Sunday Poster Session
Category: Esophagus
P0755 - The Vanishing Esophagus: A Case of Acute Esophageal Necrosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- RG
Rodney A. A. George-Rivera, MD (he/him/his)
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Rodney A. George-Rivera, MD, Bianca Goyco-Cortes, MD, Jose Martin-Ortiz, MD, FACG, Orlando Rodriguez-Amador, MD
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Acute Esophageal Necrosis (AEN) is a rare entity and medical emergency with an incidence of 0.01-0.28%. The 2-hit hypothesis for AEN proposes that two events, an initial low-flow vascular state followed by a secondary injury, contribute to the development of this condition.
Case Description/
Methods: Case of a 70-year-old man former smoker with medical history of hypertension, atrial fibrillation and coronary artery disease who presented to the emergency department after 4 days of blood-streaked oral secretions associated to epigastric discomfort. Examination showed bradycardia and epigastric tenderness. Blood work was remarkable for lactatemia. Hemoglobin levels were within patient`s baseline and there was no elevation on BUN to Creatinine ratio. CT of the abdomen and pelvis with IV and oral contrast showed thickening of distal esophagus. Patient was started on high dose PPI and evaluated by the GI Inpatient team. Upper endoscopy revealed severe deep ulceration of the mid to distal esophagus with friable mucosa and some necrotic tissue. Gastroesophageal junction was spared. Endoscopic findings were consistent with acute esophageal necrosis. During admission medication for rate control was optimized with resolution of bradycardia. He was discharged home with high dose PPI for 8 weeks. After completion of therapy, a follow up upper endoscopy revealed normal esophageal mucosa with complete resolution of necrotic esophagitis.
Discussion: In this case, AEN is suspected to be secondary to a decrease in esophageal perfusion caused by hemodynamic compromised in a patient with risk factors for vascular disease. Despite no biopsy proved diagnosis, endoscopic findings including inflammation in distal esophagus with the sparing of the gastroesophageal junction supports the diagnosis of esophageal ischemia in this patient. It is important to suspect and recognize this condition as a possible etiology of gastrointestinal bleeding since it is a rare cause that carries a high mortality rate.
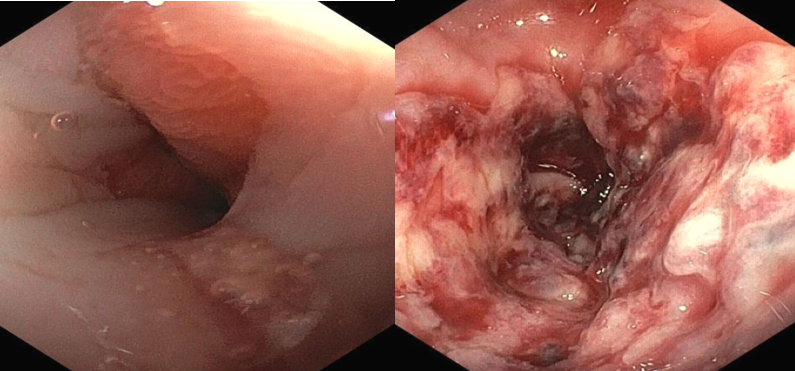
Figure: Figure 1. Gastroesophageal junction (left) and lower esophagus (right) at presentation.
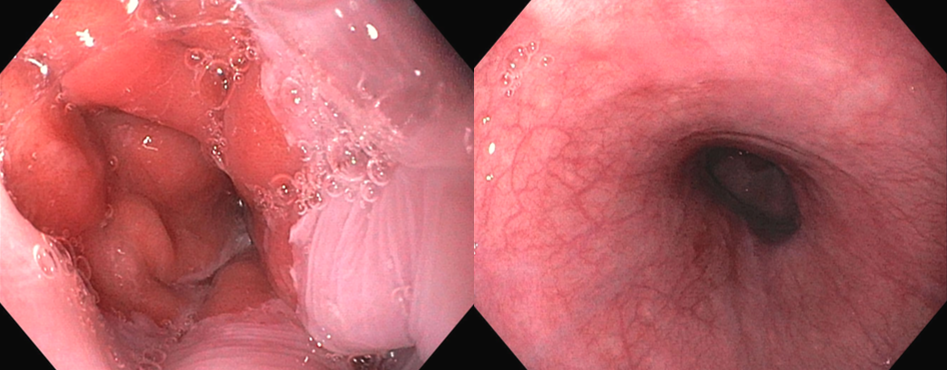
Figure: Figure 2. Gastroesophageal junction (left) and lower esophagus (right) after 8 weeks of PPI.
Disclosures:
Rodney George-Rivera indicated no relevant financial relationships.
Bianca Goyco-Cortes indicated no relevant financial relationships.
Jose Martin-Ortiz indicated no relevant financial relationships.
Orlando Rodriguez-Amador indicated no relevant financial relationships.
Rodney A. George-Rivera, MD, Bianca Goyco-Cortes, MD, Jose Martin-Ortiz, MD, FACG, Orlando Rodriguez-Amador, MD. P0755 - The Vanishing Esophagus: A Case of Acute Esophageal Necrosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Acute Esophageal Necrosis (AEN) is a rare entity and medical emergency with an incidence of 0.01-0.28%. The 2-hit hypothesis for AEN proposes that two events, an initial low-flow vascular state followed by a secondary injury, contribute to the development of this condition.
Case Description/
Methods: Case of a 70-year-old man former smoker with medical history of hypertension, atrial fibrillation and coronary artery disease who presented to the emergency department after 4 days of blood-streaked oral secretions associated to epigastric discomfort. Examination showed bradycardia and epigastric tenderness. Blood work was remarkable for lactatemia. Hemoglobin levels were within patient`s baseline and there was no elevation on BUN to Creatinine ratio. CT of the abdomen and pelvis with IV and oral contrast showed thickening of distal esophagus. Patient was started on high dose PPI and evaluated by the GI Inpatient team. Upper endoscopy revealed severe deep ulceration of the mid to distal esophagus with friable mucosa and some necrotic tissue. Gastroesophageal junction was spared. Endoscopic findings were consistent with acute esophageal necrosis. During admission medication for rate control was optimized with resolution of bradycardia. He was discharged home with high dose PPI for 8 weeks. After completion of therapy, a follow up upper endoscopy revealed normal esophageal mucosa with complete resolution of necrotic esophagitis.
Discussion: In this case, AEN is suspected to be secondary to a decrease in esophageal perfusion caused by hemodynamic compromised in a patient with risk factors for vascular disease. Despite no biopsy proved diagnosis, endoscopic findings including inflammation in distal esophagus with the sparing of the gastroesophageal junction supports the diagnosis of esophageal ischemia in this patient. It is important to suspect and recognize this condition as a possible etiology of gastrointestinal bleeding since it is a rare cause that carries a high mortality rate.
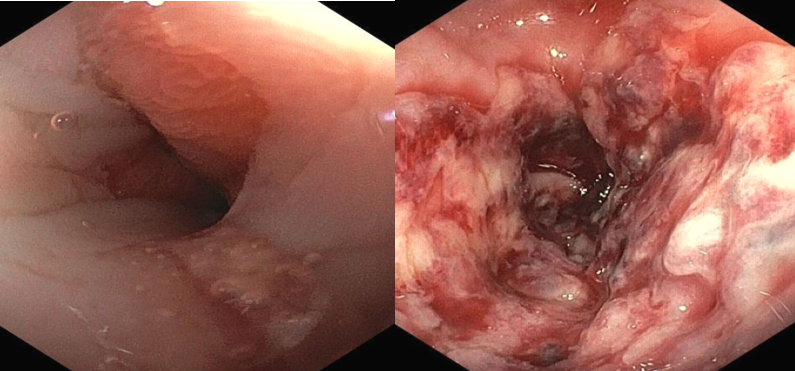
Figure: Figure 1. Gastroesophageal junction (left) and lower esophagus (right) at presentation.
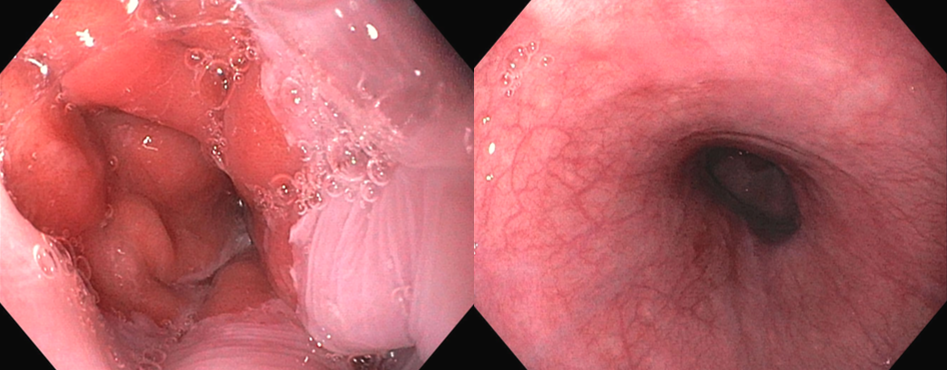
Figure: Figure 2. Gastroesophageal junction (left) and lower esophagus (right) after 8 weeks of PPI.
Disclosures:
Rodney George-Rivera indicated no relevant financial relationships.
Bianca Goyco-Cortes indicated no relevant financial relationships.
Jose Martin-Ortiz indicated no relevant financial relationships.
Orlando Rodriguez-Amador indicated no relevant financial relationships.
Rodney A. George-Rivera, MD, Bianca Goyco-Cortes, MD, Jose Martin-Ortiz, MD, FACG, Orlando Rodriguez-Amador, MD. P0755 - The Vanishing Esophagus: A Case of Acute Esophageal Necrosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
