Sunday Poster Session
Category: Functional Bowel Disease
P0799 - Hypermobility Spectrum Disorders and Fundic Accommodation as Assessed by Intragastric Meal Distribution
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- PS
Priyanka Shah, MD
Lewis Katz School of Medicine at Temple University
Philadelphia, PA
Presenting Author(s)
Priyanka Shah, MD1, Alan H. Maurer, MD, MS1, Henry P.. Parkman, MD, FACG2
1Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 2Temple University Hospital, Philadelphia, PA
Introduction: Patients with hypermobility spectrum disorders (HSD) often experience severe GI symptoms, including reflux and bloating. The etiology of these symptoms is unclear. However, one possible explanation is abnormal fundic accommodation in patients with HSD. In this study, we compare both GI symptom severity and intragastric meal distribution on gastric emptying scintigraphy (GES) between patients with and without HSD to evaluate for a possible connection between HSD and fundic accommodation.
Methods: Patients undergoing evaluation for gastroparesis completed the Patient Assessment of Gastrointestinal Disorders-Symptom Severity Index (PAGI-SYM) to grade symptom severity. They also underwent GES; measurements of percentage of meal retained were taken at 0, 30, 60, 120, 180, and 240 minutes. Patients who did not eat at least 90% of the standard meal were excluded. In addition to GES, intragastric meal distribution was assessed using proximal/total and proximal/distal count ratios. Symptom severity and count ratios were compared between HSD and non-HSD patients via Welch’s t-test. A p-value < 0.05 was considered significant.
Results: 58 patients with accessible GES were undergoing evaluation for gastroparesis. 11 had HSD (H+) and 47 did not (H-). H+ had significantly more severe symptoms in the postprandial fullness/early satiety subscale (4.14±0.83 vs. 3.41±1.21, p = 0.027) and the Gastroparesis Cardinal Symptoms Index (3.53±0.74 vs. 2.93±1.01, p = 0.035) (Table 1). The mean proximal/total and proximal/distal ratios at all time marks in H+ were lower than H-. The proximal/distal ratio was significantly lower in H+ at the 30, 60, and 240 minute time marks compared to H- (2.34±1.09, 1.94±0.64, 0.64±0.24 vs. 3.55±2.85, 2.92±2.85, 0.90±0.56, p = 0.027, 0.037, and 0.024, respectively) (Figure 1).
Discussion: Patients with HSD had significantly more severe early satiety/postprandial fullness symptoms. They also had smaller amounts of the meal in the proximal stomach as determined by the analysis of intragastric meal distribution; this suggests impaired fundic accommodation with greater transit from the fundus toward the distal stomach. These results support the hypothesis that the increased severity of GI symptoms in patients with HSD, specifically in the early satiety/postprandial fullness subscale, is associated with impaired fundic accommodation. Future studies focused on enhancing fundic accommodation in HSD patients should be pursued in order to improve their GI symptoms.
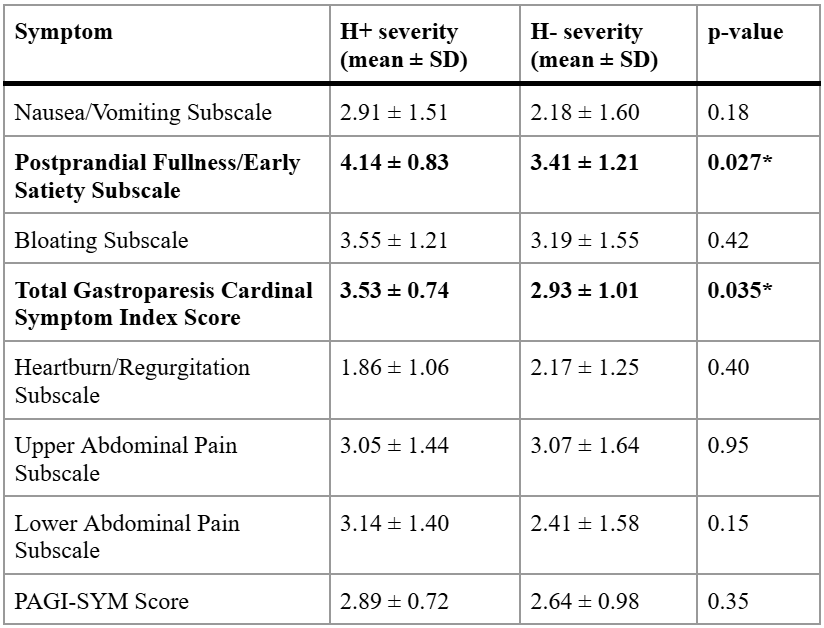
Figure: Table 1: Symptom severities for the PAGI-SYM subscales for patients with and without HSD. p-values using Welch's t-test for analysis of differences between the groups are shown.
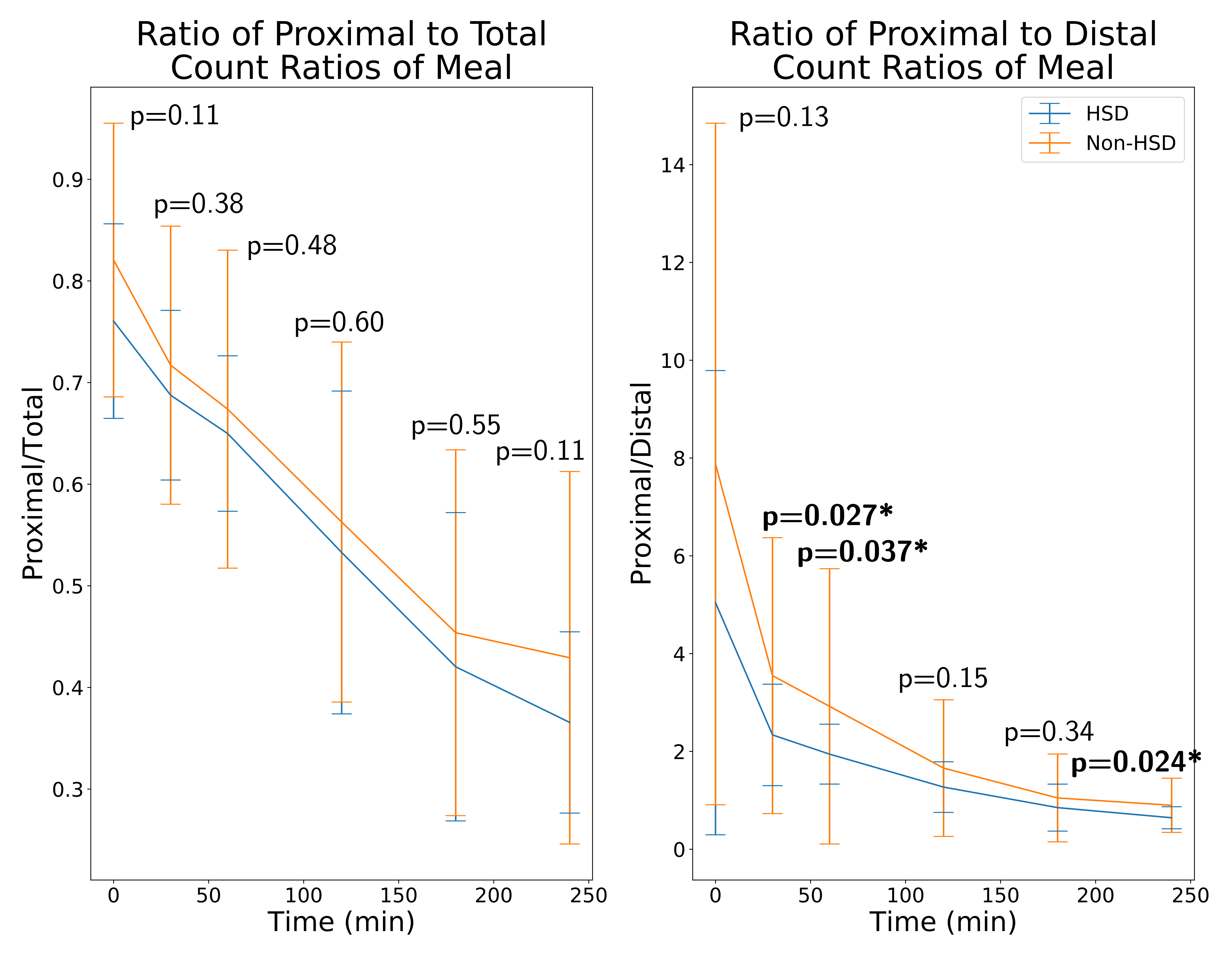
Figure: Figure 1: Ratios of proximal to total and proximal to distal intragastric count ratios over time for patients with and without HSD. Error bars indicate standard deviations, and p-values indicate significance via t-test.
Disclosures:
Priyanka Shah indicated no relevant financial relationships.
Alan Maurer indicated no relevant financial relationships.
Henry Parkman indicated no relevant financial relationships.
Priyanka Shah, MD1, Alan H. Maurer, MD, MS1, Henry P.. Parkman, MD, FACG2. P0799 - Hypermobility Spectrum Disorders and Fundic Accommodation as Assessed by Intragastric Meal Distribution, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 2Temple University Hospital, Philadelphia, PA
Introduction: Patients with hypermobility spectrum disorders (HSD) often experience severe GI symptoms, including reflux and bloating. The etiology of these symptoms is unclear. However, one possible explanation is abnormal fundic accommodation in patients with HSD. In this study, we compare both GI symptom severity and intragastric meal distribution on gastric emptying scintigraphy (GES) between patients with and without HSD to evaluate for a possible connection between HSD and fundic accommodation.
Methods: Patients undergoing evaluation for gastroparesis completed the Patient Assessment of Gastrointestinal Disorders-Symptom Severity Index (PAGI-SYM) to grade symptom severity. They also underwent GES; measurements of percentage of meal retained were taken at 0, 30, 60, 120, 180, and 240 minutes. Patients who did not eat at least 90% of the standard meal were excluded. In addition to GES, intragastric meal distribution was assessed using proximal/total and proximal/distal count ratios. Symptom severity and count ratios were compared between HSD and non-HSD patients via Welch’s t-test. A p-value < 0.05 was considered significant.
Results: 58 patients with accessible GES were undergoing evaluation for gastroparesis. 11 had HSD (H+) and 47 did not (H-). H+ had significantly more severe symptoms in the postprandial fullness/early satiety subscale (4.14±0.83 vs. 3.41±1.21, p = 0.027) and the Gastroparesis Cardinal Symptoms Index (3.53±0.74 vs. 2.93±1.01, p = 0.035) (Table 1). The mean proximal/total and proximal/distal ratios at all time marks in H+ were lower than H-. The proximal/distal ratio was significantly lower in H+ at the 30, 60, and 240 minute time marks compared to H- (2.34±1.09, 1.94±0.64, 0.64±0.24 vs. 3.55±2.85, 2.92±2.85, 0.90±0.56, p = 0.027, 0.037, and 0.024, respectively) (Figure 1).
Discussion: Patients with HSD had significantly more severe early satiety/postprandial fullness symptoms. They also had smaller amounts of the meal in the proximal stomach as determined by the analysis of intragastric meal distribution; this suggests impaired fundic accommodation with greater transit from the fundus toward the distal stomach. These results support the hypothesis that the increased severity of GI symptoms in patients with HSD, specifically in the early satiety/postprandial fullness subscale, is associated with impaired fundic accommodation. Future studies focused on enhancing fundic accommodation in HSD patients should be pursued in order to improve their GI symptoms.
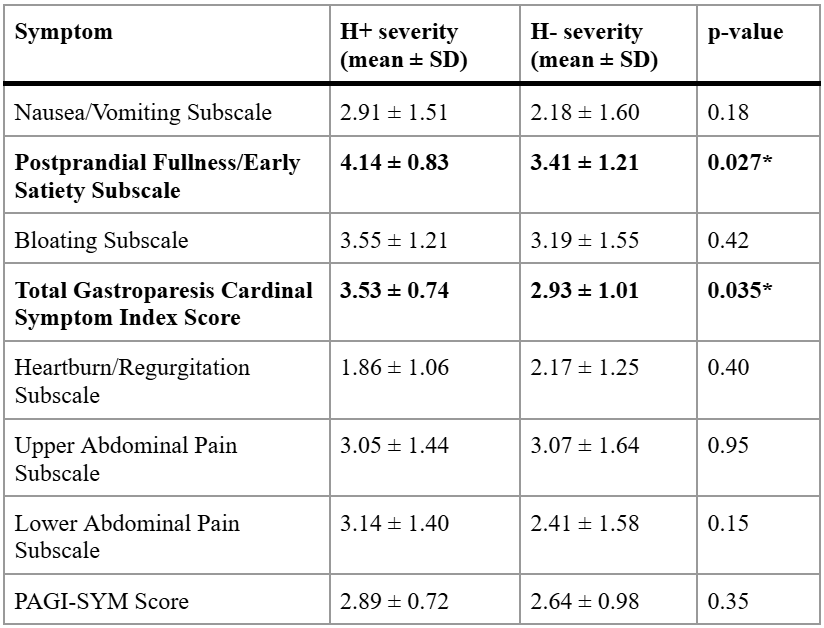
Figure: Table 1: Symptom severities for the PAGI-SYM subscales for patients with and without HSD. p-values using Welch's t-test for analysis of differences between the groups are shown.
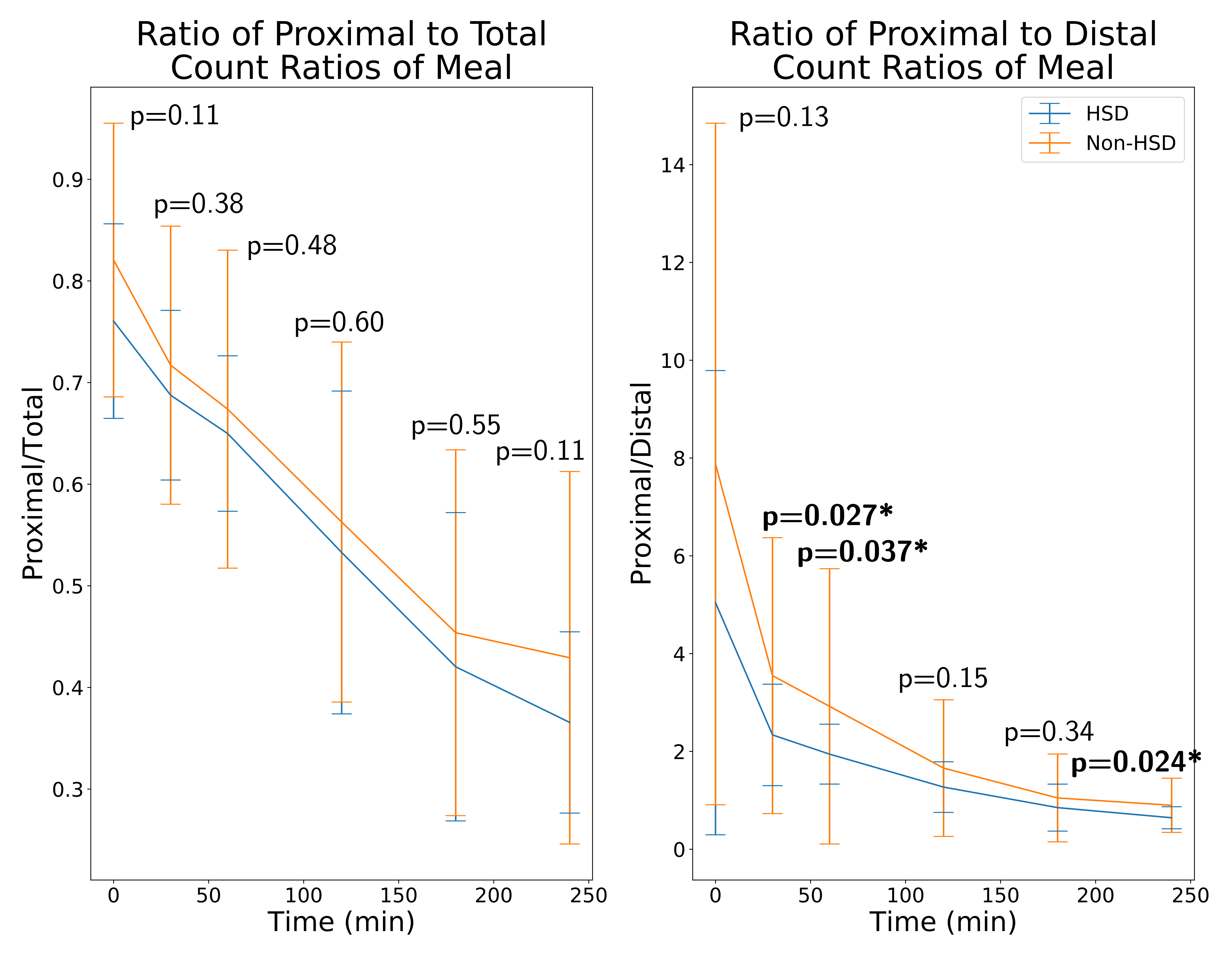
Figure: Figure 1: Ratios of proximal to total and proximal to distal intragastric count ratios over time for patients with and without HSD. Error bars indicate standard deviations, and p-values indicate significance via t-test.
Disclosures:
Priyanka Shah indicated no relevant financial relationships.
Alan Maurer indicated no relevant financial relationships.
Henry Parkman indicated no relevant financial relationships.
Priyanka Shah, MD1, Alan H. Maurer, MD, MS1, Henry P.. Parkman, MD, FACG2. P0799 - Hypermobility Spectrum Disorders and Fundic Accommodation as Assessed by Intragastric Meal Distribution, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
