Sunday Poster Session
Category: Esophagus
P0754 - Beyond the Usual Suspects: Acute Esophageal Necrosis in a 48-Year-Old With Alcohol Use Disorder
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JJ
Joseph Jones, MD
United Health Services, Wilson Medical Center
Johnson City, NY
Presenting Author(s)
Joseph Jones, MD1, Khandokar A. Talib, MD2, Ahmed Shehadah, MD3, Amanke Oranu, MD3, Toseef Javaid, MD1
1United Health Services, Wilson Medical Center, Johnson City, NY; 2United Health Services, Wilson Medical Center, Vestal, NY; 3United Health Services, Wilson Medical Center, Binghamton, NY
Introduction: Acute esophageal necrosis (AEN), also known as “black esophagus,” is a rare condition with an endoscopic prevalence of 0.01–0.28%. It is characterized by circumferential black discoloration of the esophageal mucosa. AEN predominantly affects older males (mean age 68) and is associated with poor nutritional status, alcohol use, and multiple comorbidities. Hematemesis and melena are the most common presenting symptoms, though diagnosis is often incidental during EGD. Although typically self-limited with supportive care, AEN carries a high mortality rate (13–35%), often related to underlying disease, with direct complications, including perforation, stricture, and severe hemorrhage, accounting for a smaller subset.
Case Description/
Methods: A 48-year-old male with a history of alcohol use disorder presented after a witnessed seizure. He reported daily alcohol consumption and poor nutrition. Vitals revealed tachycardia, and labs showed severe hyponatremia and elevated lactate. Ethanol level was undetectable. Hypertonic saline was administered with a central line. Subsequently, he developed new-onset atrial fibrillation with rapid ventricular response and hypotension, treated with digoxin and enoxaparin. The patient then had hematemesis, which he later disclosed had occurred intermittently for one week. His hemoglobin dropped from 14.0 g/dL to 10.2 g/dL within eight hours, and he developed melena. Management included pantoprazole, octreotide, and a massive transfusion protocol. Esophagogastroduodenoscopy (EGD) revealed diffuse circumferential black discoloration and ulceration throughout the esophagus, consistent with AEN [Figure 1]. Gastric and duodenal mucosa appeared normal. The patient was managed with nil per os (NPO) status and intravenous proton pump inhibitor therapy, before gradually resuming oral intake. He was discharged in stable condition to a substance use rehabilitation facility after nine days.
Discussion: Acute esophageal necrosis is a rare condition that typically affects older male patients with multiple medical comorbidities, making this an atypical presentation in a young adult whose medical history is significant only for alcohol use disorder. Furthermore, while acute esophageal necrosis often presents with upper gastrointestinal bleeding, severe bleeding complications—such as those exhibited by this patient requiring massive transfusion—are rare. Early recognition and aggressive supportive care are essential for favorable outcomes.
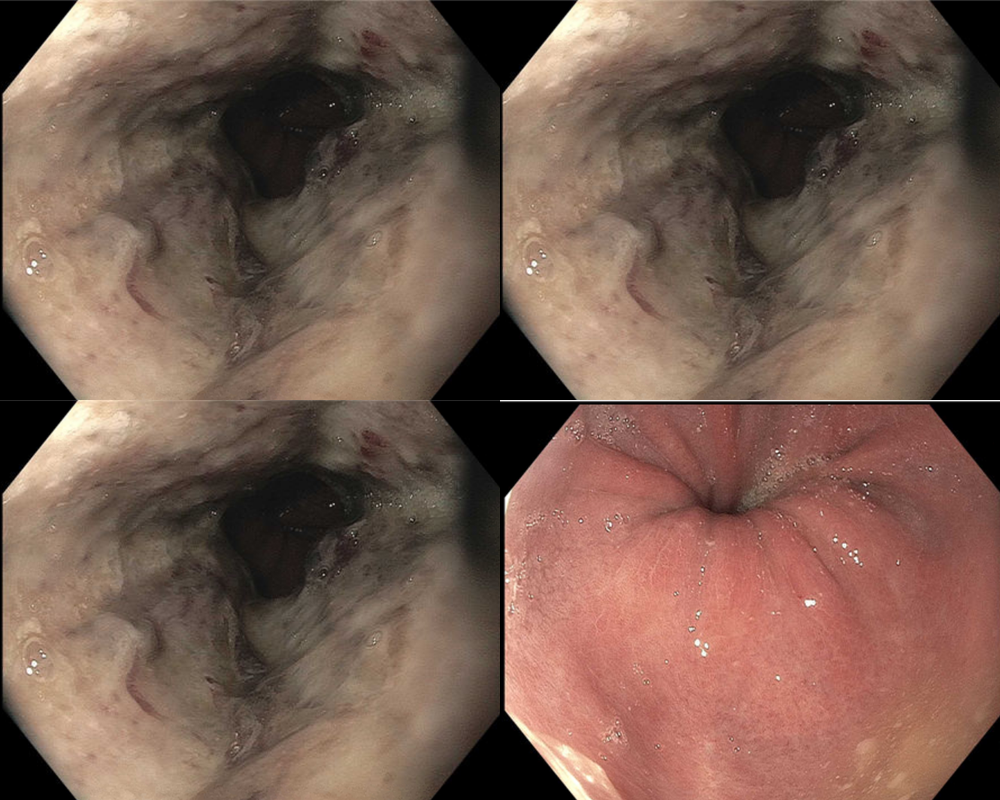
Figure: Figure 1: Diffuse circumferential black discoloration and ulceration throughout the esophagus.
Disclosures:
Joseph Jones indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Joseph Jones, MD1, Khandokar A. Talib, MD2, Ahmed Shehadah, MD3, Amanke Oranu, MD3, Toseef Javaid, MD1. P0754 - Beyond the Usual Suspects: Acute Esophageal Necrosis in a 48-Year-Old With Alcohol Use Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1United Health Services, Wilson Medical Center, Johnson City, NY; 2United Health Services, Wilson Medical Center, Vestal, NY; 3United Health Services, Wilson Medical Center, Binghamton, NY
Introduction: Acute esophageal necrosis (AEN), also known as “black esophagus,” is a rare condition with an endoscopic prevalence of 0.01–0.28%. It is characterized by circumferential black discoloration of the esophageal mucosa. AEN predominantly affects older males (mean age 68) and is associated with poor nutritional status, alcohol use, and multiple comorbidities. Hematemesis and melena are the most common presenting symptoms, though diagnosis is often incidental during EGD. Although typically self-limited with supportive care, AEN carries a high mortality rate (13–35%), often related to underlying disease, with direct complications, including perforation, stricture, and severe hemorrhage, accounting for a smaller subset.
Case Description/
Methods: A 48-year-old male with a history of alcohol use disorder presented after a witnessed seizure. He reported daily alcohol consumption and poor nutrition. Vitals revealed tachycardia, and labs showed severe hyponatremia and elevated lactate. Ethanol level was undetectable. Hypertonic saline was administered with a central line. Subsequently, he developed new-onset atrial fibrillation with rapid ventricular response and hypotension, treated with digoxin and enoxaparin. The patient then had hematemesis, which he later disclosed had occurred intermittently for one week. His hemoglobin dropped from 14.0 g/dL to 10.2 g/dL within eight hours, and he developed melena. Management included pantoprazole, octreotide, and a massive transfusion protocol. Esophagogastroduodenoscopy (EGD) revealed diffuse circumferential black discoloration and ulceration throughout the esophagus, consistent with AEN [Figure 1]. Gastric and duodenal mucosa appeared normal. The patient was managed with nil per os (NPO) status and intravenous proton pump inhibitor therapy, before gradually resuming oral intake. He was discharged in stable condition to a substance use rehabilitation facility after nine days.
Discussion: Acute esophageal necrosis is a rare condition that typically affects older male patients with multiple medical comorbidities, making this an atypical presentation in a young adult whose medical history is significant only for alcohol use disorder. Furthermore, while acute esophageal necrosis often presents with upper gastrointestinal bleeding, severe bleeding complications—such as those exhibited by this patient requiring massive transfusion—are rare. Early recognition and aggressive supportive care are essential for favorable outcomes.
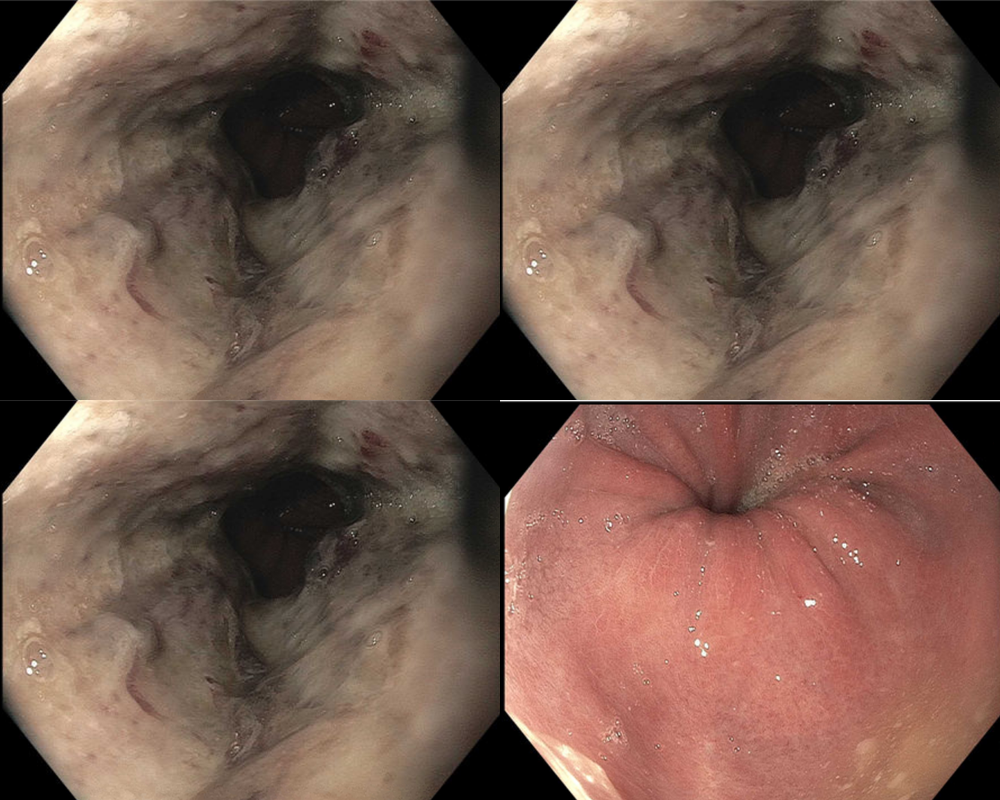
Figure: Figure 1: Diffuse circumferential black discoloration and ulceration throughout the esophagus.
Disclosures:
Joseph Jones indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Joseph Jones, MD1, Khandokar A. Talib, MD2, Ahmed Shehadah, MD3, Amanke Oranu, MD3, Toseef Javaid, MD1. P0754 - Beyond the Usual Suspects: Acute Esophageal Necrosis in a 48-Year-Old With Alcohol Use Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
