Sunday Poster Session
Category: Functional Bowel Disease
P0822 - Real-World Effectiveness of the Low FODMAP Diet vs Other Therapeutic Diet Interventions for Functional Gastrointestinal Disorders, Under Guidance of a Registered Dietitian
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Darshil Choksi, MD
University of Texas at Austin Dell Medical School
Austni, TX
Presenting Author(s)
Darshil Choksi, MD1, Noah Fanous, MD2, Srivani Mandaloju, MPH2, Kaeli Kampschmidt, BS3, Clara DiVincenzo, RD3, Linda A. Feagins, MD2
1University of Texas at Austin Dell Medical School, Austni, TX; 2University of Texas at Austin Dell Medical School, Austin, TX; 3University of Texas at Austin, Austin, TX
Introduction: A low FODMAP diet (LFD) is commonly used to improve gastrointestinal (GI) symptoms for patients with a variety of functional GI disorders (FGID), including irritable bowel syndrome (IBS). The LFD is not straightforward, and data suggests that using an experienced dietitian to implement this diet increases success. The aim of this study was to assess the effectiveness of LFD in real world GI practice with an embedded dietitian and to compare this to other dietary interventions employed for these disorders.
Methods: Adult patients seen in a GI practice with a dedicated registered dietitian between 1/1/2021 to 12/31/2023 who were referred to the dietitian with a diagnosis where a LFD was considered were evaluated for eligibility. Cases were patients who underwent a LFD trial while controls were those who decided along with the dietitian to not undertake a LFD and instead underwent other dietary changes (avoiding trigger foods, augmenting fiber intake, improving mealtime habits). Patients already on a LFD or without adequate follow up were excluded. Symptoms were categorized into 8 groups based on the GI PROMIS symptom scale and assessed pre- and post-intervention.
Results: We identified 58 cases and 144 controls (Table 1). Of cases, 48 (83%) successfully completed phase 1 of the LFD, 14 (24%) phase 2, and 3 (5.2%) phase 3. The most common symptoms were gas/bloating (82%), abdominal pain (66%), and diarrhea (50%). At baseline, both groups had a similar number of symptoms (3.17 vs 2.95, p=0.17). By 6 months, both had similar rates of having at least 1 symptom improved (40% vs 36%, p=0.64) and at least 1 symptom resolved (28% vs 22.9%, p=0.48). The overall number of symptoms resolved was similar (0.51 vs 0.38, p=0.34). Success rates of improving individual symptoms were also similar, except for the control group having greater improvement in reflux symptoms (Table 2).
Discussion: Most patients who pursued the LFD were able to successfully complete the first phase under dietitian guidance. Over half of the patients who completed the LFD achieved improvement in at least 1 symptom. Those who opted for alternative diet interventions, demonstrated improvements in symptoms at rates similar to those who had pursued the LFD. This data suggests that, while the LFD is an effective therapeutic approach to FGID, patients who are unable or unwilling to follow a LFD can still benefit from other therapeutic diet adjustments, under the careful management of a dietitian.
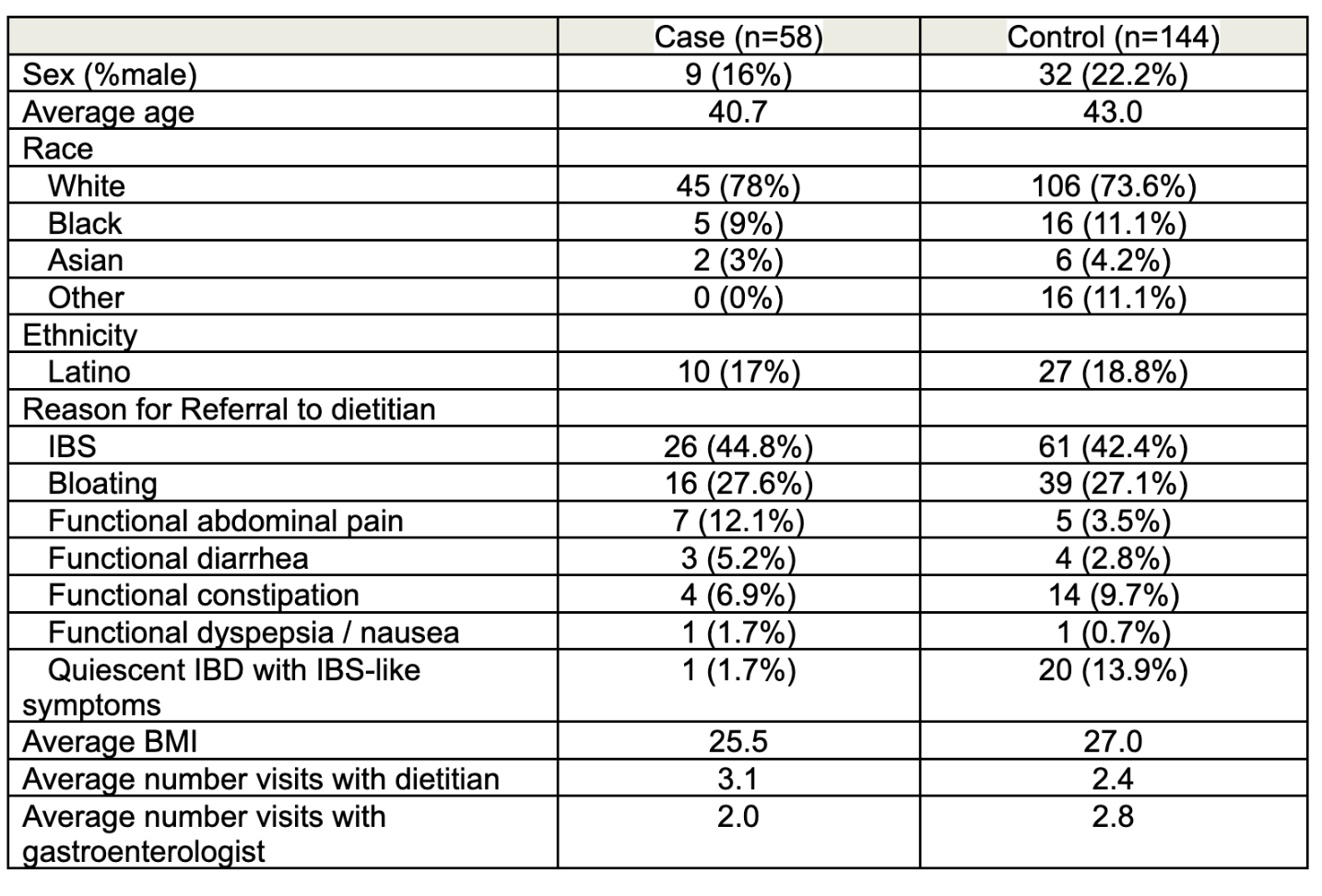
Figure: Table 1. Patient Baseline and GI Disease Characteristics Compared between Cases (Those Who Underwent a Low FODMAP trial) and Controls.
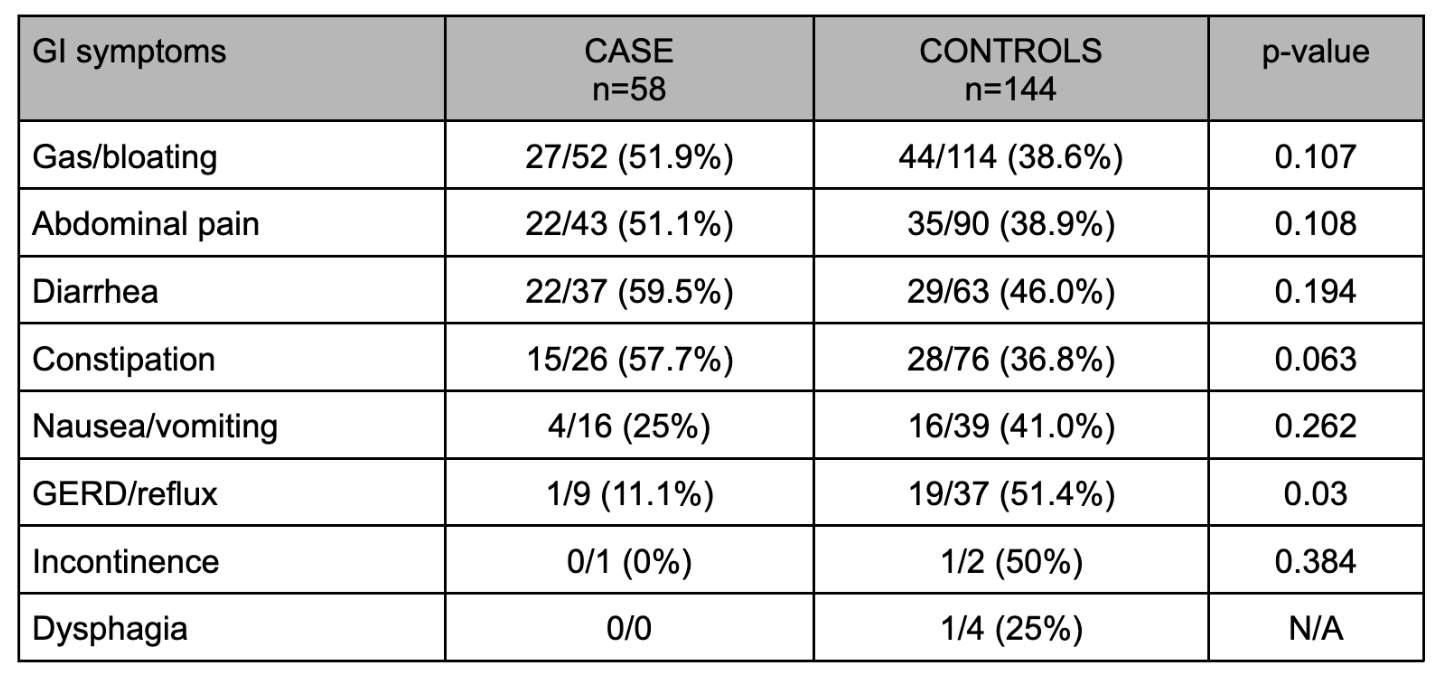
Figure: Table 2: Patients with baseline GI symptoms, categorized using the GI PROMIS symptom scale, who attained at least partial improvement after 6 months of diet intervention compared between cases and controls.
Disclosures:
Darshil Choksi indicated no relevant financial relationships.
Noah Fanous indicated no relevant financial relationships.
Srivani Mandaloju indicated no relevant financial relationships.
Kaeli Kampschmidt indicated no relevant financial relationships.
Clara DiVincenzo indicated no relevant financial relationships.
Linda Feagins: Corevitas – Clinical trial participation. Takeda – Clinical trial participation.
Darshil Choksi, MD1, Noah Fanous, MD2, Srivani Mandaloju, MPH2, Kaeli Kampschmidt, BS3, Clara DiVincenzo, RD3, Linda A. Feagins, MD2. P0822 - Real-World Effectiveness of the Low FODMAP Diet vs Other Therapeutic Diet Interventions for Functional Gastrointestinal Disorders, Under Guidance of a Registered Dietitian, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas at Austin Dell Medical School, Austni, TX; 2University of Texas at Austin Dell Medical School, Austin, TX; 3University of Texas at Austin, Austin, TX
Introduction: A low FODMAP diet (LFD) is commonly used to improve gastrointestinal (GI) symptoms for patients with a variety of functional GI disorders (FGID), including irritable bowel syndrome (IBS). The LFD is not straightforward, and data suggests that using an experienced dietitian to implement this diet increases success. The aim of this study was to assess the effectiveness of LFD in real world GI practice with an embedded dietitian and to compare this to other dietary interventions employed for these disorders.
Methods: Adult patients seen in a GI practice with a dedicated registered dietitian between 1/1/2021 to 12/31/2023 who were referred to the dietitian with a diagnosis where a LFD was considered were evaluated for eligibility. Cases were patients who underwent a LFD trial while controls were those who decided along with the dietitian to not undertake a LFD and instead underwent other dietary changes (avoiding trigger foods, augmenting fiber intake, improving mealtime habits). Patients already on a LFD or without adequate follow up were excluded. Symptoms were categorized into 8 groups based on the GI PROMIS symptom scale and assessed pre- and post-intervention.
Results: We identified 58 cases and 144 controls (Table 1). Of cases, 48 (83%) successfully completed phase 1 of the LFD, 14 (24%) phase 2, and 3 (5.2%) phase 3. The most common symptoms were gas/bloating (82%), abdominal pain (66%), and diarrhea (50%). At baseline, both groups had a similar number of symptoms (3.17 vs 2.95, p=0.17). By 6 months, both had similar rates of having at least 1 symptom improved (40% vs 36%, p=0.64) and at least 1 symptom resolved (28% vs 22.9%, p=0.48). The overall number of symptoms resolved was similar (0.51 vs 0.38, p=0.34). Success rates of improving individual symptoms were also similar, except for the control group having greater improvement in reflux symptoms (Table 2).
Discussion: Most patients who pursued the LFD were able to successfully complete the first phase under dietitian guidance. Over half of the patients who completed the LFD achieved improvement in at least 1 symptom. Those who opted for alternative diet interventions, demonstrated improvements in symptoms at rates similar to those who had pursued the LFD. This data suggests that, while the LFD is an effective therapeutic approach to FGID, patients who are unable or unwilling to follow a LFD can still benefit from other therapeutic diet adjustments, under the careful management of a dietitian.
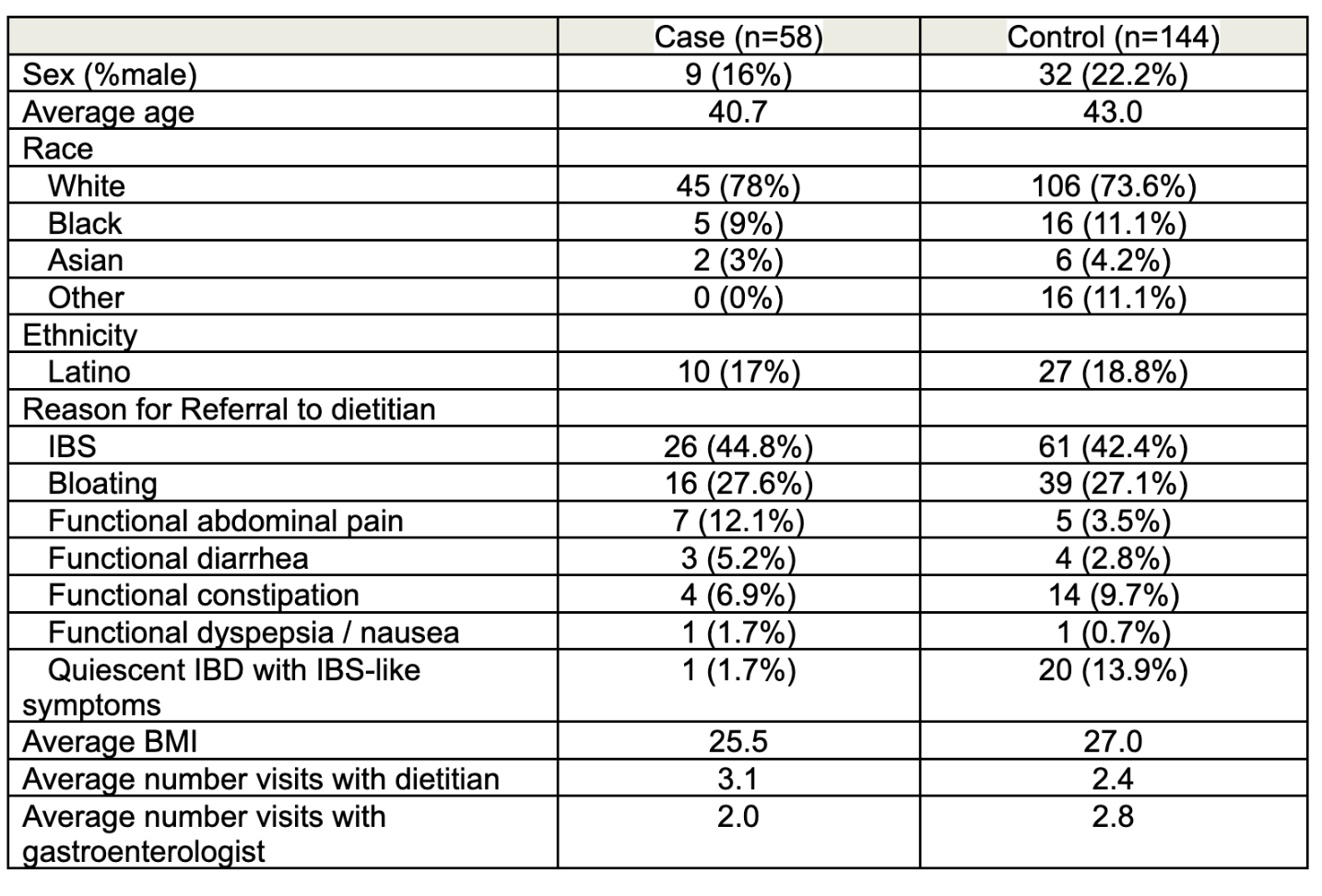
Figure: Table 1. Patient Baseline and GI Disease Characteristics Compared between Cases (Those Who Underwent a Low FODMAP trial) and Controls.
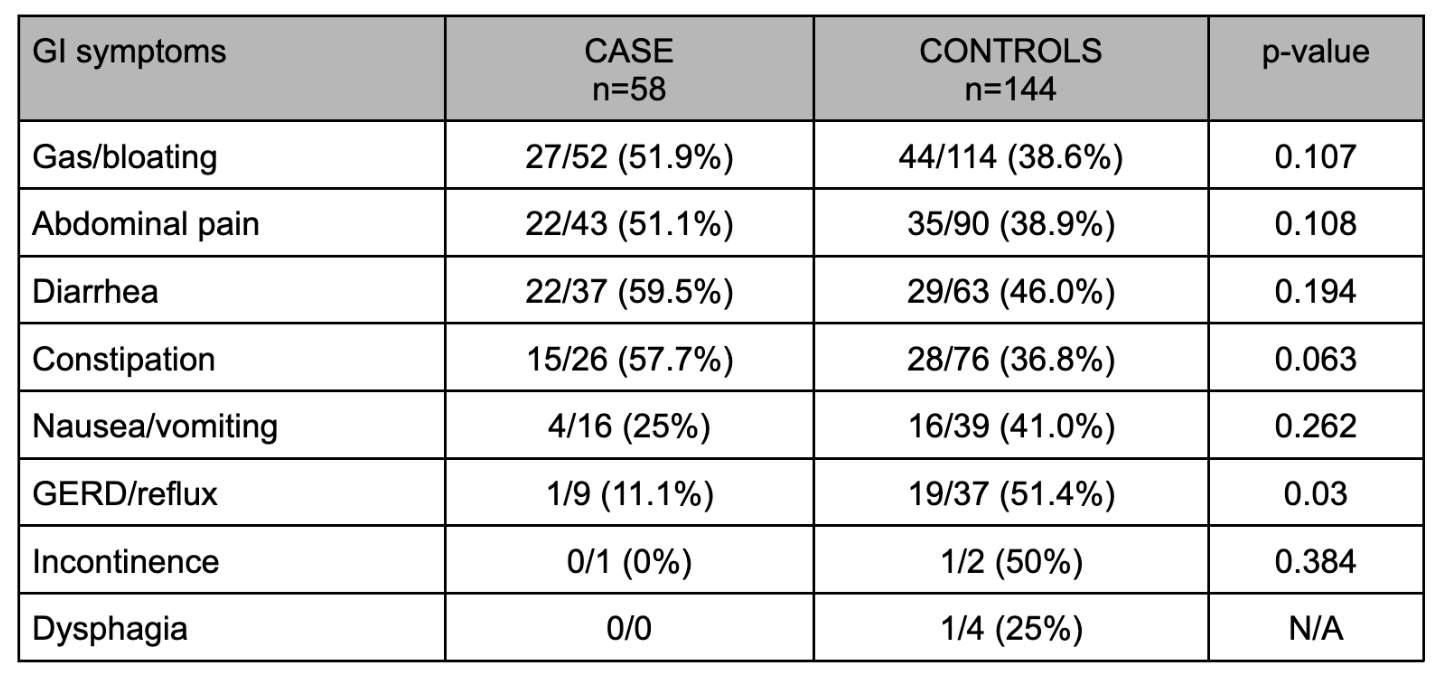
Figure: Table 2: Patients with baseline GI symptoms, categorized using the GI PROMIS symptom scale, who attained at least partial improvement after 6 months of diet intervention compared between cases and controls.
Disclosures:
Darshil Choksi indicated no relevant financial relationships.
Noah Fanous indicated no relevant financial relationships.
Srivani Mandaloju indicated no relevant financial relationships.
Kaeli Kampschmidt indicated no relevant financial relationships.
Clara DiVincenzo indicated no relevant financial relationships.
Linda Feagins: Corevitas – Clinical trial participation. Takeda – Clinical trial participation.
Darshil Choksi, MD1, Noah Fanous, MD2, Srivani Mandaloju, MPH2, Kaeli Kampschmidt, BS3, Clara DiVincenzo, RD3, Linda A. Feagins, MD2. P0822 - Real-World Effectiveness of the Low FODMAP Diet vs Other Therapeutic Diet Interventions for Functional Gastrointestinal Disorders, Under Guidance of a Registered Dietitian, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

