpretation. This case also emphasizes the importance of a thorough understanding of esophageal vascular anatomy and the careful collection of a detailed patient history to guide timely diagnosis and management.
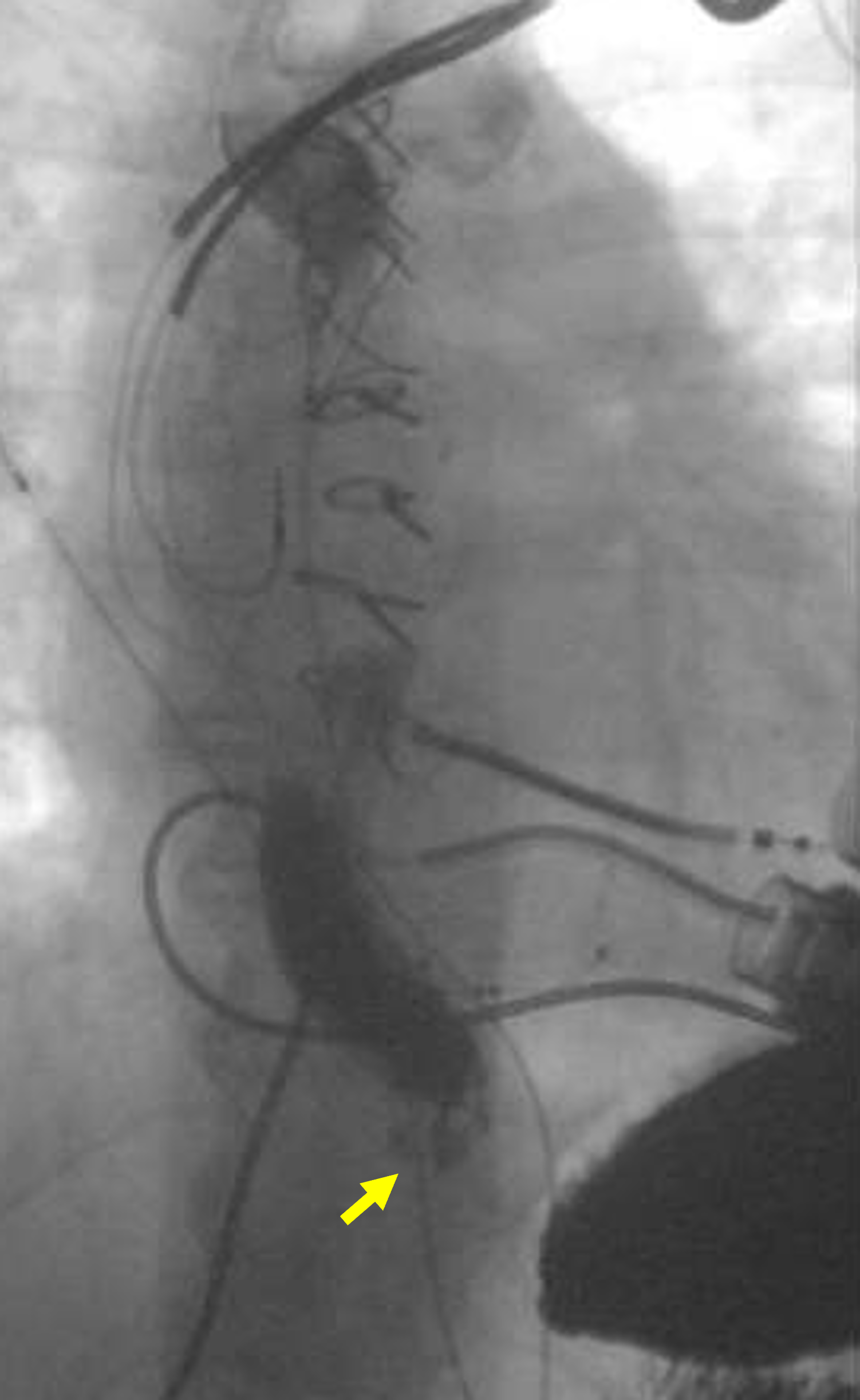
Figure: Figure 1. Barium esophagram suggestive of normal esophageal mucosa and small type I hiatal hernia (yellow arrow)
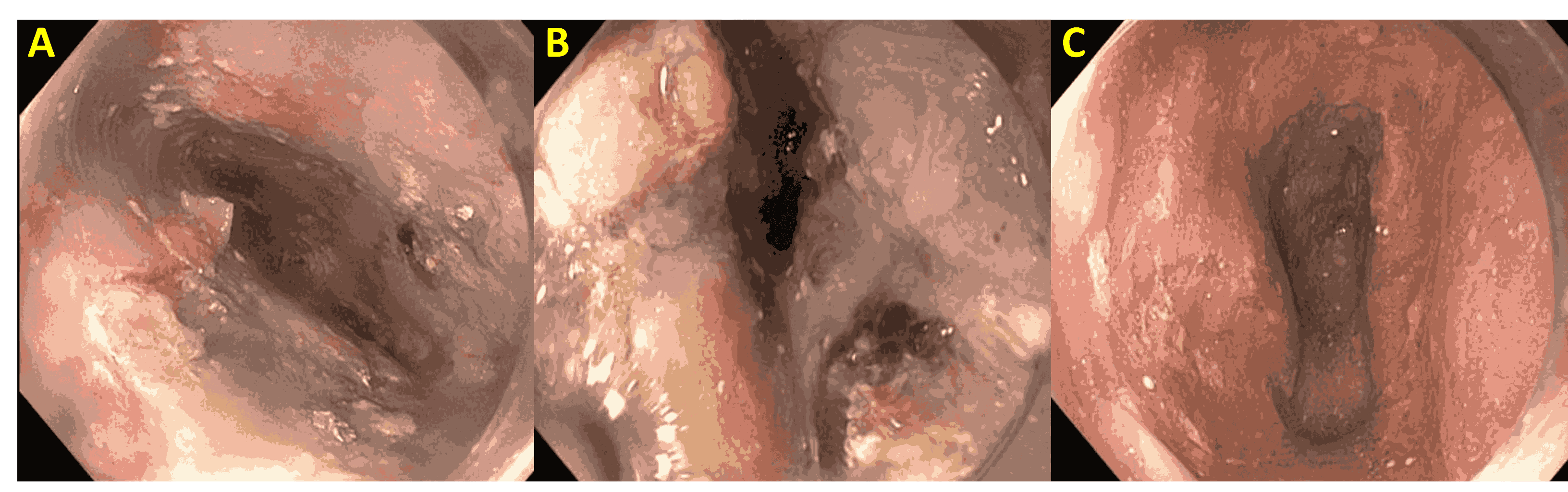
Figure: Figure 2. (A–B) Large esophageal ulcer with a clean base and overlying food debris. (C) Ischemic-appearing esophageal mucosa with sloughing observed following endoscope passage.
Disclosures:
Tsola Efejuku indicated no relevant financial relationships.
Manavi Bhagwat indicated no relevant financial relationships.
Himesh Zaver indicated no relevant financial relationships.
Nicola Litchfield indicated no relevant financial relationships.
Jeanetta Frye indicated no relevant financial relationships.
Tsola Efejuku, MD1, Manavi Bhagwat, MD1, Himesh Zaver, MD2, Nicola Litchfield, DO1, Jeanetta Frye, MD1. P0889 - An Unintended Consequence: Dysphagia Following Bronchial Artery Embolization for Recurrent Hemoptysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia Health, Charlottesville, VA
Introduction: Bronchial artery embolization (BAE) is a treatment for recurrent hemoptysis. Although adverse events are rare, we present a case of dysphagia caused by ischemic esophageal ulceration following BAE.
Case Description/
Methods: A 61-year-old female patient presented to a tertiary care center with hemoptysis. Past medical history was significant for paroxysmal atrial fibrillation and end-stage heart failure requiring a left ventricular assist device and warfarin anticoagulation. The patient had recurrent admissions for hemoptysis not amenable to standard hemostatic therapies via bronchoscopy. Following multidisciplinary discussion, the patient underwent catheter-directed BAE of her left bronchial artery for recurrent hemoptysis. One week after BAE procedure, the patient developed odynophagia and dysphagia to both solids and liquids, prompting gastrointestinal consultation. Initial evaluation included a barium esophagram, which was unremarkable except for a small hiatal hernia (Figure 1). The patient subsequently underwent esophagogastroduodenoscopy (EGD), which revealed a large esophageal ulcer (Figure 2A–B) surrounded by focal ischemic-appearing mucosa and food debris (Figure 2C), located approximately 25 cm from the incisors. The mucosa proximal and distal to the ulcer appeared normal and healthy. The ulcer and ischemic appearing mucosa were biopsied. Pathology was supportive of acute and chronic inflammation with reactive changes consistent with ischemia-related injury. Stains for fungal and viral pathogens were negative. The patient was started on a proton pump inhibitor and a low-residue dysphagia diet and was discharged home in stable condition.
Discussion: The major arteries supplying the esophagus include the inferior thyroid, bronchial, left gastric, and left phrenic arteries. In this case, BAE involving the left bronchial artery resulted in esophageal ischemia, leading to ulceration and esophageal symptoms. Although food debris was noted on EGD, the overall findings were not consistent with a stasis ulcer, underscoring the importance of avoiding anchoring bias in clinical interpretation. This case also emphasizes the importance of a thorough understanding of esophageal vascular anatomy and the careful collection of a detailed patient history to guide timely diagnosis and management.
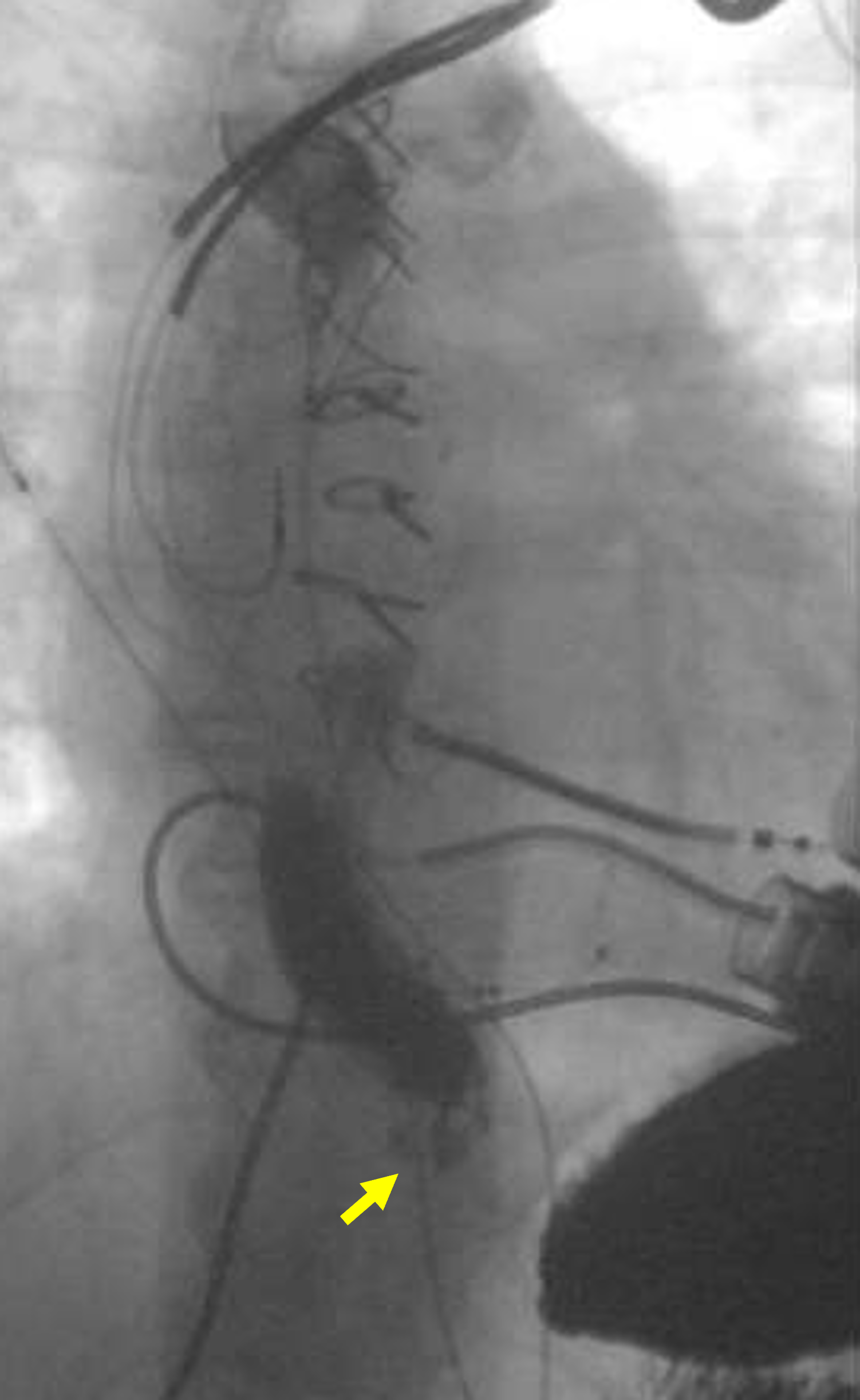
Figure: Figure 1. Barium esophagram suggestive of normal esophageal mucosa and small type I hiatal hernia (yellow arrow)
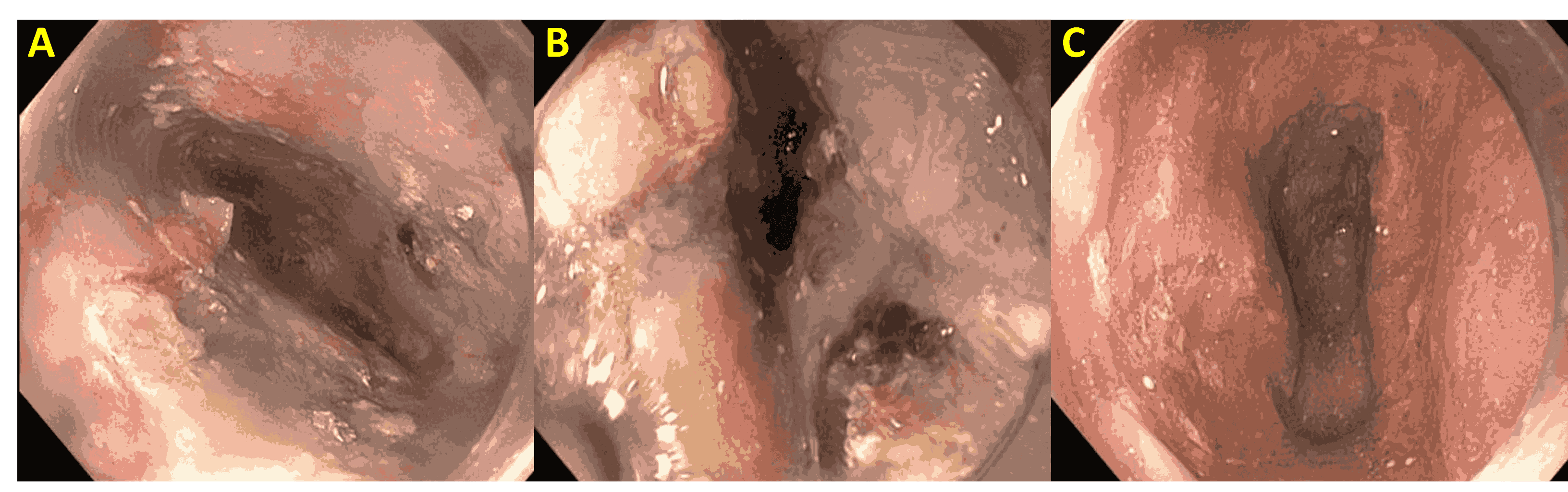
Figure: Figure 2. (A–B) Large esophageal ulcer with a clean base and overlying food debris. (C) Ischemic-appearing esophageal mucosa with sloughing observed following endoscope passage.
Disclosures:
Tsola Efejuku indicated no relevant financial relationships.
Manavi Bhagwat indicated no relevant financial relationships.
Himesh Zaver indicated no relevant financial relationships.
Nicola Litchfield indicated no relevant financial relationships.
Jeanetta Frye indicated no relevant financial relationships.
Tsola Efejuku, MD1, Manavi Bhagwat, MD1, Himesh Zaver, MD2, Nicola Litchfield, DO1, Jeanetta Frye, MD1. P0889 - An Unintended Consequence: Dysphagia Following Bronchial Artery Embolization for Recurrent Hemoptysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
