Sunday Poster Session
Category: General Endoscopy
P0880 - Removing the Benign on Routine Colonoscopy: A Rare Case of Appendiceal Inversion
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JO
Juan Ortiz Rodriguez, MD (he/him/his)
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Juan Ortiz Rodriguez, MD, Jessica Strzepka, MD, Omar Nehme, MD
Rush University Medical Center, Chicago, IL
Introduction: Appendiceal inversion (AI) is rare, with an incidence estimated at 0.01%. It is defined as appendiceal tissue pulled into itself or the cecal lumen. It is seen more commonly in females, patients with cystic fibrosis, and patients with history of appendectomy. AI raises a clinical conundrum for endoscopists, whose aim is to identify premalignant or malignant conditions on luminal evaluation, since its appearance can often appear similar to polyps or neoplasms. Reports in the literature suggest that tissue sampling or resection can lead to complications of bleeding, peritonitis, or perforation.
Case Description/
Methods: A 45-year-old female with history of sickle cell trait who presented for average risk colon cancer screening. Pertinent surgical history included a cesarian section. There was no family history of colon cancer. Colonoscopy revealed a 13 mm pedunculated polyp at the appendiceal orifice. Given granular appearance of mucosa, biopsy with cold forceps was obtained for sampling. This revealed friable mucosa and bleeding. Given persistent bleeding, lesion was resected with hot snare polypectomy followed by placement of three hemostatic clips. Patient was prescribed a five-day course of amoxicillin/clavulanic acid for infection prophylaxis and instructed to seek medical attention for infectious symptoms or bleeding signs. Upon follow-up, post procedural course remained unremarkable. The final pathology report showed nondysplastic colonic mucosa suggestive of inverted appendiceal tissue.
Discussion: AI is a rare condition, which if encountered on endoscopy, can raise questions regarding optimal management depending on size, mucosal characteristics, and patient risk factors. Unnecessary intervention on AI risks potential complications. However, inadequate sampling or removal of premalignant conditions can risk morbidity and mortality as well. We describe a case of attempted tissue sampling to rule out pathology given atypical mucosal appearance, which resulted in bleeding with subsequent resection and clip placement, of which histology later confirmed the lesion to be AI. There have been few similar cases reported in the recent literature. We highlight the need for careful consideration of risks and benefits of sampling and/or resection. Recent literature suggests that biopsy may be considered to rule out neoplastic processes, with cross sectional imaging being an alternative option. If intervention is completed, antibiotics can be considered to mitigate infection risk as in this case.
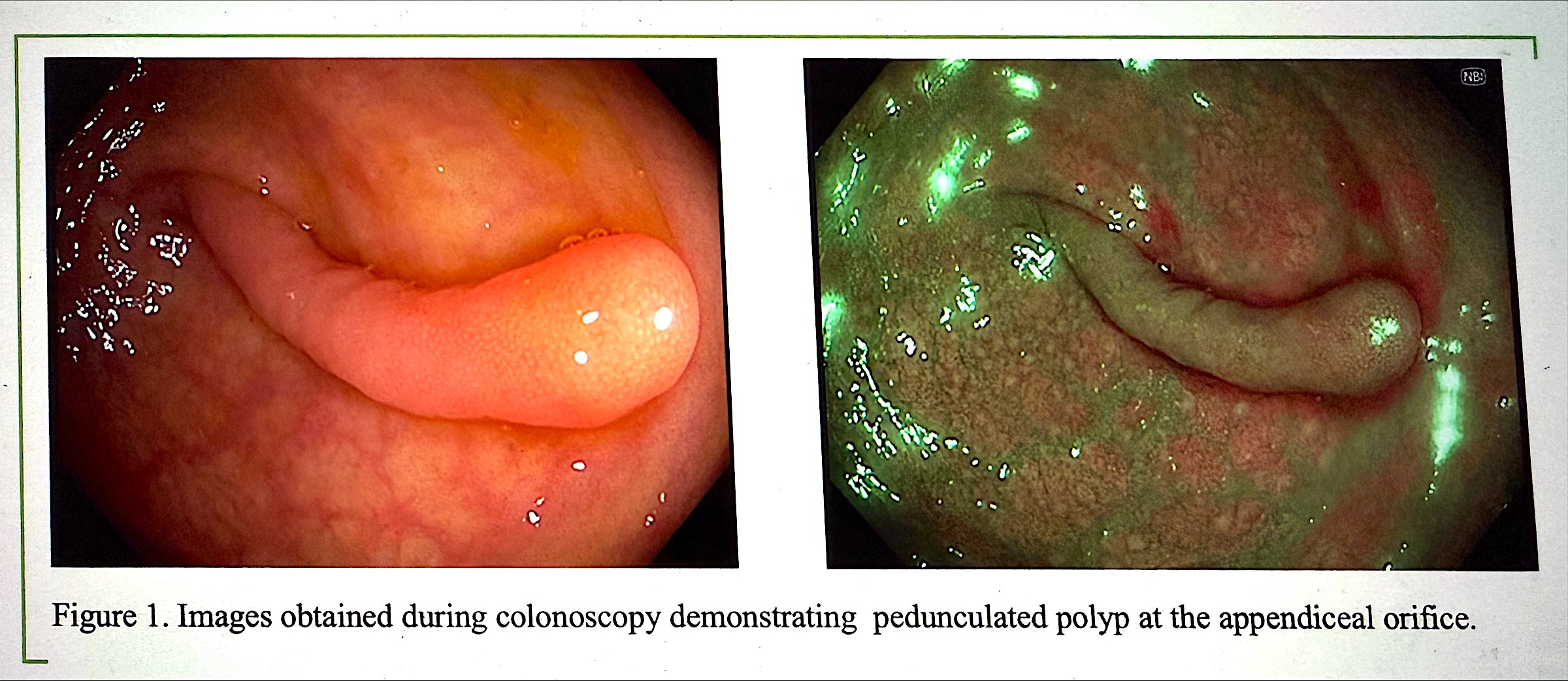
Figure: Figure 1. Pedunculated polyp at the appendiceal orifice
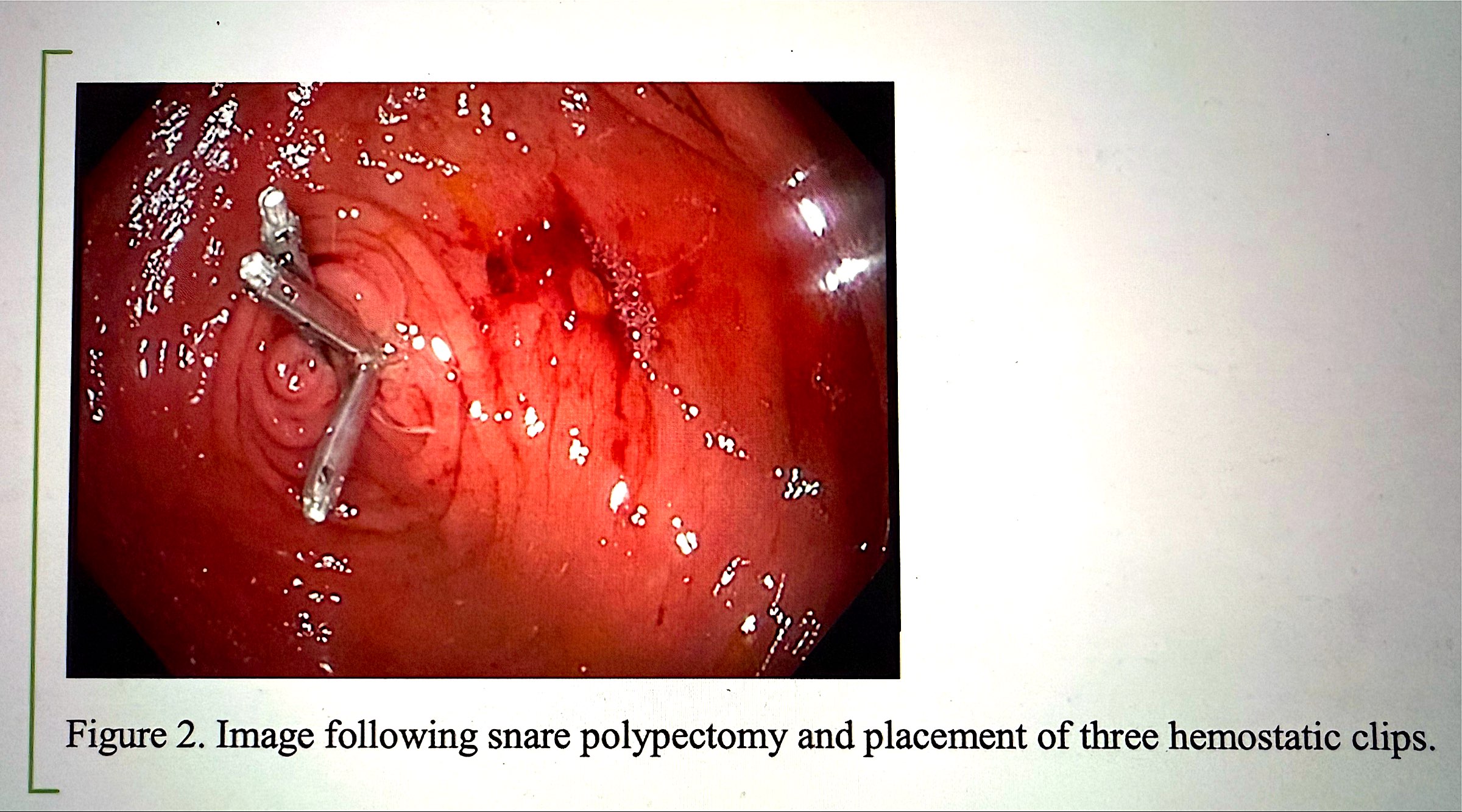
Figure: Figure 2. Status post snare polypectomy and placement of three hemostatic clips
Disclosures:
Juan Ortiz Rodriguez indicated no relevant financial relationships.
Jessica Strzepka indicated no relevant financial relationships.
Omar Nehme indicated no relevant financial relationships.
Juan Ortiz Rodriguez, MD, Jessica Strzepka, MD, Omar Nehme, MD. P0880 - Removing the Benign on Routine Colonoscopy: A Rare Case of Appendiceal Inversion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Rush University Medical Center, Chicago, IL
Introduction: Appendiceal inversion (AI) is rare, with an incidence estimated at 0.01%. It is defined as appendiceal tissue pulled into itself or the cecal lumen. It is seen more commonly in females, patients with cystic fibrosis, and patients with history of appendectomy. AI raises a clinical conundrum for endoscopists, whose aim is to identify premalignant or malignant conditions on luminal evaluation, since its appearance can often appear similar to polyps or neoplasms. Reports in the literature suggest that tissue sampling or resection can lead to complications of bleeding, peritonitis, or perforation.
Case Description/
Methods: A 45-year-old female with history of sickle cell trait who presented for average risk colon cancer screening. Pertinent surgical history included a cesarian section. There was no family history of colon cancer. Colonoscopy revealed a 13 mm pedunculated polyp at the appendiceal orifice. Given granular appearance of mucosa, biopsy with cold forceps was obtained for sampling. This revealed friable mucosa and bleeding. Given persistent bleeding, lesion was resected with hot snare polypectomy followed by placement of three hemostatic clips. Patient was prescribed a five-day course of amoxicillin/clavulanic acid for infection prophylaxis and instructed to seek medical attention for infectious symptoms or bleeding signs. Upon follow-up, post procedural course remained unremarkable. The final pathology report showed nondysplastic colonic mucosa suggestive of inverted appendiceal tissue.
Discussion: AI is a rare condition, which if encountered on endoscopy, can raise questions regarding optimal management depending on size, mucosal characteristics, and patient risk factors. Unnecessary intervention on AI risks potential complications. However, inadequate sampling or removal of premalignant conditions can risk morbidity and mortality as well. We describe a case of attempted tissue sampling to rule out pathology given atypical mucosal appearance, which resulted in bleeding with subsequent resection and clip placement, of which histology later confirmed the lesion to be AI. There have been few similar cases reported in the recent literature. We highlight the need for careful consideration of risks and benefits of sampling and/or resection. Recent literature suggests that biopsy may be considered to rule out neoplastic processes, with cross sectional imaging being an alternative option. If intervention is completed, antibiotics can be considered to mitigate infection risk as in this case.
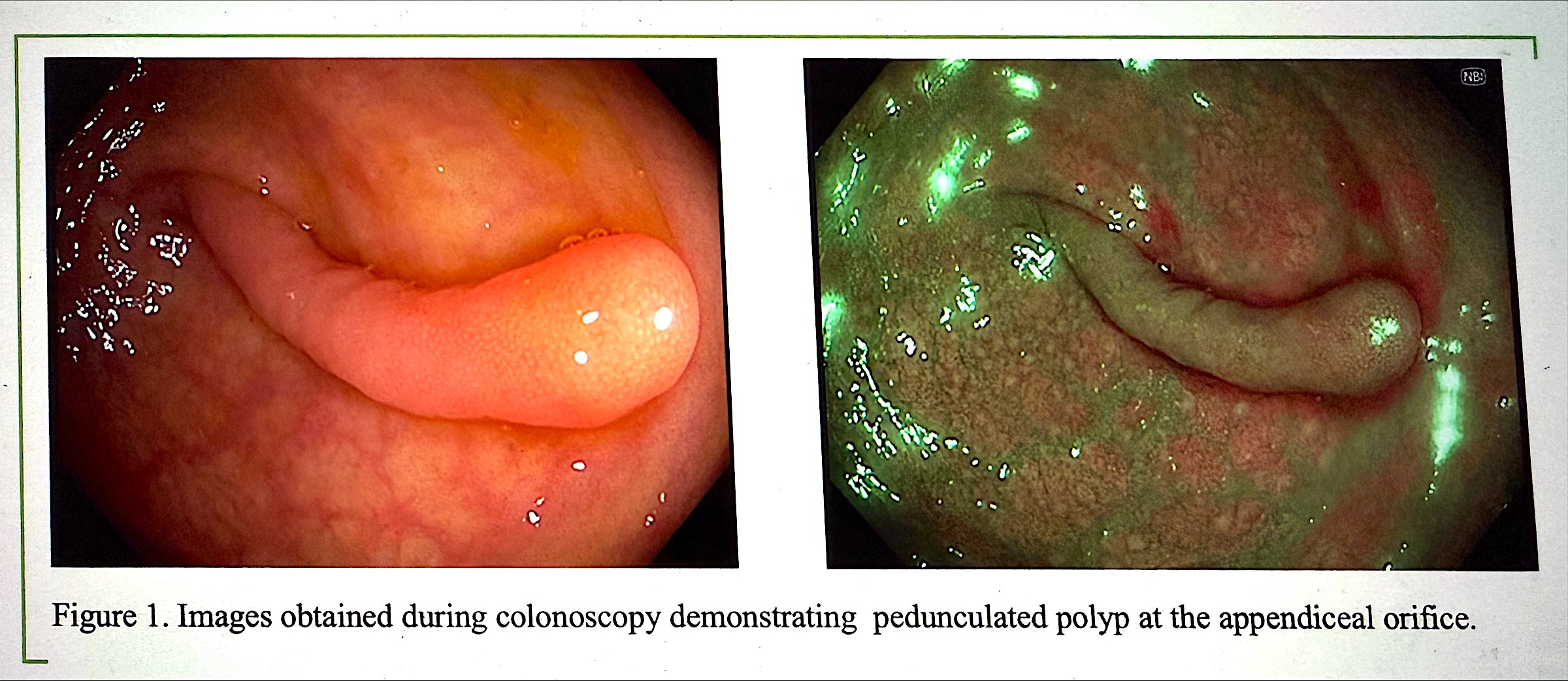
Figure: Figure 1. Pedunculated polyp at the appendiceal orifice
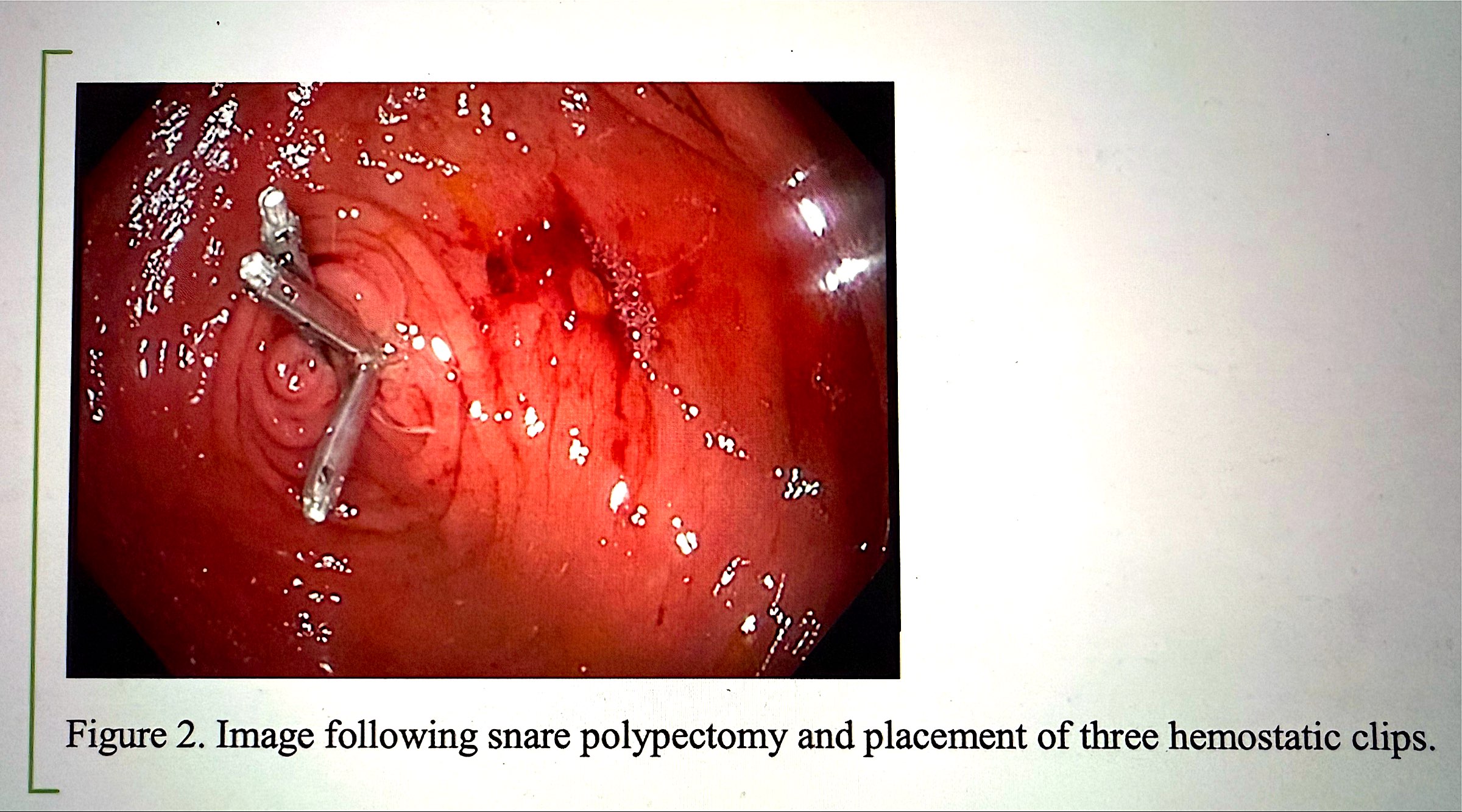
Figure: Figure 2. Status post snare polypectomy and placement of three hemostatic clips
Disclosures:
Juan Ortiz Rodriguez indicated no relevant financial relationships.
Jessica Strzepka indicated no relevant financial relationships.
Omar Nehme indicated no relevant financial relationships.
Juan Ortiz Rodriguez, MD, Jessica Strzepka, MD, Omar Nehme, MD. P0880 - Removing the Benign on Routine Colonoscopy: A Rare Case of Appendiceal Inversion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
