Sunday Poster Session
Category: Functional Bowel Disease
P0808 - Investigation of Osmotically Active Contrast Solutions in the Quantification of Visceral Hypersensitivity: A Prospective Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- RG
Riya Gupta, MBBS (she/her/hers)
Mayo Clinic
Phoenix, AZ
Presenting Author(s)
Riya Gupta, MBBS1, David J. Bartlett, MD1, Victor Chedid, MD, MSc1, Moataz Aboeldahb, MBBCh2, Xiao Jing Wang, MD1
1Mayo Clinic, Rochester, MN; 2Mayo Clinic College of Medicine and Science, Rochester, MN
Introduction: Visceral hypersensitivity (VH) is a key component of many disorders of gut-brain interaction (DGBIs), including functional dyspepsia (FD) and irritable bowel syndrome (IBS). Existing tests of VH in DGBIs, like rectal or jejunal barostat, are invasive, expensive, and limited to specialized centers. As such, objective diagnosis of VH remains elusive. CT enterography (CTE), used to assess small bowel pathology, utilizes oral, osmotically active mannitol and sorbitol-based agent as neutral contrast timed for small bowel distension and can cause gastrointestinal (GI) symptoms. This study investigates the utility of contrast-induced symptoms as a noninvasive biomarker for VH in DGBIs, particularly in the small bowel.
Methods: A prospective study was conducted at a tertiary care center among patients undergoing CTE for various indications. GI symptom burden was assessed using questionnaires before (–24h), immediately after (0h), and at 4–24h post-CTE. Demographics were extracted from electronic health records. Patients were categorized as IBS, FD, both, or neither (No DBGI) based on a prospectively administered abridged bowel disease questionnaire (ABDQ).
Results: Of 75 patients enrolled, 4 were excluded due to prior bowel surgery (2) or active C. difficile (2). Patients without active IBD were classified as IBS (n=9), FD (n=7), FD+IBS (n=23), and No DGBI (n=19); 2 had inactive IBD (1 in IBS, 1 in FD+IBS). The IBS group had the greatest mean abdominal pain increase from 0h to 4-24h (2.44 ± 1.13, p=0.01) and the highest overall change from -24 to 4–24h (1.56 ± 1.33, p=0.02). At specific time points, the FD+IBS and FD only group had the highest pain at -24h (3.25 ± 1.65; 3 ± 1.83 p< 0.001) and at 0h (2.29 ± 1.88, 1.14 ± 0.9 p< 0.001). Patients with IBS or FD+IBS showed the highest pain level at 4–24h (p=0.05).
Discussion: Symptom exacerbation after consuming osmotically active contrast was more severe in patients who met DGBI criteria by ABDQ. Differential timing of symptom exacerbation further subtyped the DGBIs, though it was limited by small sample sizes. FD patients showed symptom increase earliest while IBS patients demonstrated delayed symptom exacerbation, suggesting visceral hypersensitivity in the distal GI tract. Those with both had the highest symptom burden, suggesting a potential additive effect. Additional research comparing VH to healthy controls can further clarify the utility of symptom exacerbation with osmotically active solution as a VH biomarker.
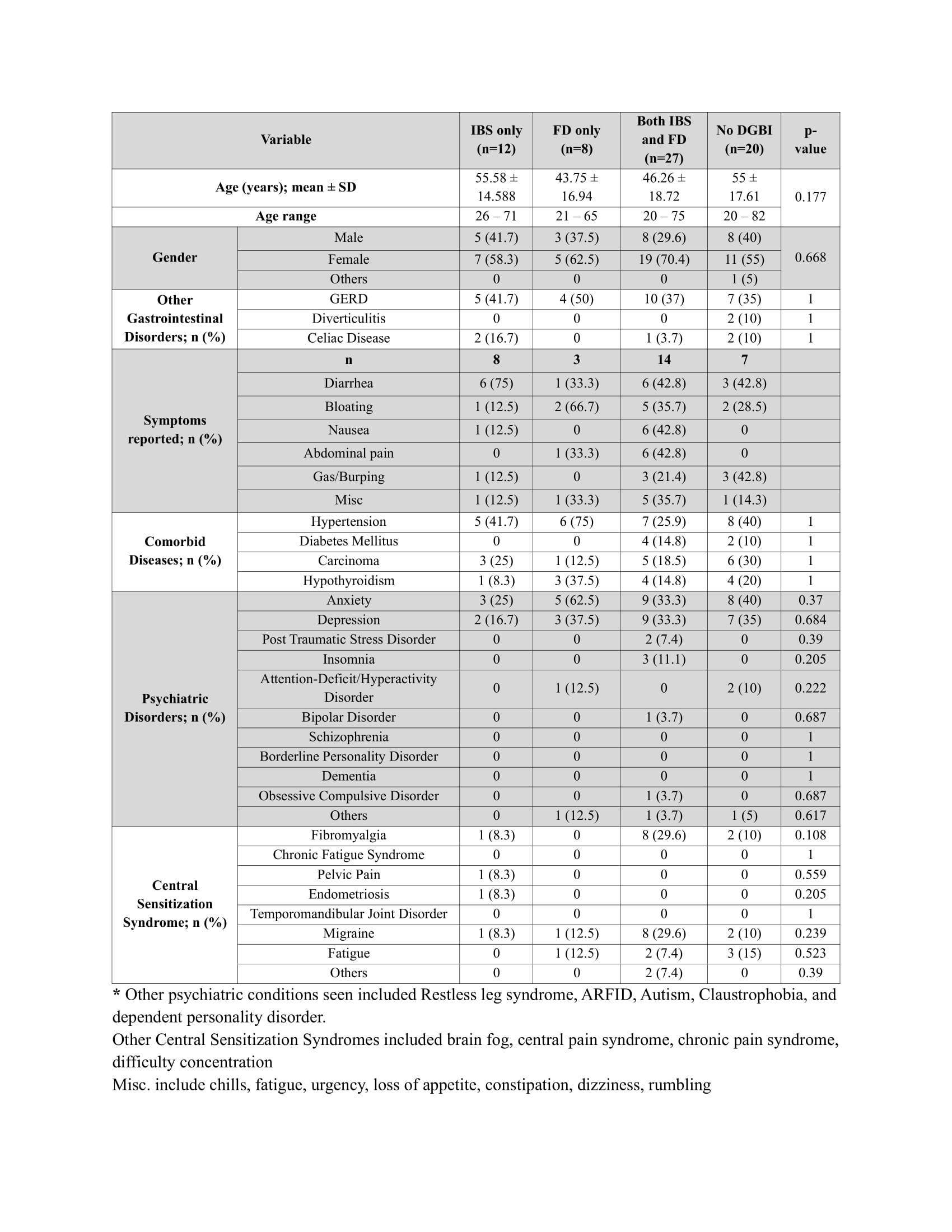
Figure: Demographics of patients undergoing CT enterography

Figure: Graphs representing mean abdominal pain change and mean abdominal pain over time among the subcategories
Disclosures:
Riya Gupta indicated no relevant financial relationships.
David J. Bartlett indicated no relevant financial relationships.
Victor Chedid: Pfizer – Grant/Research Support. Takeda – Consultant.
Moataz Aboeldahb indicated no relevant financial relationships.
Xiao Jing Wang indicated no relevant financial relationships.
Riya Gupta, MBBS1, David J. Bartlett, MD1, Victor Chedid, MD, MSc1, Moataz Aboeldahb, MBBCh2, Xiao Jing Wang, MD1. P0808 - Investigation of Osmotically Active Contrast Solutions in the Quantification of Visceral Hypersensitivity: A Prospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Mayo Clinic College of Medicine and Science, Rochester, MN
Introduction: Visceral hypersensitivity (VH) is a key component of many disorders of gut-brain interaction (DGBIs), including functional dyspepsia (FD) and irritable bowel syndrome (IBS). Existing tests of VH in DGBIs, like rectal or jejunal barostat, are invasive, expensive, and limited to specialized centers. As such, objective diagnosis of VH remains elusive. CT enterography (CTE), used to assess small bowel pathology, utilizes oral, osmotically active mannitol and sorbitol-based agent as neutral contrast timed for small bowel distension and can cause gastrointestinal (GI) symptoms. This study investigates the utility of contrast-induced symptoms as a noninvasive biomarker for VH in DGBIs, particularly in the small bowel.
Methods: A prospective study was conducted at a tertiary care center among patients undergoing CTE for various indications. GI symptom burden was assessed using questionnaires before (–24h), immediately after (0h), and at 4–24h post-CTE. Demographics were extracted from electronic health records. Patients were categorized as IBS, FD, both, or neither (No DBGI) based on a prospectively administered abridged bowel disease questionnaire (ABDQ).
Results: Of 75 patients enrolled, 4 were excluded due to prior bowel surgery (2) or active C. difficile (2). Patients without active IBD were classified as IBS (n=9), FD (n=7), FD+IBS (n=23), and No DGBI (n=19); 2 had inactive IBD (1 in IBS, 1 in FD+IBS). The IBS group had the greatest mean abdominal pain increase from 0h to 4-24h (2.44 ± 1.13, p=0.01) and the highest overall change from -24 to 4–24h (1.56 ± 1.33, p=0.02). At specific time points, the FD+IBS and FD only group had the highest pain at -24h (3.25 ± 1.65; 3 ± 1.83 p< 0.001) and at 0h (2.29 ± 1.88, 1.14 ± 0.9 p< 0.001). Patients with IBS or FD+IBS showed the highest pain level at 4–24h (p=0.05).
Discussion: Symptom exacerbation after consuming osmotically active contrast was more severe in patients who met DGBI criteria by ABDQ. Differential timing of symptom exacerbation further subtyped the DGBIs, though it was limited by small sample sizes. FD patients showed symptom increase earliest while IBS patients demonstrated delayed symptom exacerbation, suggesting visceral hypersensitivity in the distal GI tract. Those with both had the highest symptom burden, suggesting a potential additive effect. Additional research comparing VH to healthy controls can further clarify the utility of symptom exacerbation with osmotically active solution as a VH biomarker.
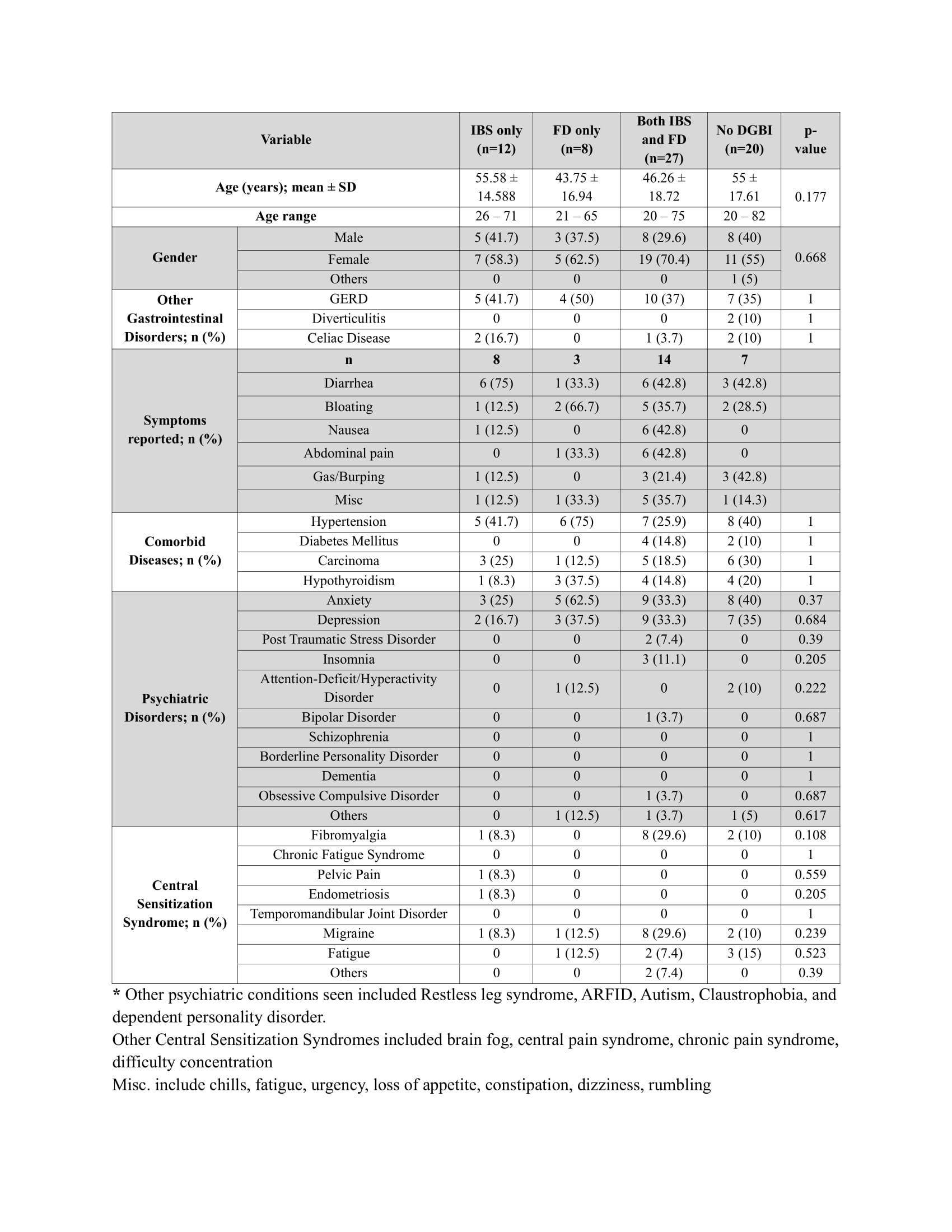
Figure: Demographics of patients undergoing CT enterography

Figure: Graphs representing mean abdominal pain change and mean abdominal pain over time among the subcategories
Disclosures:
Riya Gupta indicated no relevant financial relationships.
David J. Bartlett indicated no relevant financial relationships.
Victor Chedid: Pfizer – Grant/Research Support. Takeda – Consultant.
Moataz Aboeldahb indicated no relevant financial relationships.
Xiao Jing Wang indicated no relevant financial relationships.
Riya Gupta, MBBS1, David J. Bartlett, MD1, Victor Chedid, MD, MSc1, Moataz Aboeldahb, MBBCh2, Xiao Jing Wang, MD1. P0808 - Investigation of Osmotically Active Contrast Solutions in the Quantification of Visceral Hypersensitivity: A Prospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

