Sunday Poster Session
Category: General Endoscopy
P0874 - Successful Conservative Management of Buried Bumper Syndrome
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- ZI
Zaid Imam, MBBS (he/him/his)
Washington Township Medical Group
Mountain View, CA
Presenting Author(s)
Hiba Ghannam, MD1, Keenan Kassar, MBA2, Abdulhadi Abo Nofal, 3, Zaid Imam, MD4
1Health Point Abudhabi, Abudhabi, Abu Dhabi, United Arab Emirates; 2Loyola University, Lemont, IL; 3Alfaisal University, Riyadh, Ar Riyad, Saudi Arabia; 4Washington Hospital Healthcare System, Mountain View, CA
Introduction: Buried bumper syndrome (BPS) is a rare complication of percutaneous endoscopic gastrostomy (PEG) placement with an estimated incidence of 0.3-2.4%. We hereby report a case of BPS managed successfully by post-enteral nutrition and loosening of the bumper highlighting the importance of early recognition of this serious complication.
Case Description/
Methods: A 31-year-old-Asian male with no prior medical history was admitted as a victim of a motor vehicle accident complicated by subarachnoid hemorrhage. Prolonged oropharyngeal dysphagia necessitated placement of a PEG tube on admission day 10. On day 16, he developed low grade fevers with cellulitis overlying the PEG tube. On examination, the PEG site was indurated and erythematous, the PEG tube was not easily rotatable and was loosened at the bedside. A computed tomography of the abdomen demonstrated no evidence of peritonitis, no abscess but evidence of diffuse subcutaneous edema around the PEG site. BPS was suspected, and an esophagogastroduodenoscopy (EGD) was performed demonstrating a buried bumper that was loosened further (Panel A) and a nasoduodenal tube was placed under endoscopic guidance. Given this developed 6 days following initial placement, concerns about tract maturity and absence of perforation favored a trial of conservative management. The PEG tube was connected to dependent drainage, with a reinforced dressing pushing the tube inwards to avoid re-burying of the bumper in the ulcerated area of the stomach and nasoduodenal feeding was utilized. The patient clinically improved within 48 hours with resolution of cellulitis, fevers and leukocytosis. A repeat EGD 14 days from the initial procedure demonstrated significant healing (Panel B). The nasoduodenal tube was removed, and the gastrostomy tube was used for enteral access. He was discharged in stable condition and on interval follow-up 2 months later, no recurrence of gastrostomy site cellulitis or other PEG related complications were noted.
Discussion: This case highlights a rare complication of BPS presenting early post-PEG placement with cellulitis and where early recognition and conservative management with gastric decompression, post-pyloric feeding, antibiotics and close monitoring was successful.
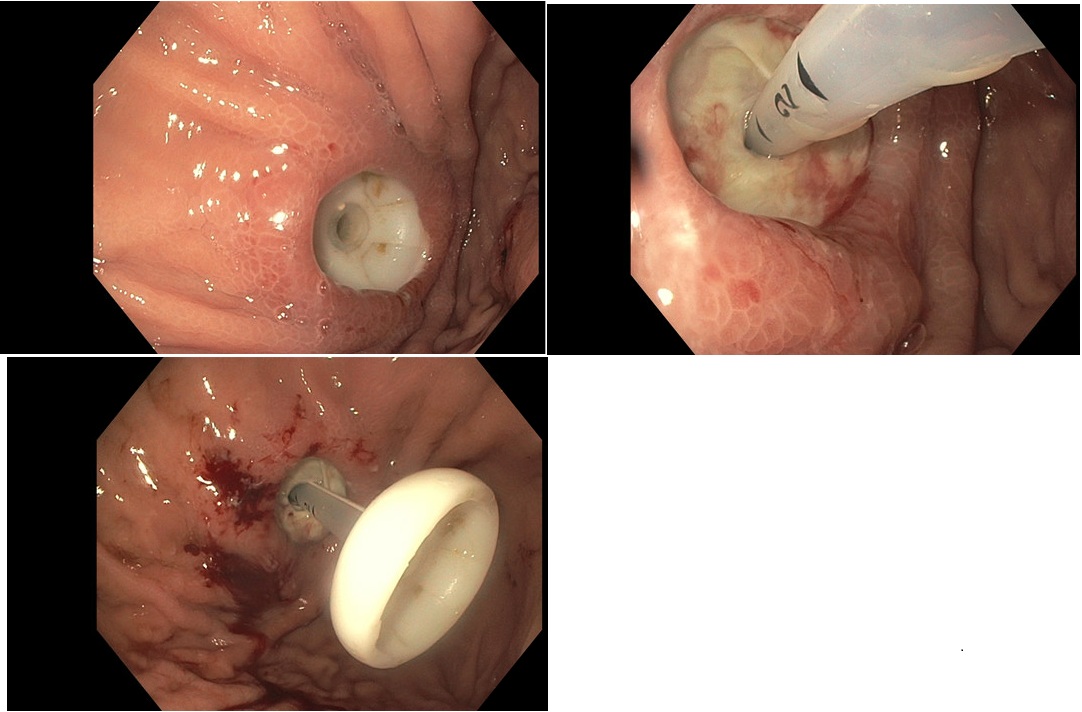
Figure: Panel A: First esophagogastroduodenoscopy demonstrating a buried bumper syndrome with no evidence of gastric perforation and a deeply cratered ulcer at the bumper site

Figure: Panel B: Follow-up esophagogastroduodenoscopy 14 days later with significant healing of the prior ulceration, gastrostomy used for enteral access following this procedure
Disclosures:
Hiba Ghannam indicated no relevant financial relationships.
Keenan Kassar indicated no relevant financial relationships.
Abdulhadi Abo Nofal indicated no relevant financial relationships.
Zaid Imam indicated no relevant financial relationships.
Hiba Ghannam, MD1, Keenan Kassar, MBA2, Abdulhadi Abo Nofal, 3, Zaid Imam, MD4. P0874 - Successful Conservative Management of Buried Bumper Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Health Point Abudhabi, Abudhabi, Abu Dhabi, United Arab Emirates; 2Loyola University, Lemont, IL; 3Alfaisal University, Riyadh, Ar Riyad, Saudi Arabia; 4Washington Hospital Healthcare System, Mountain View, CA
Introduction: Buried bumper syndrome (BPS) is a rare complication of percutaneous endoscopic gastrostomy (PEG) placement with an estimated incidence of 0.3-2.4%. We hereby report a case of BPS managed successfully by post-enteral nutrition and loosening of the bumper highlighting the importance of early recognition of this serious complication.
Case Description/
Methods: A 31-year-old-Asian male with no prior medical history was admitted as a victim of a motor vehicle accident complicated by subarachnoid hemorrhage. Prolonged oropharyngeal dysphagia necessitated placement of a PEG tube on admission day 10. On day 16, he developed low grade fevers with cellulitis overlying the PEG tube. On examination, the PEG site was indurated and erythematous, the PEG tube was not easily rotatable and was loosened at the bedside. A computed tomography of the abdomen demonstrated no evidence of peritonitis, no abscess but evidence of diffuse subcutaneous edema around the PEG site. BPS was suspected, and an esophagogastroduodenoscopy (EGD) was performed demonstrating a buried bumper that was loosened further (Panel A) and a nasoduodenal tube was placed under endoscopic guidance. Given this developed 6 days following initial placement, concerns about tract maturity and absence of perforation favored a trial of conservative management. The PEG tube was connected to dependent drainage, with a reinforced dressing pushing the tube inwards to avoid re-burying of the bumper in the ulcerated area of the stomach and nasoduodenal feeding was utilized. The patient clinically improved within 48 hours with resolution of cellulitis, fevers and leukocytosis. A repeat EGD 14 days from the initial procedure demonstrated significant healing (Panel B). The nasoduodenal tube was removed, and the gastrostomy tube was used for enteral access. He was discharged in stable condition and on interval follow-up 2 months later, no recurrence of gastrostomy site cellulitis or other PEG related complications were noted.
Discussion: This case highlights a rare complication of BPS presenting early post-PEG placement with cellulitis and where early recognition and conservative management with gastric decompression, post-pyloric feeding, antibiotics and close monitoring was successful.
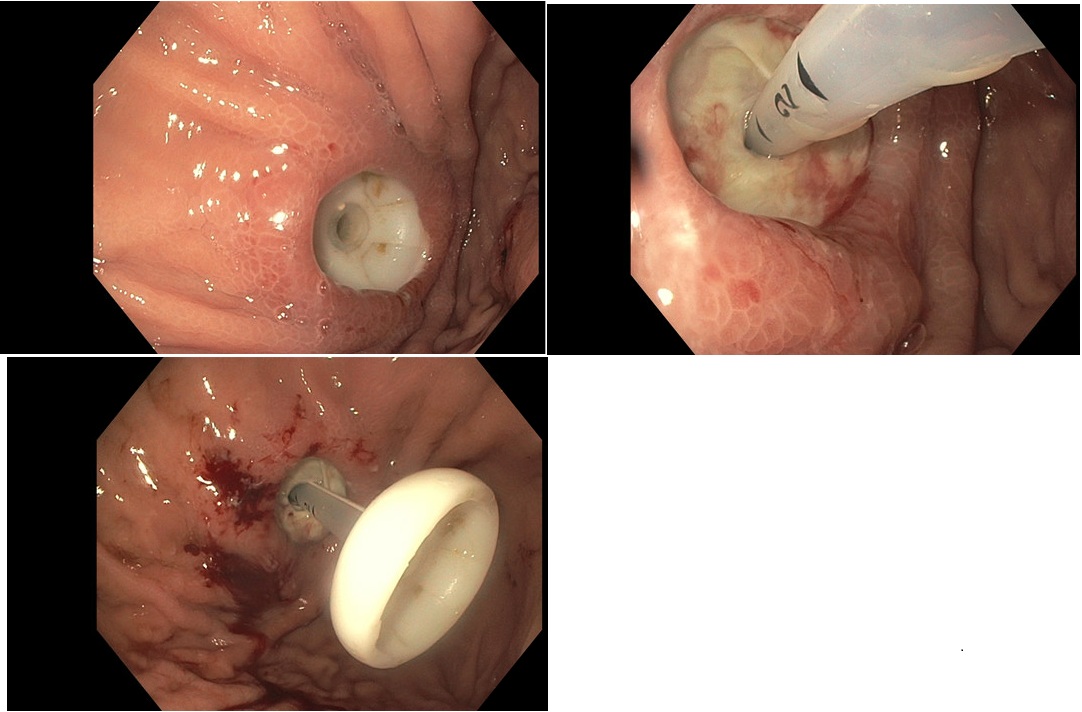
Figure: Panel A: First esophagogastroduodenoscopy demonstrating a buried bumper syndrome with no evidence of gastric perforation and a deeply cratered ulcer at the bumper site

Figure: Panel B: Follow-up esophagogastroduodenoscopy 14 days later with significant healing of the prior ulceration, gastrostomy used for enteral access following this procedure
Disclosures:
Hiba Ghannam indicated no relevant financial relationships.
Keenan Kassar indicated no relevant financial relationships.
Abdulhadi Abo Nofal indicated no relevant financial relationships.
Zaid Imam indicated no relevant financial relationships.
Hiba Ghannam, MD1, Keenan Kassar, MBA2, Abdulhadi Abo Nofal, 3, Zaid Imam, MD4. P0874 - Successful Conservative Management of Buried Bumper Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
