Sunday Poster Session
Category: General Endoscopy
P0865 - Trends and Disparities in Esophagogastroduodenoscopy Utilization for Dyspepsia Admissions: A Six Year US National Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Abhin Sapkota, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Abhin Sapkota, MD1, Kriti Katwal, 2, Saksham Kohli, MBBS1, Gedion Amdetsion, MD1, Maria Grba, MD1, Seema R. Gandhi, MD3
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lumbini Medical College, Palpa, Lumbini, Nepal; 3Cook County Health, Chicago, IL
Introduction: Dyspepsia is a common gastrointestinal complaint which accounts for a significant proportion of healthcare visits. The role of esophagogastroduodenoscopy (EGD) in dyspepsia, remains controversial due to its invasive nature and associated costs. Guidelines recommend EGD for dyspepsia with alarm features or in older patients. However, the real-world application of these guidelines in the inpatient setting remain unclear. This study aims to investigate utilization of EGD for dyspepsia admissions.
Methods: A retrospective cohort study was conducted using the National Inpatient Sample database (2016–2021) to identify dyspepsia as a primary diagnosis using appropriate International Classification of Diseases, 10th Revision (ICD-10) codes. EGD utilization was determined using ICD-10 procedure codes and analyzed using survey-weighted descriptive statistics and multivariable logistic regression. Longitudinal analysis was done and statistical significance was set at p < 0.05.
Results: Among 63,255 dyspepsia-related hospitalizations, 5,905 (9.33%) underwent EGD. Those who underwent EGD were slightly younger and had a higher proportion of females. EGD cohort had longer length of stay (LOS) (3.43 vs. 2.55 days, p< 0.001) and higher total charges ($37,855 vs. $30,154, p< 0.001). Patients with Medicaid(aOR: 0.62, p=0.001), Private insurance (aOR: 0.76, p=0.005) and Self-pay (aOR: 0.52, p=0.051) had lower odds of EGD use compared to Medicare. Midwest region had higher odds (aOR: 1.34, p=0.003) compared to Northwest. Medium (aOR: 1.33, p=0.003) and large (aOR: 1.36, p=0.001) size hospitals had higher odds compared to small size. There was a modest decrease in EGD utilization from 9.7% in 2016 to 7.7% in 2021.
Discussion: EGD is performed in a minority of dyspepsia cases, consistent with guidelines recommendations. However, its association with longer LOS and higher costs highlights the need for better-defined inpatient criteria. The similar comorbidity burden between both cohorts suggests that disease severity alone does not dictate EGD use. Medicaid and self-pay patients were less likely to undergo EGD compared to Medicare beneficiaries, suggesting potential financial barriers. Larger hospitals had higher EGD utilization, possibly due to greater availability of endoscopic services. The overall decline in EGD use over time may reflect evolving management strategies. Addressing these disparities through policy initiatives and appropriate resource allocation is crucial to ensuring equitable access to EGD.
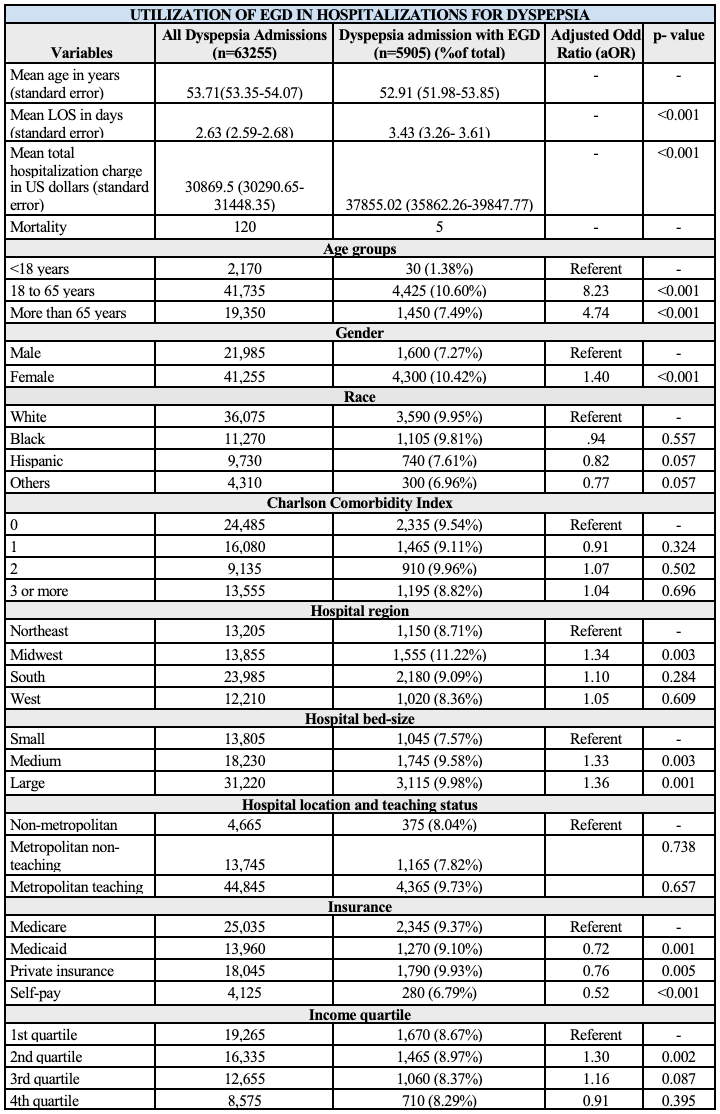
Figure: Table 1. Sociodemographic distribution of Esophagogastroduodenoscopy use in Dyspepsia Admissions.
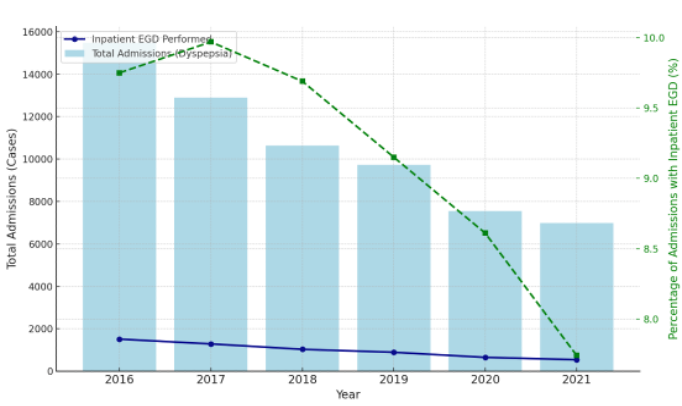
Figure: Figure 1. Trends in total Dyspepsia Admissions and Esophagogastroduodenoscopy use over the years.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Kriti Katwal indicated no relevant financial relationships.
Saksham Kohli indicated no relevant financial relationships.
Gedion Amdetsion indicated no relevant financial relationships.
Maria Grba indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Abhin Sapkota, MD1, Kriti Katwal, 2, Saksham Kohli, MBBS1, Gedion Amdetsion, MD1, Maria Grba, MD1, Seema R. Gandhi, MD3. P0865 - Trends and Disparities in Esophagogastroduodenoscopy Utilization for Dyspepsia Admissions: A Six Year US National Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lumbini Medical College, Palpa, Lumbini, Nepal; 3Cook County Health, Chicago, IL
Introduction: Dyspepsia is a common gastrointestinal complaint which accounts for a significant proportion of healthcare visits. The role of esophagogastroduodenoscopy (EGD) in dyspepsia, remains controversial due to its invasive nature and associated costs. Guidelines recommend EGD for dyspepsia with alarm features or in older patients. However, the real-world application of these guidelines in the inpatient setting remain unclear. This study aims to investigate utilization of EGD for dyspepsia admissions.
Methods: A retrospective cohort study was conducted using the National Inpatient Sample database (2016–2021) to identify dyspepsia as a primary diagnosis using appropriate International Classification of Diseases, 10th Revision (ICD-10) codes. EGD utilization was determined using ICD-10 procedure codes and analyzed using survey-weighted descriptive statistics and multivariable logistic regression. Longitudinal analysis was done and statistical significance was set at p < 0.05.
Results: Among 63,255 dyspepsia-related hospitalizations, 5,905 (9.33%) underwent EGD. Those who underwent EGD were slightly younger and had a higher proportion of females. EGD cohort had longer length of stay (LOS) (3.43 vs. 2.55 days, p< 0.001) and higher total charges ($37,855 vs. $30,154, p< 0.001). Patients with Medicaid(aOR: 0.62, p=0.001), Private insurance (aOR: 0.76, p=0.005) and Self-pay (aOR: 0.52, p=0.051) had lower odds of EGD use compared to Medicare. Midwest region had higher odds (aOR: 1.34, p=0.003) compared to Northwest. Medium (aOR: 1.33, p=0.003) and large (aOR: 1.36, p=0.001) size hospitals had higher odds compared to small size. There was a modest decrease in EGD utilization from 9.7% in 2016 to 7.7% in 2021.
Discussion: EGD is performed in a minority of dyspepsia cases, consistent with guidelines recommendations. However, its association with longer LOS and higher costs highlights the need for better-defined inpatient criteria. The similar comorbidity burden between both cohorts suggests that disease severity alone does not dictate EGD use. Medicaid and self-pay patients were less likely to undergo EGD compared to Medicare beneficiaries, suggesting potential financial barriers. Larger hospitals had higher EGD utilization, possibly due to greater availability of endoscopic services. The overall decline in EGD use over time may reflect evolving management strategies. Addressing these disparities through policy initiatives and appropriate resource allocation is crucial to ensuring equitable access to EGD.
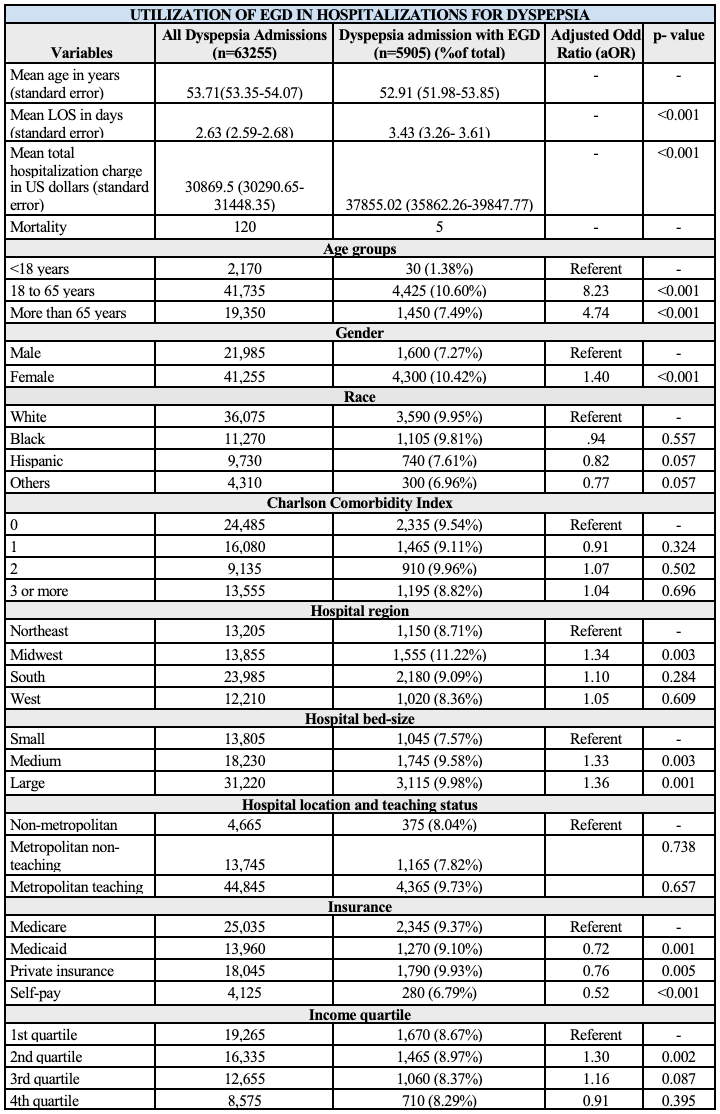
Figure: Table 1. Sociodemographic distribution of Esophagogastroduodenoscopy use in Dyspepsia Admissions.
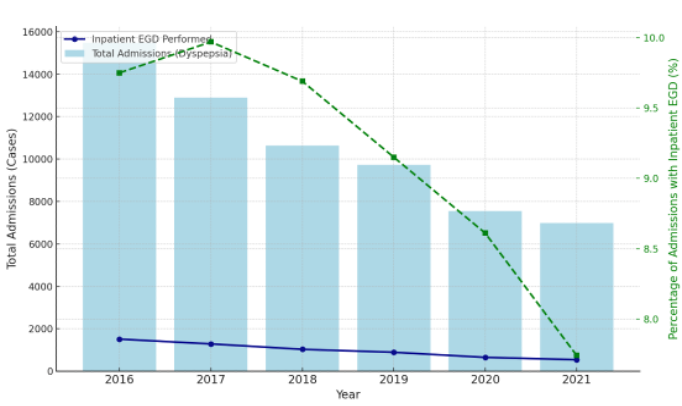
Figure: Figure 1. Trends in total Dyspepsia Admissions and Esophagogastroduodenoscopy use over the years.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Kriti Katwal indicated no relevant financial relationships.
Saksham Kohli indicated no relevant financial relationships.
Gedion Amdetsion indicated no relevant financial relationships.
Maria Grba indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Abhin Sapkota, MD1, Kriti Katwal, 2, Saksham Kohli, MBBS1, Gedion Amdetsion, MD1, Maria Grba, MD1, Seema R. Gandhi, MD3. P0865 - Trends and Disparities in Esophagogastroduodenoscopy Utilization for Dyspepsia Admissions: A Six Year US National Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
