Sunday Poster Session
Category: Esophagus
P0757 - Acute Esophageal Necrosis: Black Esophagus
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AT
Asli Tahan (she/her/hers)
University of Missouri
Presenting Author(s)
Ervin Tahan, 1, Asli Tahan, 1, Muhammad F.. Mubarak, MBBS2
1University of Missouri, Columbia, MO; 2King Saud University, Los Angeles, CA
Introduction: Across many medical disciplines, the word “necrosis” imbues a sense of urgency and highlights the gravity of a patient’s medical condition. From necrotizing fasciitis to necrotizing enterocolitis in infants, to osteonecrosis of the jaw, to acute esophageal necrosis(AEN), the rapid autolysis of various tissues is an ominous sign in these patients. Mortality from AEN, commonly known as “black esophagus”, is nearly 32%. It predominantly affects males 4 times more often than females and is usually a result of hypoperfusion or ischemia. Diagnosis is made endoscopically with the assistance of computed tomography(CT) scan and pathology. We present a rare condition of AEN that was diagnosed with esophagogastroduodenoscopy(EGD).
Case Description/
Methods: A 60-year-old male with past medical history of hypertension, type-2 diabetes, coronary artery disease(CAD), and gastroesophageal reflux disease presented with coffee ground emesis and melena. His symptoms started with nausea 2 days before the admission. He reported heavy alcohol use in the past but admitted to 2 drinks nightly on average. Vitals on admission were heart rate:110/min, blood pressure:85/50mmHg, WBC:18,500/mm3, Hb:12g/dl, platelets:210,000/mm3, lactate:18mmol/L, and INR:1.1. He was fluid resuscitated, started on proton pump inhibitor IV therapy and once stabilized, an EGD was performed, which showed an AEN from the level of the cricopharyngeal muscle to gastroesophageal junction(GEJ). For concerns of vascular ischemia, a CT-angiography was obtained but did not reveal vascular pathology.
Discussion: At first glance, this patient presented typical signs of upper GI bleeding. However, EGD led to diagnosis of a rare condition of AEN. 90% of the time, AEN can present with melena or hematemesis and can be accompanied by syncope, fever, abdominal pain and nausea. Endoscopically, the esophageal mucosa had a circumferential black color which immediately terminated at the GEJ, usually indicative of a vascular compromise. Due to its anatomical location and vascular supply, distal esophagus is prone to be a ‘watershed’ region. This patient had risk factors for ischemic conditions such as history of CAD, hypertension, and diabetes along with septic presentation and low flow state due to acute blood loss. In such cases, while AEN might not be the first differential diagnosis for melena, index of suspicion should be in the differential and the supportive care as well as treating the underlying causes are important in management.
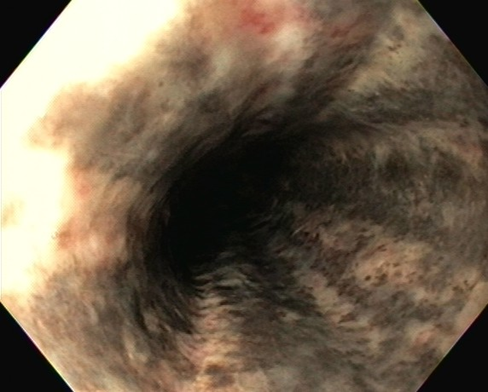
Figure: Picture 1: Acute esophageal necrosis: black esophagus endoscopic appearance
Disclosures:
Ervin Tahan indicated no relevant financial relationships.
Asli Tahan indicated no relevant financial relationships.
Muhammad Mubarak indicated no relevant financial relationships.
Ervin Tahan, 1, Asli Tahan, 1, Muhammad F.. Mubarak, MBBS2. P0757 - Acute Esophageal Necrosis: Black Esophagus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri, Columbia, MO; 2King Saud University, Los Angeles, CA
Introduction: Across many medical disciplines, the word “necrosis” imbues a sense of urgency and highlights the gravity of a patient’s medical condition. From necrotizing fasciitis to necrotizing enterocolitis in infants, to osteonecrosis of the jaw, to acute esophageal necrosis(AEN), the rapid autolysis of various tissues is an ominous sign in these patients. Mortality from AEN, commonly known as “black esophagus”, is nearly 32%. It predominantly affects males 4 times more often than females and is usually a result of hypoperfusion or ischemia. Diagnosis is made endoscopically with the assistance of computed tomography(CT) scan and pathology. We present a rare condition of AEN that was diagnosed with esophagogastroduodenoscopy(EGD).
Case Description/
Methods: A 60-year-old male with past medical history of hypertension, type-2 diabetes, coronary artery disease(CAD), and gastroesophageal reflux disease presented with coffee ground emesis and melena. His symptoms started with nausea 2 days before the admission. He reported heavy alcohol use in the past but admitted to 2 drinks nightly on average. Vitals on admission were heart rate:110/min, blood pressure:85/50mmHg, WBC:18,500/mm3, Hb:12g/dl, platelets:210,000/mm3, lactate:18mmol/L, and INR:1.1. He was fluid resuscitated, started on proton pump inhibitor IV therapy and once stabilized, an EGD was performed, which showed an AEN from the level of the cricopharyngeal muscle to gastroesophageal junction(GEJ). For concerns of vascular ischemia, a CT-angiography was obtained but did not reveal vascular pathology.
Discussion: At first glance, this patient presented typical signs of upper GI bleeding. However, EGD led to diagnosis of a rare condition of AEN. 90% of the time, AEN can present with melena or hematemesis and can be accompanied by syncope, fever, abdominal pain and nausea. Endoscopically, the esophageal mucosa had a circumferential black color which immediately terminated at the GEJ, usually indicative of a vascular compromise. Due to its anatomical location and vascular supply, distal esophagus is prone to be a ‘watershed’ region. This patient had risk factors for ischemic conditions such as history of CAD, hypertension, and diabetes along with septic presentation and low flow state due to acute blood loss. In such cases, while AEN might not be the first differential diagnosis for melena, index of suspicion should be in the differential and the supportive care as well as treating the underlying causes are important in management.
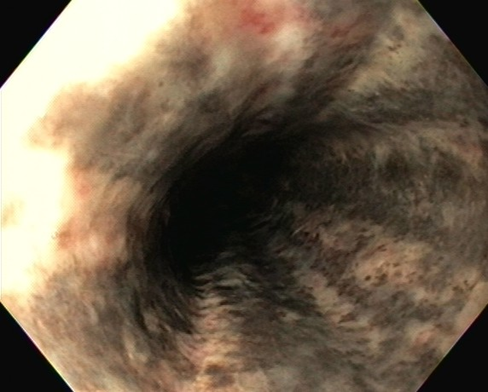
Figure: Picture 1: Acute esophageal necrosis: black esophagus endoscopic appearance
Disclosures:
Ervin Tahan indicated no relevant financial relationships.
Asli Tahan indicated no relevant financial relationships.
Muhammad Mubarak indicated no relevant financial relationships.
Ervin Tahan, 1, Asli Tahan, 1, Muhammad F.. Mubarak, MBBS2. P0757 - Acute Esophageal Necrosis: Black Esophagus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
